Editors' note: Given the speed and intensity of the activity surrounding the current Covid‐19 epidemic, we wanted to bring the dispatch below, from the faculty at Boston University Medical Center, to the attention of the neurology community. We realize that many other institutions are undertaking similar projects (e.g., this site from Brigham and Women's Hospital, https://covidprotocols.org/protocols/11-neurology/, but for those who are not yet aware of them, we wanted to make sure that these sources of information were broadly recognized and available to neurologists. Martin A. Samuels, MD and Clifford B. Saper, MD, PhD.
Introduction
In response to the coronavirus disease 2019 (COVID‐19) pandemic, the scientific community has made great efforts to accelerate its process for knowledge synthesis and dissemination, including expedited journal peer review,1 open source platforms for quick review of preprints,2 removal of paywalls from COVID‐19–related publications,3 specialty article collections,4 and rapidly produced consensus statements by academic societies.5 Due to the need for urgent guidance on disease management within different specialties, there has been an emergence of ad hoc task forces that curate and synthesize information, sharing recommendations publicly, with frequent updates as new evidence becomes available.3 This editorial details our experience creating and disseminating protocols for the management of neurological disorders in hospitalized patients with COVID‐19, based on frequent evaluation of available evidence and supplemented by expert opinion.
Shortly after the World Health Organization (WHO) declared the pandemic status of COVID‐19 on March 11, 2020, we noted that there was no consolidated source of information on the management of neurology inpatients with COVID‐19, in contrast to guidance on outpatient management detailed in protocols published by the Association of British Neurologists.6 At the time, there were early reports of acute cerebrovascular disease, encephalopathy, and headaches,7, 8 among other neurological conditions secondary to the virus. We aimed to address this gap by establishing an intrainstitutional task force to develop and share protocols for the management of these conditions.
At the time of this writing, Massachusetts has the third‐highest caseload of COVID‐19 in the United States. Our institution has seen a disproportionate number of cases in Boston, reflecting the vulnerable population we serve as a safety net hospital. As we experienced an early surge, we feel well positioned to share our protocols partially guided by our experiences as frontline clinicians, which may be useful for institutions in regions lagging ours in the trajectory of the pandemic or in the event of a second surge.
Development
On March 20, 9 days after pandemic status was declared by the WHO, we created a task force of 15 neurologists representing 6 subspecialties at our institution. The group agreed on 4 principles to guide the development of the protocols: (1) prioritization of evidence over expert opinion whenever possible, (2) balance of generalizability to account for interinstitutional differences and sufficient detail for practicality, (3) frequent updates based on emerging literature and accumulating frontline clinical experience, and (4) methodical collaboration between group members and with peers in the scientific community.
Over a 2‐week period, task force members developed management protocols according to their subspecialty expertise and uploaded them to a shared document. These protocols summarized the existing literature on neurological complications of COVID‐19 and detailed practical management considerations, including strategies for conserving personal protective equipment and minimizing health care worker exposure. The online document hosted the most current version of each protocol alongside open bullet points, which group members populated with suggestions and critique. All sections were finalized on April 1 and reviewed by senior clinicians. Team members agreed to submit weekly updates and revisions ad hoc based on new information in the literature or firsthand clinical experience.
Dissemination
With the approval of the hospital chief medical officer, we created a site external to the hospital and medical school web domains to host the protocols, to promote their generalizability beyond our institution. On April 3, 2 weeks after establishing the task force, we published the protocols at covidneurology.org.9 Within the first 72 hours of publication, the website was promoted on the Synapse American Academy of Neurology Online Communities and on social media.
Data Analytics
Viewership analytics data were initially collected using the open source log file analyzer Awstats and replaced by Google Analytics on April 13. At the time of this writing (May 4, 2020), there have been 14,463 total page views according to web domain analytics. Over one arbitrary week from April 14 to April 20, which reflects a week of “normal” usage set >10 days after initial dissemination and promotion, there were 465 unique visitors to the site over 588 sessions. The median number of daily unique visitors was 84 (range = 48–119).
