Dear Editor,
Since first reported in December 2019, the novel RNA β‐coronavirus disease 2019 (COVID‐19) has spread rapidly across the world with, as of the 3 May 2020, 3.3 million confirmed cases with >230 000 deaths worldwide and >200 countries affected [1]. The most common symptoms reported include dry cough, fever and fatigue with ground‐glass opacification bilaterally in the lungs on imaging and lymphopenia on haematological analysis. In severe cases, the patients can develop acute respiratory distress syndrome (ARDS) or multi‐organ failure, which can lead to death [2, 3]. Transmission of the virus [severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2)] is via direct contact or via droplets spread by a cough or sneeze from an infected individual. The difficulty in disease detection and containment has been the long course of COVID‐19. Current evidence shows an incubation period of up to 14 days after exposure to the virus, and on average most patients first display symptoms 5 days after initial exposure. More importantly, carriers are contagious even during this preceding asymptomatic incubation phase of the disease [2, 4].
In the UK, a general lockdown was introduced on the 23 March 2020 as the major public health measure to slow viral transmission. Even before then, hospitals in the NHS had been preparing for a surge in demand by re‐deploying staff and resources. Urological services have been impacted by the cancellation of routine elective surgery and limiting the diminishing surgical resources to select risk‐stratified patients only. The Royal Colleges of Surgeons (RCS) have produced Inter‐Collegiate guidance as to what procedures may be considered of sufficient urgency to take place during the pandemic, and within urology, these are further aided by the BAUS guidelines.
In considering the risk to patients attending for surgery, there is a paucity of data. Lei et al. [5] reported on 34 patients who underwent elective surgeries in Wuhan, China during the COVID‐19 pandemic, all who then re‐presented with COVID‐19 symptoms within 7 days of surgery. None of these patients reported symptoms prior to surgery and all had laboratory confirmed COVID‐19 after re‐admission. Seven of the 34 (20.6%) patients subsequently died of COVID‐19 complications. We therefore investigated all patients in the Hampshire Hospital Foundation Trust (HHFT) who were triaged and underwent urological surgery in the first 3 weeks of the UK COVID‐19 lockdown.
All patients on the urology waiting list at HHFT were reviewed and re‐classified according to the BAUS guidelines. Summaries of patients deemed to be in need of surgery were submitted to a newly formed hospital clinical priority committee for ratification. Following this surgery was arranged at HHFTs main NHS sites in North Hampshire Hospital, Basingstoke or the Royal Hampshire County Hospital, Winchester, or at the Hampshire Clinic BMI Healthcare; a newly available NHS resource in light of the COVID‐19 pandemic. By adopting this approach and by re‐configuring our services enabled procedures to be undertaken at ‘cold’ sites with low or no patients with COVID‐19.
All patients had standard pre‐COVID‐19 preoperative assessments with no COVID‐19 swabs taken preceding surgery. In addition, a HHFT standardised screening consent form for COVID‐19 symptoms was included as part of the pre‐assessment (Fig. 1) and patients were excluded if any symptoms were present.
Fig. 1.
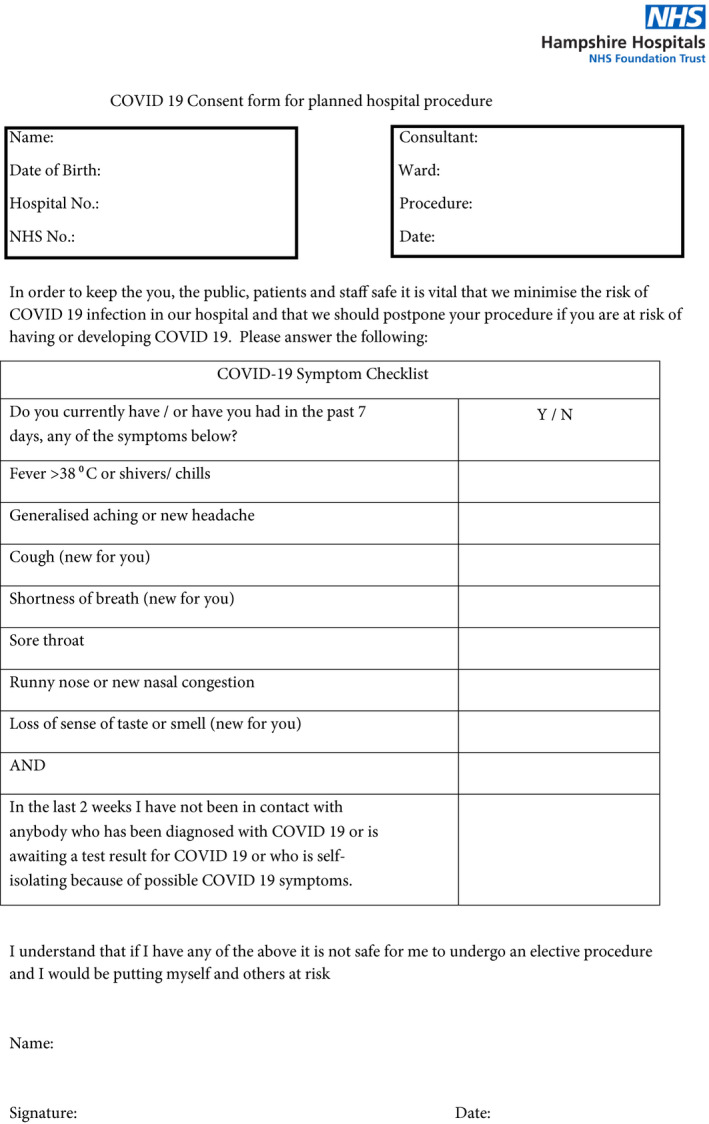
HHFT preoperative patient symptoms questionnaire consent form for COVID‐19.
