Abstract
Coronavirus disease 2019 (COVID‐19) has become a major global public health concern. The mortality rate for critically ill patients is up to 60%, and, thus, reducing the disease severity and case mortality is a top priority. Currently, cytokine storms are considered as the major cause of critical illness and death due to COVID‐19. After a systematical review of the literature, we propose that cross‐reactive antibodies associated with antibody‐dependent enhancement (ADE) may actually be the cause of cytokine storms. It would be more difficult to develop vaccines for highly pathogenic human coronaviruses (CoVs) if ADE characteristics are taken into consideration. Therefore, it is urgent to find an effective way to prevent the occurrence of severe illness as severe acute respiratory syndrome CoV‐2 specific drugs or vaccines are still in development. If the activation of memory B cells can be selectively inhibited in high‐risk patients at an early stage of COVID‐19 to reduce the production of cross‐reactive antibodies against the virus, we speculate that ADE can be circumvented and severe symptoms can be prevented. The mammalian target of rapamycin (mTOR) inhibitors satisfy such needs and it is recommended to conduct clinical trials for mTOR inhibitors in preventing the severity of COVID‐19.
Keywords: ADE, antibody‐dependent enhancement, coronavirus, cross‐reactive antibody, cytokine storm, immunity, mTOR inhibitors, rapamycin
Highlights
Cytokine storms are the major cause of critical illness and death due to COVID‐19. Antibody‐dependent enhancement (ADE) may be the major cause of cytokine storms. Selective inhibition of memory B cell activation by mTOR inhibitors could prevent ADE and reduce COVID‐19 severity.
1. INTRODUCTION
So far as of 3 May 2020, there is no vaccine for the 2019‐started novel coronavirus disease 2019 (COVID‐19). On 1 May 2020, U.S. Food and Drug Administration issued an emergency use authorization for the antiviral drug remdesivir for the treatment of patients with COVID‐19. 1 However, the clinical benefits of remdesivir in patients with severe disease are limited. 2 In addition to antiviral drugs and vaccines, convalescent plasma (CP) transfusion provides a potential option for treating severe patients with COVID‐19. However, the latest published research papers suggested that the severity of COVID‐19 is related to increased, rather than decreased, immunoglobulin G (IgG) response, 3 and that CP transfusion can be beneficial only to the patients who were given before 14 days post‐onset of illness (dpoi) rather than after that time. 4 About 20% patients with COVID‐19 have developed severe illness, and 5% have further developed critical illness with a mortality rate of 61.5%. 5 Therefore, it is urgent to find an alternative way to treat COVID‐19 while vaccine candidates are still under development and CP therapy is needed to be further investigated in randomized clinical studies.
COVID‐19 has many striking similarities to severe acute respiratory syndrome (SARS) which outbreak 17 years ago. A previous study demonstrated that the peripheral blood CD4+ and CD8+ T cells in SARS‐infected survivors showed a reversible decline. The decline and duration of T cells and the severity of the disease are closely related, while the irreversible decline leads to mortality. T‐cell decline coexists with the increase of interleukin 6 (IL‐6), tumor necrosis factor α (TNF‐α), and other proinflammatory cytokines. 6 The recent data collected from patients with COVID‐19 also confirmed that T‐cell counts are negatively correlated with the changes in the production of IL‐6, TNF‐α, and other proinflammatory cytokines. 7
The cytokine release syndrome (CRS) or so‐called cytokine storms are currently considered as the cause of critical illness and death. 8 Antibody‐dependent enhancement (ADE), especially the suboptimal antibody‐elated responds maybe the cause of the CRS. 9 , 10 , 11 , 12 After a systematical review of the literature, we propose that cross‐reactive antibodies associated with ADE may be the major cause of cytokine storms in highly pathogenic human coronavirus (CoV) infection, including SARS and COVID‐19. Methods specifically blocking this type of ADE will provide therapeutic potentials for patients suffering from severe COVID‐19, especially the elderly and health care workers.
