Dear Editor,
The antimalarials, chloroquine and hydroxychloroquine (HCQ), and the antivirals lopinavir/ritonavir have been recently recorded as having anti‐severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) effects. 1 In particular, regarding Italy, one of the countries most affected by the pandemic, the Italian Society of Infectious and Tropical disease (Lombardy section) has recommended the use of HCQ for treatment of coronavirus disease 2019 (COVID‐19). 2 HCQ is widely used to treat dermatologic and rheumatologic diseases, and it has been described as one of the main drugs triggering acute generalized exanthematous pustulosis (AGEP). 3 , 4 Only one single case of AGEP induced by HIV post‐exposure prophylaxis with lopinavir/ritonavir has been reported. 5
A 70‐year‐old Italian woman with no personal/family history of psoriasis was admitted to our clinic for the rapid onset of a diffuse, pruritic pustular eruption. Three weeks before, she had been treated for SARS‐CoV‐2 pneumonia with lopinavir/ritonavir 200/50 mg two tablets and HCQ 200 mg bid for 10 days with a good response. Three days after the withdrawal of the treatment, she referred the onset of a skin eruption on the upper arms, rapidly spreading to the trunk. She consulted her primary care physician and began treatment with oral prednisone 0.3 mg/kg daily. Seven days later, due to the worsening of her skin eruption, the patient decided to consult the emergency department.
Physical examination revealed a widespread eruption on an erythematous–oedematous base, with scattered pinhead‐sized pustules and scales, involving the face, trunk and upper limbs. Targetoid lesions studded with small pustules were present in a symmetric pattern over buttocks, thighs and legs (Fig. 1). Mucous membranes, palms and soles were spared. The patient denied any other recent drug intake. A skin biopsy taken from the thigh showed a subcorneal pustule with mild focal acanthosis and spongiosis, neutrophilic exocytosis, sparse keratinocyte necrosis, and a perivascular lymphocytic infiltrate with rare neutrophils and eosinophils (Fig. 2), consistent with AGEP. The patient was suggested to gradually taper prednisone within 30 days with a slow but progressive resolution.
Figure 1.

(a) Widespread acute rash on an erythematous–oedematous base, with scattered pinhead‐sized pustules involving the face, trunk and upper limbs; the patient is wearing a surgical mask and gloves in accordance with the hospital's anti‐coronavirus disease 2019 recommendations. (b) Extensive desquamation with scattered pustules on the abdomen and targetoid lesions on the thigh. (c) Erythematous–oedematous targetoid lesions covered by discrete small pustules and scales.
Figure 2.
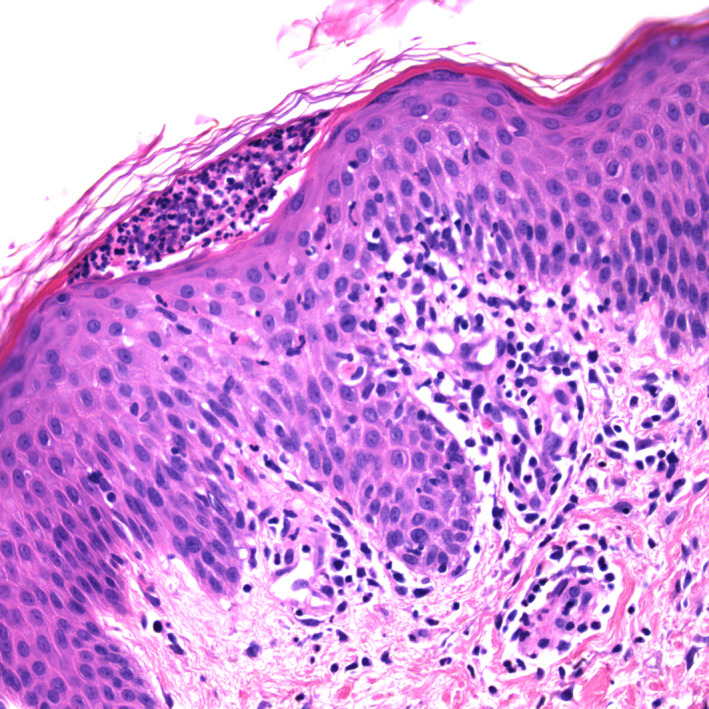
Subcorneal neutrophilic pustule, slight spongiosis with acanthosis, neutrophilic exocytosis, rare keratinocyte necrosis and a perivascular infiltrate consisting of lymphocytes with rare neutrophils and eosinophils (haematoxylin–eosin stain; original magnification: ×20).