A consecutive series of patients listed for operations during the first 3 weeks since the UK lockdown were identified for prospective follow‐up.
Standard operating procedures were followed as per the Public Health England (PHE) COVID‐19 infection control policy [6]. During the operation, standard personal protective equipment (PPE) for aerosol generating procedures was used by the anaesthetics team. The theatre team used standard PPE for non‐aerosol generating procedures.
During the postoperative period, all patients were recovered on designated ‘COVID‐19 negative’ surgical wards in multi‐patient shared bays.
After 14 days, all patients were contacted via a telephone consultation to assess for any potential postoperative or COVID‐19 complications.
A total of 52 consecutive patients underwent a urological operation between 23 March and 9 April 2020. The mean (range) age of the patients was 66 (22–89) years and 45 (86.5%) were male. Six (11.5%) operations were performed as an emergency and 46 (88.5%) patients had a general anaesthetic for their procedure. The majority of patients (69%) were American Society of Anesthesiologists (ASA) Classification Grade 2. The majority of patients stayed <23 h in hospital, with 92.3% of cases discharged within 48 h. This is summarised in Table 1, with the range of operations performed being from endoscopic rigid cystoscopy and bladder washout to radical laparoscopic nephrectomies. No patients reported symptoms of COVID‐19 preoperatively and none had been tested for COVID‐19 or admitted to hospital during the follow‐up period. Two (3.8%) Clavien–Dindo complications were reported, both were of Grade II. Both patients reported symptoms of UTI and received a 7‐day course of antibiotics from their GP after their transurethral resection of bladder tumour (TURBT).
Table 1.
Summary of patient factors and operative procedures in the study cohort.
| Variable | Value |
| Age, years, mean (range) | 66 (22–89) |
| Sex, n (%) | |
| Female | 7 (13.5) |
| Male | 45 (86.5) |
| Operation type, n (%) | |
| Scheduled | 46 (88.5) |
| Emergency | 6 (11.5) |
| ASA score, median | 2 |
| 1, n | 4 |
| 2, n | 36 |
| 3, n | 11 |
| 4, n | 1 |
| Anaesthetic type, n (%) | |
| General | 46 (88.5) |
| Sedation | 2 (3.8) |
| Spinal | 4 (7.7) |
| Operations performed, n | |
| Rigid cystoscopy + bladder washout | 1 |
| Rigid cystoscopy + bladder biopsy + cystodiathermy | 11 |
| Rigid cystoscopy + urethral dilatation for stricture management | 3 |
| Rigid cystoscopy + insertion of ureteric stent | 6 |
| Excision of penile lesion | 1 |
| Radical inguinal orchidectomy | 1 |
| Transperineal template prostate biopsy | 7 |
| TURBT | 17 |
| Laparoscopic radical nephrectomy | 5 |
| Length of stay, h, median | <23 |
| <23 h, n (%) | 35 (67.3) |
| 24–48 h, n (%) | 13 (25) |
| 49–72 h, n (%) | 3 (5.8) |
| >73 h, n (%) | 1 (1.9) |
Abbreviations: ARDS, acute respiratory distress syndrome; ASA, American Society of Anesthesiologists; COVID‐19, coronavirus disease 2019; PHE, Public Health England; PPE, personal protective equipment; SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2; TURBT, transurethral resection of bladder tumour.
During the time of the pandemic, careful consideration is essential to ascertain as to whether an urgent urological intervention is required or appropriate. A thorough discussion must be undertaken with the patients regarding the risks and benefits of operating, as well as considering the availability of resources. It seems sensible to offer procedures on a site with no or low numbers of COVID‐19‐confirmed cases and this may have contributed to our results.