2. ADE IN SARS AND COVID‐19
Patients with SARS who have developed antibodies earlier in the serum and have high antibody levels experienced a severe infection. 13 The median time that SARS‐CoV antibodies were detected in the serum was 16 days. It is remarkable that IgG antibodies were first detected in some patients as early as day 4 of the disease. The early occurrence of serum IgG antibodies is associated with a high incidence of entering the intensive care unit (ICU). 14 This phenomenon has also been reported in patients with COVID‐19. 3 According to the general understanding of antiviral immune response, high antibody levels indicate that pathogens are easily controlled and infections can be alleviated. Counterintuitively, the severity of SARS and COVID‐19 is associated with increased IgG response.
A recent study showed a rapid increase of lymphocyte counts and remarkable absorption of lung lesions in patients with COVID‐19 receiving CP transfusion before 14 dpoi. Notably, patients who received CP after 14 dpoi showed much less significant improvement. 4 Consistent with this study, previous research found that among 80 SARS‐CoV‐infected patients who received CP therapy, 33 showed good and 47 showed poor results. The better treatment outcome was observed among patients who were given CP before 14 dpoi (58.3% vs 15.6%; P < .01). 15 CP transfusion therapy is based on a hypothesis that CP is considered to have more neutralizing antibodies. Considering the increased IgG antibodies respond in the critically ill patient at an early stage, 3 , 13 , 14 we speculate that the early increased IgG antibodies are not the same as those in the CP. These antibodies are likely derived from cross‐reactive antibodies related to memory immunity, which leads to ADE.
Therefore, we hypothesize that SARS and COVID‐19 have the characteristic of ADE. Briefly, when virus A enters the body, it activates memory B cells and inhibits the activation of naive B cells. The memory B cells produce antibodies capable of binding to virus A. However, these are cross‐reactive antibodies, based on the immune memory of the previous infection by other similar virus strain A1 which has one or more similar epitopes to those of virus A. These cross‐reactive antibodies are capable of promoting virus entry into monocytes/macrophages via the Fc receptor, and subsequently, a large number of viruses are replicated and released after the immune escape (Figure 1).
Figure 1.
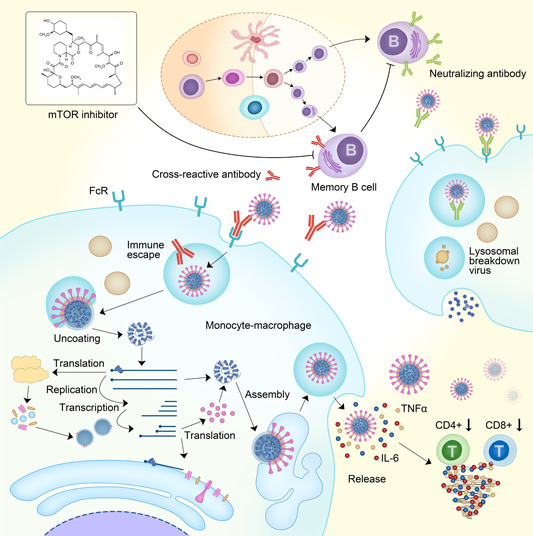
Antibody‐dependent enhancement (ADE) and cytokine release during coronavirus infection The upper right part of the figure: B cells differentiate and mature from their progenitor cells in the germinal center, and finally become plasma cells, secreting IgM at an early stage and IgG about 2 weeks post‐infection. These IgGs are neutralizing antibodies that bind to coronavirus surface spike proteins. The constant region of the antibody binds to the Fc receptor on the surface of the monocyte‐macrophage and is engulfed into the cell. Then, the lysosome recognizes the antibody‐virus complex, and the phagocytic complex is decomposed. Finally, virus fragments are released as part of the normal immune process. The lower left part of the figure: The antibodies secreted by memory B cells are cross‐reactive antibodies, which will inhibit the secretion of neutralizing antibodies by plasma cells. The cross‐reactive antibody binds to the virus with weak affinity, and after the complex binds to the Fc receptor, it is engulfed by monocyte macrophages. After entering the monocyte‐macrophage, because of weak affinity, the virus is separated from the cross‐reactive antibody and is not engulfed by the lysosome, leading to the immune escape. Subsequently, the virus uncoates, replicates, and assembles. Finally, a large number of mature viruses are released from the monocyte macrophages. At the same time, IL‐6, TNF‐α, and other cytokines are also released. These cytokines downregulate T cells (including CD4+ and CD8+). With more and more cytokines released, a so‐called cytokine storm is formed during the ADE process. The upper left corner shows that an mTOR inhibitor, rapamycin, could inhibit the activation of memory B cells and therefore inhibit the ADE process. IgG, immunoglobulin G; IgM, immunoglobulin M; IL‐6, interleukin 6; mTOR, mammalian target of rapamycin; TNF‐α, tumor necrosis factor α
3. ADE CAN EXPLAIN CHARACTERISTICS OF SEVERE COVID‐19