Acute generalized exanthematous pustulosis is classically characterized by a sudden onset of widespread non‐follicular sterile pustules arising within large areas of oedematous erythema; it has been attributed to drugs in 90% of cases. 6 Rarely, AGEP can manifest itself in an atypical fashion with the development of target‐like lesions. This presentation, also reported as generalized pustular figurate erythema or AGEP with erythema multiforme‐like lesions or atypical AGEP, has been described especially in patients taking HCQ. 7 , 8 , 9 Although we cannot rule out that lopinavir/ritonavir could be implicated into the rash, 5 we suggest that HCQ was the probable triggering drug in our COVID‐19 patient because this antimalarial is considered one of the most frequently mentioned drugs causing AGEP both in its typical and atypical form. 3 , 6 Infectious viral agents such as parvovirus B19, cytomegalovirus and coxsackie B4 have also been reported as exceptionally AGEP related. 3 , 6 Although some skin eruptions have been recently associated with SARS‐CoV‐2 including varicella‐like exanthems, erythematous or urticarial rashes, the development of pustular lesions has never been described in COVID‐19. 10
AGEP is considered a self‐limiting disease with good prognosis that usually resolves in 15 days after the causative drug is withdrawn. 3 , 6 However, HCQ‐induced AGEP accompanied by erythema multiforme‐like lesions seems to follow a more recalcitrant course than usual, as it occurred in our patient. It predominantly involves women and is characterized by a longer latent period and a protracted course requiring systemic corticosteroid administration. 7
Because of the actual spreading use of HCQ, not only for dermatological and rheumatological conditions but also for the treatment of COVID‐19 patients, it is likely that clinicians could observe an increased number of cases of HCQ‐induced AGEP in the near future.
Acknowledgements
The patients in this manuscript have given written informed consent to publication of their case details.
Funding sources: none reported.
References
- 1. Costanzo M, De Giglio MAR, Roviello GN. SARS‐CoV‐2: recent reports on antiviral therapies based on lopinavir/ritonavir, darunavir/umifenovir, hydroxychloroquine, remdesivir, favipiravir and other drugs for the treatment of the new coronavirus. Curr Med Chem 2020; 27. 10.2174/0929867327666200416131117. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2. http://www.simit.org/medias/1569‐covid19‐vademecum‐13‐03‐202.pdf. (last accessed: 17 April 2020).
- 3. Sidoroff A, Dunant A, Viboud C et al. Risk factors for acute generalized exanthematous pustulosis (AGEP)‐results of a multinational case‐control study (EuroSCAR). Br J Dermatol 2007; 157: 989–996. [DOI] [PubMed] [Google Scholar]
- 4. Sharma AN, Mesinkovska NA, Paravar T. Characterizing the adverse dermatologic effects of hydroxychloroquine: a systematic review. J Am Acad Dermatol 2020; S0190‐9622(20)30564‐8. 10.1016/j.jaad.2020.04.024 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5. Ghosn J, Duvivier C, Tubiana R, Katlama C, Caumes E. Acute generalized exanthematous pustulosis induced by HIV postexposure prophylaxis with lopinavir‐ritonavir. Clin Infect Dis 2005; 41: 1360–1361. [DOI] [PubMed] [Google Scholar]
- 6. Szatkowski J, Schwartz RA. Acute generalized exanthematous pustulosis (AGEP): A review and update. J Am Acad Dermatol 2015; 73: 843–848. [DOI] [PubMed] [Google Scholar]
- 7. Schwartz RA, Janniger CK. Generalized pustular figurate erythema: a newly delineated severe cutaneous drug reaction linked with hydroxychloroquine. Dermatol Ther 2020; 6: e13380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lin JH, Sheu HM, Lee JY. Acute generalized exanthematous pustulosis with erythema multiforme‐like lesions. Eur J Dermatol 2002; 12: 475–478. [PubMed] [Google Scholar]
- 9. Kostopoulos TC, Krishna SM, Brinster NK, Ortega‐Loayza AG. Acute generalized exanthematous pustulosis: atypical presentations and outcomes. J Eur Acad Dermatol Venereol 2015; 29: 209–214. [DOI] [PubMed] [Google Scholar]
- 10. Marzano AV, Genovese G, Fabbrocini G et al. Varicella‐like exanthem as a specific COVID‐19‐associated skin manifestation: multicenter case series of 22 patients [published online ahead of print, 2020 Apr 16]. J Am Acad Dermatol 2020; S0190‐9622(20)30657‐5. 10.1016/j.jaad.2020.04.044 [DOI] [PMC free article] [PubMed] [Google Scholar]