It appears from the results of the present study that delivering urgent urological surgery during the COVID‐19 pandemic appears to be safe with minimal complications postoperatively and importantly with no evidence of hospital‐acquired COVID‐19 infections.
The reported incubation time of 2–14 days prior to the arrival of symptoms dictated our follow‐up period. Lei et al. [5] reported on average symptoms first presenting 5.2 days after the operation. We can therefore reasonably assume that any patients who contracted COVID‐19 either before or during their operation will have developed symptoms by the follow‐up stage. Furthermore, no patients required re‐admission during the 14‐day follow‐up period in our present cohort.
Our present data are somewhat at odds with the previously published study by Lei et al. [5], where all patients developed COVID‐19 symptoms and required hospital re‐admission after elective surgery. There are many potential factors that may have contributed to these different results. Firstly, our patient cohort is limited to urological procedures only, which in general are endoscopic in nature and may not have the same ‘systemic stress response’ as the other types of surgeries listed, such as radical gastrectomy or radical resection of rectal cancer. However, our present cohort included five cases of laparoscopic radical nephrectomies, which are considered as high‐risk major surgeries in urology. Furthermore, by the lockdown stage in the UK, the awareness of COVID‐19 within the medical and general population had increased, with social distancing in the community already in place by this stage, which may have decreased the incidence of infection within the community. In addition, PPE advice from PHE had already been implemented by this stage to prevent transmission both from patient to staff, as well as vice versa. However as of 3 May 2020, there have been 2827 confirmed cases of COVID‐19 in the Hampshire Upper Tier Local Authority area [7]. This is the third highest number of cases in England, with an estimated overall local population of ~1.3 million people [8]. Therefore, the disease by the lockdown stage was likely already prevalent in the local community, and in particular, the actual number of COVID‐19 cases will be higher than the official confirmed cases as people with COVID‐19 symptoms who did not require hospital admission will have neither been swabbed nor counted.
Cases were performed where possible as either a day‐case or short inpatient admission in order to limit patient exposure to the clinical environment, with >90% of cases discharged home within 48 h. One patient stayed >73 h and had a 50‐day length of stay. He was admitted with urosepsis following a collapse at home and had known advanced prostate cancer with bilateral stents in situ. An emergency stent change was performed on day 45 of admission due to bacterial colonisation and the patient was discharged on day 5 postoperatively after appropriate social care support was arranged.
There were two complications discovered in the postoperative period, both were of UTI symptoms after an endoscopic procedure, which were treated in the community with a standard 7‐day course of oral antibiotics, which fully resolved the symptoms. This is within the normal parameters expected after general endoscopic urological operations, where the risk of infections is quoted as between 10–50%.
Our present study supports the continued delivery of appropriately triaged urgent urological surgery during the COVID‐19 pandemic. A thorough assessment accounting for the risks and benefits for each case is necessary, and as the duration of the pandemic progresses, the ability to continue delivering urgent surgical care will greatly help mitigate the longer‐term impact of delaying treatment and meet the urgent needs of patients without COVID‐19.
Funding source
None.
Author contributors
Tim Nedas, Louise Paramore and Bob Yang designed the study, collected and analysed the data. All authors participated in data collection. Louise Paramore and Bob Yang drafted the manuscript. Richard Hindley and Timothy Nedas revised the final manuscript.
Conflict of Interests
None declared.
L.P. and B.Y. are co‐first authors.
References
- 1.World Health Organization. Coronavirus disease (COVID‐19) pandemic. Available at: https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019. Accessed May 2020
- 2. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID‐19) outbreak. J Autoimmun 2020; 109: 102433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xia XY, Wu J, Liu HL et al. Epidemiological and initial clinical characteristics of patients with family aggregation of COVID‐19. J Clin Virol 2020; 127: 104360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Singhal T. A review of coronavirus disease‐2019 (COVID‐19). Indian J Pediatr 2020; 87: 281–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lei S, Jiang F, Su W et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID‐19 infection. EClinicalMedicine 2020; 100331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Public Health England . COVID‐19 personal protective equipment (PPE). GOV.UK. 2020. Available at: https://www.gov.uk/government/publications/wuhan‐novel‐coronavirus‐infection‐prevention‐and‐control/covid‐19‐personal‐protective‐equipment‐ppe. Accessed April 2020
- 7. UK Government . Coronavirus (COVID‐19) cases in the UK – Data Dashboard. GOV.UK, Available at: https://coronavirus.data.gov.uk/#local‐authorities. Accessed May 2020
- 8. Hampshire County Council . Population statistics. Hampshire County Council. Available at: https://www.hants.gov.uk/landplanningandenvironment/facts‐figures/population. Accessed April 2020 [Google Scholar]