Pathological observations revealed that the exuding cells in the alveolar cavity of the patients died due to COVID‐19 were mainly monocytes/macrophages. Virus inclusions were also visible in the macrophages of patients with COVID‐19. 16 , 17 Immunohistochemical staining showed that the macrophages were SARS‐CoV‐2 positive, while the nucleic acid was tested positive by a polymerase chain reaction. The spleen and other immune organs exhibit macrophage hyperplasia, phagocytosis, and a decrease in the number of lymphocytes. 16 , 17
It was previously shown that the SARS‐CoV‐1 virus (SARS‐CoV) can enter macrophages via a suboptimal antibody‐mediated pathway and it can replicate in these cells. 18 Viral‐Track, which allows unsupervised detection of viral RNA in single‐cell RNA‐seq datasets, also found evidence of SARS‐COV‐2 infection in monocytes/macrophages in severe patients. 19 In addition, viral antigens were also detected in macrophages infiltrated into the alveolar interstitium and cavities of SARS‐CoV‐2‐infected hACE2‐expressing mice. 20 Moreover, immunofluorescent double staining showed that IL‐6 is primarily produced by infected macrophages. 17 These observations suggest that SARS‐CoV‐2 can also enter into monocytes/macrophages, 21 possibly through the Fc receptor.
Proinflammatory cytokines such as IL‐6 and TNF‐α are mainly derived from macrophages. The activity of macrophages and the massive release of these cytokines mutually confirm that the cytokine storm is the secondary event of macrophage activation. A recent study demonstrated a significantly enhanced production of cytokines and chemokines by macrophages in those treated with sera from deceased patients with SARS and virus as compared to cells treated with virus alone. Sera treatment alone did not induce cytokines or chemokines. Blockade of Fc gamma receptors reduced the production of proinflammatory cytokines from macrophages. 22
Typically, after the body is infected with a virus, virus‐specific T cells are required to kill the virus by killing the infected cells. However, cytokine IL‐6 can inhibit the differentiation of T cells and impair T‐cell immunity. 23 Therefore, the observed decrease in the number of T cells can be a secondary event of a cytokine storm.
Cross‐reactive antibodies trigger ADE. Hitherto, seven CoV's have been found infecting humans and three of these viruses (SARS‐CoV, SARS‐CoV‐2, and Middle East respiratory syndrome [MERS]‐CoV) cause SARS as well as severe illness and mortality. The remaining four low‐pathogenic CoV's (HCoV‐229E, HCoV‐OC43, HCoV‐NL63, and HCoV‐HKU1) only cause cold‐like symptoms. SARS‐CoV‐2 shares more than 60% sequence identity with these four cold‐causing CoV's and share even more than 80% sequence identity with SARS‐CoV. 24 The SARS‐CoV has multiple cross‐reactive epitopes with these low‐pathogenic CoV's. 25 The antibodies against these four low‐pathogenic CoV's have being investigated objectively in healthy individuals with greater than 70% positive rate of serum IgG antibodies, 26 indicating greater than 70% individuals have been infected with at least one of these CoV's. Interestingly, 75.75% (359/499), 75.95% (379/499), and 71.54% (357/499) individuals had remarkably low total T‐cell counts, and CD4+ and CD8+ T‐cell counts in patients with COVID‐19. 7
Most of the severe illnesses occur in adults, elderly, and those with comorbidity diseases that could transform into a critical situation. Since adolescents are less likely to develop severe illnesses, we focused on the correlation between cross‐reactive antibodies and age, comorbidity diseases, and other high‐risk factors. Among all the serum collected from 105 adults with aged ≥50 (mean, 67.9) years from seven sites in the USA, the detection rate of antibodies against four low pathogenicity CoV's was 91% to 100%. 27 HCoV‐229E and HCoV‐OC43 antibody levels continuously tracked in 44 members of 10 families in Seattle have shown that mean antibody titers increased directly with age. 28 In addition to causing common colds, human CoV's may also be involved in the etiology of severe diseases in all age groups. 29 Compared to the positive detection rate of 40% in children, serum antibody positivity in health care workers is 100%. 30 This fact might explain why some young health care workers with less than 40 years of age have progressed to severe illness and even death due to COVID‐19.