The site has been accessed in 55 countries, with the greatest proportion of unique visitors from the USA (52%), followed by the Philippines (14%) and Saudi Arabia (12%; Fig. 1A). Within the USA, the site has been accessed in 46 states, with the greatest proportion of unique visitors from Massachusetts (22%), followed by Virginia (12%) and California (9%; see Fig. 1B). The section most frequently visited was “Ischemic Stroke” (24%), followed by “Seizures and Electroencephalography” (14%) and “Introduction” (12%). The website was accessed on a mobile device in 62% of all sessions, via desktop computer in 36%, and by tablet in 1%.
Figure 1.
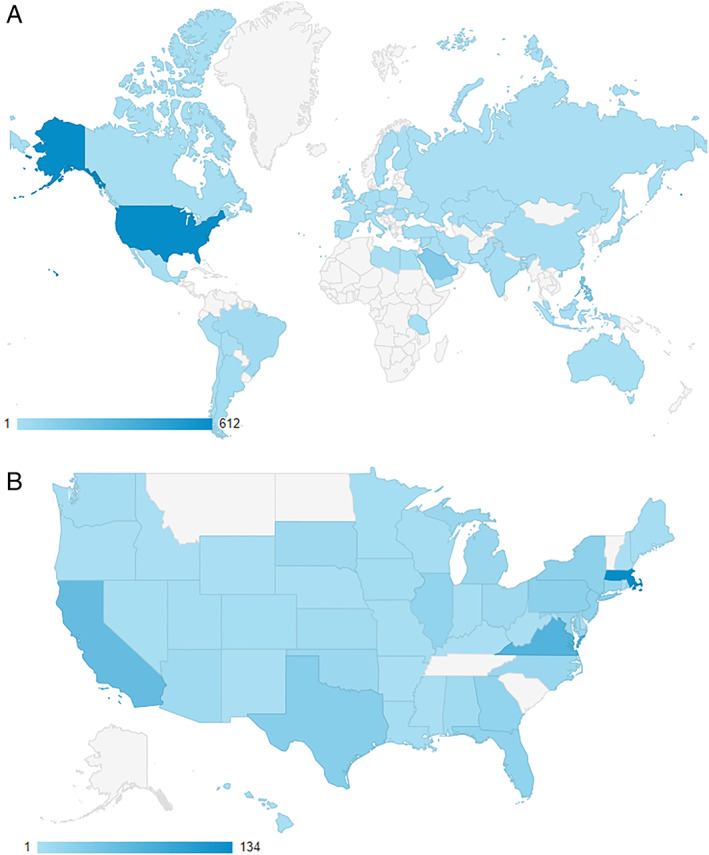
Number of unique visitors by country (A) and by state (B) up to and including May 4, 2020 (darker shade indicates a greater number of unique visitors). Courtesy of Google Analytics. [Color figure can be viewed at www.annalsofneurology.org]
Anecdotally, the coeditors have been contacted by neurologists across the country who provided feedback and suggestions on the protocols, in one case suggesting the development of an entirely new section (“Special Population: Immunocompromised Patients”).
Discussion
The viewership data gathered thus far provide some interesting insight into the usage of our protocols. First, we did not make projections on access, but feel that 465 unique visitors in a week of “normal” usage suggests an acceptable level of utility. There was no discernible trend in the number of daily visitors thus far, although we expect to see longitudinal trends over the next several weeks given the changing status of the pandemic. Although we did not expect to find a correlation between the number of visitors within a country and its COVID‐19 burden, it was notable that the Philippines hosted the greatest number of unique visitors after the USA, despite having no specific connection with our institution. Language is intuitively an important factor affecting access (English is an official language of the Philippines), along with exposure to promotion of the protocols and internet availability or censorship in some countries. We found that the number of visitors stratified by state showed a loose correlation with COVID‐19 burden; Massachusetts and California represent 2 of the 5 states with highest caseload at the time of this writing. In terms of page views by section, interest may be related to high prevalence or level of acuity of a neurological manifestation.