Collectively, we predict that once a patient is infected by SARS‐CoV‐2, the immune memory left by the previous infection with a low‐pathogenic CoV is activated. The memory B cell rapidly produces cross‐reactive antibodies. Fc receptors mediate the viral antibody complex enter into monocytes/macrophages, resulting in ADE. The virus replicates after an immune escape, which causes a rapid increase of virus progenies, the release of multiple proinflammatory cytokines, lymphocyte reduction, and immune dysregulation, leading to severe and critical illness in patients with COVID‐19 (Figure 1).
4. THERAPEUTIC POTENTIAL OF MECHANISTIC TARGET OF RAPAMYCIN INHIBITORS IN COVID‐19 TREATMENT
The mechanistic target of rapamycin (mTOR) pathway functions as a central regulator of cell metabolism, growth, proliferation, and survival. It senses both intracellular and extracellular signals to control the protein synthesis, lipids metabolism, autophagy, and transcription. 31 mTOR is a member of the phosphatidylinositol 3‐kinase‐related kinase family of protein kinases. mTOR is the key component of at least two distinct multiprotein complexes, mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2), which sense different signals to control different cellular processes. 32 The rapamycin‐sensitive mTORC1 mainly functions as a nutrient/energy/redox sensor and controls protein synthesis, lipid metabolism, and organelle biogenesis. The rapamycin‐insensitive mTORC2 serves as a regulator of the actin cytoskeleton, metabolism, and cell survival. 32
Due to the key role of the mTOR pathway in diverse cellular processes, it is not surprising that this pathway shapes the development and response of diverse immune cells. 33 mTOR controls the gene expression of myeloid immune cells to regulate their migration and cytokine expression. Inhibition of mTORC1 enhances the T‐cell stimulatory activity of dendritic cells (DCs) and promotes the autophagy of macrophages. mTORC2 controls cell polarity and chemotaxis of neutrophils and mast cells. Activation of mTORC1 controls the proliferation and acquisition of cytotoxicity of NK cells upon IL‐15 stimulation.
In addition, the mTOR pathway also plays a vital role in B‐cell development. mTORC1 controls BCL6 expression to control the fate of B cells in the germinal center. Inhibition of mTORC1 reduces the populations of antigen‐specific memory B cells after B‐cell activation. 34 Rapamycin treatment blocks murine B‐cell proliferation induced by anti‐IgM, and prevents B‐cell growth but not survival. 35 , 36 mTOR inhibitors, rapamycin/sirolimus, and ATP‐competitive inhibitors (INK128, PP242, Ku‐0063794, and AZD8055) have also been shown to suppress early B‐cell production in germinal centers. 37 , 38
If the activation of memory B cells can be selectively inhibited in these high‐risk patients at an early stage to reduce the production of cross‐reactive antibodies for SARS‐CoV‐2, we speculate that the ADE process can be avoided and severe symptoms can be alleviated. Considering the role of mTOR inhibitors in limiting the proliferation of memory B cells, patients treated with mTOR inhibitors are expected to have reduced early cross‐reactive antibody production and thus less ADE. In addition, mTOR inhibitor rapamycin also enhances the magnitude and quality of viral‐specific CD8+ T‐cell responses to vaccination in macaques. 39 In consideration of the pivotal role of mTOR in controlling cellular metabolism, pathogens have evolved elegant strategies to target this pathway within DCs and macrophage to promote immune escape. 40 These studies elucidated new mechanistic characteristics of mTOR inhibitors and suggested immune applications beyond their role as immunosuppressants.
On the other hand, mTOR inhibitor rapamycin blocks the replication of MERS‐CoV in vitro. 41 Adjuvant treatment with mTOR inhibitors and corticosteroids can significantly improve the outcome in ICU patients infected with the H1N1 influenza virus, 42 which provided additional evidence supporting the clinical usage of mTOR inhibitors for similar diseases.
There are a variety of clinically approved mTOR inhibitors in the market used as immunosuppressants during organ transplantation. Therefore, to prevent ADE and reduce the disease severity and case mortality, early application of mTOR inhibitors in patients with high‐risk of developing the severe illness is a promising direction for further investigation. The latest published research also supports the therapeutic potential of mTOR inhibitors against COVID‐19. 43 , 44
5. CLINICAL TRIAL PROPOSAL
It is recommended to conduct a randomized, double‐blind, placebo‐controlled, multicenter clinical trial to urgently confirm the safety and effectiveness of mTOR inhibitors in the prevention of COVID‐19 severity. The neutrophil‐to‐lymphocyte ratio (NLR) in patients with COVID‐19 is an early warning indicator of the development of severe disease. Among the patients of greater than 50 years of age, 50% of them with NLR greater than 3.13 will develop severe illness. 45 Pivotal clinical trials may enroll this subset of individuals at an early stage, within 2 weeks after onset, and evaluate the difference in the incidence of disease severity between the mTOR inhibitor intervention group and the control group. The intervention group should choose one of the clinically approved mTOR inhibitors, that is, sirolimus, everolimus, or temsirolimus. The primary endpoint should be the incidence of severe and critical symptoms. The secondary endpoints should include 28‐day recovery and mortality rates, changes in lymphocyte subpopulation counts, viral load, cytokine levels, and incidence of lung injury and respiratory distress. Currently, two small‐scale clinical trials using mTOR inhibitor sirolimus in treating COVID‐19 patients are ongoing (Clinicaltrials.gov Identifiers: NCT04371640 and NCT04341675).
6. SIGNIFICANCE
It would be more challenging to develop vaccines for SARS‐CoV‐2 if ADE characteristics are taken into consideration. Therefore, it is imperative to find an effective way to manage the occurrence of severe illness because the development of effective drugs or vaccines against SARS‐CoV‐2 infection requires a relatively long period of time. Treatment with mTOR inhibitors, if works as expected, will greatly ease the tension of medical resources and save countless lives worldwide.
7. LIMITATIONS AND POTENTIAL SOLUTIONS
In general, the situation of cross‐reactive antibody‐mediated protection during virus infection is ideal. CoV cross‐protection antibodies should be antibodies against S protein. According to current data, S protein cross‐reactive antibodies are not produced in the receptor‐binding domain region. 46 Moreover, recent studies have found that N protein antibodies appear earlier than those of S protein, 47 which further suggests that early high‐response antibodies are unlikely to provide protection against virus entry. Therefore, cross‐protection is less likely to occur, but more research is needed to address this possibility.
The release of inflammatory cytokines is potential double‐edged swords in viral infection and disease pathology. The innate immunity needs to be finely tuned to combat viral infection and to avoid cytokine storm. In addition to function as immunosuppressants, the mTOR inhibitors play multifunctional roles in innate immunity. 48 Therefore, early‐ and short‐term intervention by mTOR inhibitors should be incorporated in the design of clinical trials to minimize the unwanted immunosuppression effect. Moreover, IL‐6 might play a key role in the cytokine storm‐associated serious adverse outcomes and IL‐6 blockade has been initiated to treat severe COVID‐19 disease with respiratory failure (ClinicalTrials.gov Identifier: NCT04322773). In addition to mTOR inhibitors, combination therapy with anti‐IL‐6 antibody could be incorporated in the clinical trial for patients with critical SARS‐CoV‐2 pneumonia.