Whereas the usefulness of the protocols may be inferred by measuring viewership, it is not possible to evaluate behavioral changes of end users or patient outcomes in a tool targeting a global audience. In addition to data collection errors such as inaccuracies in geolocation germane to the use of data analytics, site visits and page views may underestimate utility if users multiply usage by printing out the protocols for future reference. The quality of data collection is also influenced by choice of analytics software.
We acknowledge the disadvantages of disseminating synthesized clinical information online and bypassing the journal peer review process. Most notably, these include the dangers of early adoption of nonvalidated research findings and application of recommendations to settings for which they are not designed. Although it has not been scrutinized in the literature, this format also intuitively shares some of the weaknesses of rapid reviews, generally thought to have poor compliance with evidence synthesis research standards.10
Looking forward, this method of rapid information synthesis may benefit from approach standardization at the scientific community level and establishment of uniform evaluative criteria, especially as they may be needed in future crises. We learned that this method does, however, exhibit a powerful advantage. Due to the dynamic nature of online content, we have received an abundance of valuable feedback from our peers across the country who have greatly enhanced our protocols. Our experience illustrates that, during these unprecedented times in which the spread of the pandemic outpaces our understanding of the virus, knowledge dissemination may no longer be an acceptable goal. Rather, collaboration should be our collective objective.
Author Contributions
A.C.‐A. contributed to the conception and design of the study. K.H.V.L. contributed to the conception and design of the study and the acquisition and analysis of data. P.A., J.G.S., T.F., C.T., A.D., T.N.N., K.S., M.A., A.S., A.M., M.P., S.Z., and D.M.G. contributed to the writing of the manuscript and development of the online resource that is the subject of this article.
Potential Conflicts of Interest
Nothing to report.
[Correction added on 27 June 2020, after first online publication: The middle initial was missing from author Michael D. Perloff's name and has been added.]
References
- 1. Song P, Karako T. COVID‐19: real‐time dissemination of scientific information to fight a public health emergency of international concern. Biosci Trends 2020;14:1–2. [DOI] [PubMed] [Google Scholar]
- 2. Johansson MA, Saderi D. Open peer‐review platform for COVID‐19 preprints. Nature 2020;579:29. [DOI] [PubMed] [Google Scholar]
- 3. Vervoort D, Ma X, Luc JGY, Zieroth S. Rapid scholarly dissemination and cardiovascular community engagement to combat the infodemic of the COVID‐19 pandemic. Can J Cardiol (in press) 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American Academy of Neurology . COVID‐19 Neurology Resource Center: articles and publications. 2020. Available at: https://www.aan.com/tools‐and‐resources/covid‐19‐neurology‐resource‐center/covid‐19‐articles‐and‐publications/. Accessed April 21, 2020.
- 5. Nguyen TN, Abdalkader M, Jovin TG, et al. Mechanical thrombectomy in the era of the COVID‐19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the Society of Vascular and Interventional Neurology. Stroke (in press) 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Association of British Neurologists. Association of British Neurologists Guidance on COVID‐19 for people with neurological conditions, their doctors and carers 2020. Available at: https://cdn.ymaws.com/www.theabn.org/resource/collection/6750BAE6-4CBC-4DDB-A684-116E03BFE634/ABN_Neurology_COVID-19_Guidance_22.3.20.pdf. Accessed April 20, 2020.
- 7. Adhikari SP, Meng S, Wu YJ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID‐19) during the early outbreak period: a scoping review. Infect Dis Poverty 2020;9:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li Y, Wang M, Zhou Y, et al. Acute cerebrovascular disease following COVID‐19: a single center, retrospective, observational study. SSRN Electr J (in press) 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Boston Medical Center . COVID‐19 neurology protocols. 2020. Available at: https://covidneurology.org. Accessed April 17, 2020.
- 10. Kelly SE, Moher D, Clifford TJ. Quality of conduct and reporting in rapid reviews: an exploration of compliance with PRISMA and AMSTAR guidelines. Syst Rev 2016;5:79. [DOI] [PMC free article] [PubMed] [Google Scholar]