CONFLICT OF INTERESTS
Yunfeng Zheng is the inventor of the pending patent of application No. CN202010129707.8. Other authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
YZ proposed the concept, searched the literature, and prepare the first draft. SL confirmed the theoretical basis of immunology. RL and SL reviewed, modified, and improved manuscript. All authors have read and agreed to the published version of the manuscript.
Zheng Y, Li R, Liu S. Immunoregulation with mTOR inhibitors to prevent COVID‐19 severity: A novel intervention strategy beyond vaccines and specific antiviral medicines. J Med Virol. 2020;92:1495–1500. 10.1002/jmv.26009
Contributor Information
Renfeng Li, Email: rli@vcu.edu.
Shunai Liu, Email: liusa1031@ccmu.edu.cn.
REFERENCES
- 1. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment. Accessed 1 May 2020.
- 2. Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID‐19: a randomised, double‐blind, placebo‐controlled, multicentre trial. Lancet. 2020;395:1569–1578. 10.1016/S0140-6736(20)31022-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhang B, Zhou X, Zhu C, et al. Immune phenotyping based on neutrophil‐to‐lymphocyte ratio and IgG predicts disease severity and outcome for patients with COVID‐19. medRxiv. 2020. 10.1101/2020.03.12.20035048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Duan K, Liu B, Li C, et al. Effectiveness of convalescent plasma therapy in severe COVID‐19 patients. Proc Natl Acad Sci USA. 2020;117(17):9490‐9496. 10.1073/pnas.2004168117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS‐CoV‐2 pneumonia in Wuhan, China: a single‐centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475‐481. 10.1016/S2213-2600(20)30079-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liu S, Li X, Xing Y. Immunology testing of SARS (in Chinese). Foreign Med Sci. 2003;12(3):95‐98. 10.3760/cma.j.issn.1673-4092.2005.03.010 [DOI] [Google Scholar]
- 7. Diao B, Wang C, Tan Y, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID‐19). Frontiers in Immunology. 2020;11827. 10.3389/fimmu.2020.00827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pedersen SF, Ho Y. SARS‐CoV‐2: a storm is raging. J Clin Invest. 2020;130:2202‐2205. 10.1172/JCI137647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tetro JA. Is COVID‐19 receiving ADE from other coronaviruses? Microbes Infect. 2020;22(2):72‐73. 10.1016/j.micinf.2020.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cao X. COVID‐19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20:269‐270. 10.1038/s41577-020-0308-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Iwasaki A, Yang Y. The potential danger of suboptimal antibody responses in COVID‐19. Nat Rev Immunol. 2020. 10.1038/s41577-020-0321-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huang AT, Garcia‐Carreras B, Hitchings MDT, et al. A systematic review of antibody mediated immunity to coronaviruses: antibody kinetics, correlates of protection, and association of antibody responses with severity of disease. medRxiv. 2020. 10.1101/2020.04.14.20065771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ho MS, Chen WJ, Chen HY, et al. Neutralizing antibody response and SARS severity. Emerg Infect Dis. 2005;11(11):1730‐1737. 10.3201/eid1111.040659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee N, Chan PKS, Ip M, et al. Anti‐SARS‐CoV IgG response in relation to disease severity of severe acute respiratory syndrome. J Clin Virol. 2006;35(2):179‐184. 10.1016/j.jcv.2005.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cheng Y, Wong R, Soo YOY, et al. Use of convalescent plasma therapy in SARS patients in Hong Kong. Eur J Clin Microbiol Infect Dis. 2005;24(1):44‐46. 10.1007/s10096-004-1271-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guideline for diagnosis and treatment for novel coronavirus pneumonia (7th ed., Chinese). Beijing, China: National Health Commission of the People's Republic of China. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. Accessed 3 March 2020. [Google Scholar]
- 17. Becher T, Riascos‐Bernal DF, Kramer DJ, et al. The novel severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) directly decimates human spleens and lymph nodes. MedRxiv. 2020;126:619‐632. 10.1101/2020.03.27.20045427 [DOI] [Google Scholar]
- 18. Yip MS, Cheung CY, Li PH, Bruzzone R, Peiris JM, Jaume M. Investigation of antibody‐dependent enhancement (ADE) of SARS coronavirus infection and its role in pathogenesis of SARS. BMC Proc. 2011;5:P80. 10.1186/1753-6561-5-S1-P80 [DOI] [PubMed] [Google Scholar]
- 19. Bost P, Giladi A, Liu Y, et al. Host‐viral infection maps reveal signatures of severe COVID‐19 patients. Cell. 2020. 10.1016/j.cell.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bao L, Deng W, Huang B, et al. The pathogenicity of SARS‐CoV‐2 in hACE2 transgenic mice. Nature. 2020. 10.1038/s41586-020-2312-y [DOI] [PubMed] [Google Scholar]
- 21. Merad M, Martin JC. Pathological inflammation in patients with COVID‐19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020. 10.1038/s41577-020-0331-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu L, Wei Q, Lin Q, et al. Anti‐spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS‐CoV infection. JCI Insight. 2019;4(4):e123158. 10.1172/jci.insight.123158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tsukamoto H, Fujieda K, Senju S, Ikeda T, Oshiumi H, Nishimura Y. Immune‐suppressive effects of interleukin‐6 on T‐cell‐mediated anti‐tumor immunity. Cancer Sci. 2018;109(3):523‐530. 10.1111/cas.13433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu Y, Liu B, Cui J, et al. Similarities and evolutionary relationships of COVID‐19 and related viruses. arXiv. 2020. 10.20944/preprints202003.0316.v1 [DOI] [Google Scholar]
- 25. Yan K, Tan W, Zhang X, et al. Identification of epitopes on SARS‐CoV nucleocapsid protein that induce the cross‐or specific‐reactivity among SARS‐CoV, HCoV‐OC43 and HCoV‐229E (in Chinese). Chin J Virol. 2006;22(4):248‐255. 10.13242/j.cnki.bingduxuebao.001728 [DOI] [Google Scholar]
- 26. Zhou W, Wang W, Wang H, Lu R, Tan W. First infection by all four non‐severe acute respiratory syndrome human coronaviruses takes place during childhood. BMC Infect Dis. 2013;13:433. 10.1186/1471-2334-13-433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gorse GJ, Patel GB, Vitale JN, O'Connor TZ. Prevalence of antibodies to four human coronaviruses is lower in nasal secretions than in serum. Clin Vaccine Immunol. 2010;17(12):1875‐1880. 10.1128/CVI.00278-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schmidt OW, Allan ID, Cooney MK, Foy HM, Fox JP. Rises in titers of antibody to human coronaviruses OC43 and 229E in Seattle families during 1975‐1979. Am J Epidemiol. 1986;123(5):862‐868. 10.1093/oxfordjournals.aje.a114315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Riski H, Hovi T. Coronavirus infections of man associated with diseases other than the common cold. J Med Virol. 1980;6(3):259‐265. 10.1002/jmv.1890060309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mourez T, Vabret A, Han Y, et al. Baculovirus expression of HCoV‐OC43 nucleocapsid protein and development of a Western blot assay for detection of human antibodies against HCoV‐OC43. J Virol Methods. 2007;139(2):175‐180. 10.1016/j.jviromet.2006.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Laplante M, Sabatini DM. mTOR signaling at a glance. J Cell Sci. 2009;122(20):3589‐3594. 10.1242/jcs.051011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sabatini DM. Twenty‐five years of mTOR: uncovering the link from nutrients to growth. Proc Nat Acad Sci. 2017;114(45):11818‐11825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Weichhart T, Hengstschläger M, Linke M. Regulation of innate immune cell function by mTOR. Nat Rev Immunol. 2015;15(10):599‐614. 10.1038/nri3901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Raybuck AL, Cho SH, Li J, et al. B cell‐intrinsic mTORC1 promotes germinal center—defining transcription factor gene expression, somatic hypermutation, and memory B cell generation in humoral immunity. J Immunol. 2018;200(8):2627‐2639. 10.4049/jimmunol.1701321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kay JE, Kromwel L, Doe SE, Denyer M. Inhibition of T and B lymphocyte proliferation by rapamycin. Immunology. 1991;72(4):544‐549. [PMC free article] [PubMed] [Google Scholar]
- 36. Wicker LS, Boltz RC, Matt V, Nichols EA, Peterson LB, Sigal NH. Suppression of B cell activation by cyclosporin A, FK506 and rapamycin. Eur J Immunol. 1990;20:2277‐2283. 10.1002/eji.1830201017 [DOI] [PubMed] [Google Scholar]
- 37. Ye L, Lee J, Xu L, et al. mTOR promotes antiviral humoral immunity by differentially regulating CD4 helper T Cell and B cell responses. J Virol. 2017;91(4):e01653‐16. 10.1128/JVI.01653-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Limon JJ, So L, Jellbauer S, et al. mTOR kinase inhibitors promote antibody class switching via mTORC2 inhibition. Proc Natl Acad Sci USA. 2014;111(47):E5076‐E5085. 10.1073/pnas.1407104111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Turner AP, Shaffer VO, Araki K, et al. Sirolimus enhances the magnitude and quality of viral‐specific CD8+ T‐cell responses to vaccinia virus vaccination in rhesus macaques. Am J Transplant. 2011;11(3):613‐618. 10.1111/j.1600-6143.2010.03407.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nouwen LV, Everts B. Pathogens MenTORing macrophages and dendritic cells: manipulation of mTOR and cellular metabolism to promote immune escape. Cells. 2020;9(1):E161. 10.3390/cells9010161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kindrachuk J, Ork B, Hart BJ, et al. Antiviral potential of ERK/MAPK and PI3K/AKT/mTOR signaling modulation for Middle East respiratory syndrome coronavirus infection as identified by temporal kinome analysis. Antimicrob Agents Chemother. 2015;59(2):1088‐1099. 10.1128/AAC.03659-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang CH, Chung FT, Lin SM, et al. Adjuvant treatment with a mammalian target of rapamycin inhibitor, sirolimus, and steroids improves outcomes in patients with severe H1N1 pneumonia and acute respiratory failure. Crit Care Med. 2014;42(2):313‐321. 10.1097/CCM.0b013e3182a2727d [DOI] [PubMed] [Google Scholar]
- 43. Gordon DE, Jang GM, Bouhaddou M, et al. A SARS‐CoV‐2 protein interaction map reveals targets for drug repurposing. Nature. 2020. 10.1038/s41586-020-2286-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhou Y, Hou Y, Shen J, Huang Y, Martin W, Cheng F. Network‐based drug repurposing for novel coronavirus 2019‐nCoV/SARS‐CoV‐2. Cell Discov. 2020;6:14. 10.1038/s41421-020-0153-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Liu J, Liu Y, Xiang P, et al. Neutrophil‐to‐lymphocyte ratio predicts severe illness patients with 2019 novel coronavirus in the early stage. MedRxiv. 2020. 10.1101/2020.02.10.20021584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ju B, Zhang Q, Ge X, et al. Potent human neutralizing antibodies elicited by SARS‐CoV‐2 infection. bioRxiv. 2020. 10.1101/2020.03.21.990770 [DOI] [PubMed] [Google Scholar]
- 47. Hachim A, Kavian N, Cohen CA, et al. Beyond the spike: identification of viral targets of the antibody response to SARS‐CoV‐2 in COVID‐19 patients. medRxiv. 2020. 10.1101/2020.04.30.20085670 [DOI] [Google Scholar]
- 48. Saemann MD, Haidinger M, Hecking M, Horl WH, Weichhart T. The multifunctional role of mTOR in innate immunity: implications for transplant immunity. Am J Transplant. 2009;9:2655‐2661. [DOI] [PubMed] [Google Scholar]


