Cutaneous manifestations in patients with COVID‐19 infection are increasingly being reported. Several patterns have been described since the initial report by Recalcati,1 including erythematous maculopapular,1 urticarial,1, 2 chickenpox‐like,1, 3 purpuric periflexural,4 transient livedo reticularis,5 and acroischaemic or chilblain‐like lesions.6, 7 We report the observation a new pattern with erythema multiforme (EM)‐like lesions in four hospitalized patients with COVID‐19 infection.
All four patients were women, with a mean age of 66.75 years (range 58–77 years). Mean interval between the onset of COVID‐19 symptoms to the appearance of cutaneous lesions was 19.5 days (range 16–24 days). One patient developed the skin rash during hospitalization, while the remaining three patients had been previously discharged after clinical, analytical and radiological improvement, and a negative COVID‐19 PCR test.
These three patients returned to the emergency department because of the skin rashes at 6, 7 and 4 days after discharge, respectively. Laboratory tests at the time of presentation showed worsening of one or more parameters (C‐reactive protein, D‐dimer or lymphocyte count), compared with those at the time of discharge. However, none of the patients presented recurrence of clinical symptoms of COVID‐19. Microbiological studies were performed in two patients, which excluded other infectious diseases (Table 1). In all patients, the skin lesions had begun as erythematous papules on the upper trunk, which progressively turned to erythematoviolaceous patches with a dusky centre, and a pseudovesicle in the middle. Typical EM targetoid lesions were observed in two patients. Lesions coalesced markedly on the back, and then spread to the face and limbs within 1 week, without involvement of the palms or soles (Fig. 1). These patients underwent oral cavity examination, which revealed palatal macules and petechiae.
Table 1.
Clinical and laboratory findings of the four patients with erythema multiforme‐like eruption.
| Patient | Sex | Age, years | Days after symptomsa | Days after treatmenta | Drugs | Microbiological tests | Worsening of laboratory parametersb |
| 1 | F | 63 | 19 | 16 | L/R, H, A, Cs, Ce | Not performed | Elevation of CRP and D‐dimer |
| 2 | F | 77 | 16 | 11 | L/R, H, A, Cs | Negative for HIV, EBV, CMV, VZV, HSV, M. pneumoniae, syphilis | Not performed |
| 3 | F | 58 | 24 | 15 | L/R, H, A, Cs, Ce | Not performed | Elevation of D‐dimer; decrease in lymphocyte count |
| 4 | F | 69 | 19 | 10 | L/R, H, A | Negative EVB for HIV, EBV, CMV, VZV, HSV, M. pneumoniae, syphilis. HSV PCR found in vesicle swab | Elevation of CRP and D‐dimer; decrease in lymphocyte count |
A, azithromycin; Ce, ceftriaxone; Cs, corticosteroids; CMV, cytomegalovirus; CRP, C‐reactive protein; EBV, Epstein–Barr virus; H, hydroxychloroquine; HIV, human immunodeficiency virus; HSV, herpes simplex virus (PCR multiplex); LR, lopinavir/ritonavir; M., Mycoplasma; VZV, varicella zoster virus. aDays from the onset of COVID‐19 symptoms and from the start of treatment to the appearance of cutaneous lesions, respectively; bworsening of laboratory parameters at the time of skin lesions, compared with those at the time of discharge.
Figure 1.
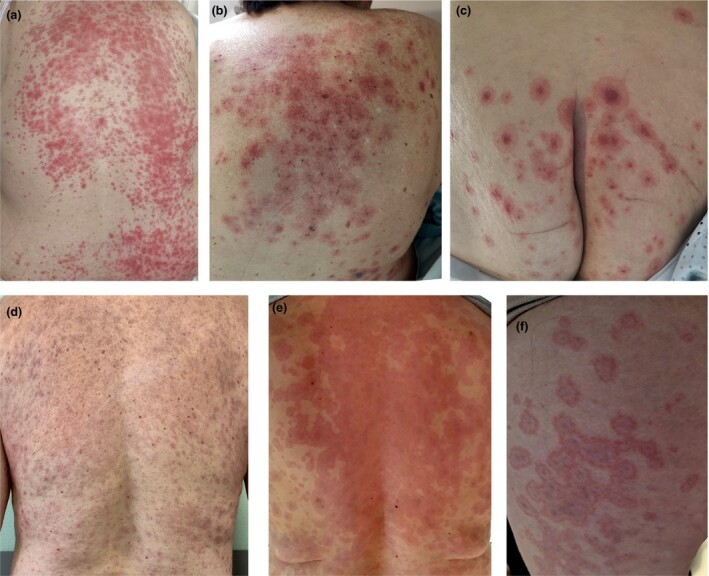
Clinical presentation of erythema multiforme (EM)‐like exanthem in (a) Patient 1; (b) Patient 2; (d) Patient 3; and (e) Patient 4 showing coalescing erythemato violaceous patches with a dusky centre, some of them with pseudovesicles in the middle, located on the back. Typical EM targetoid lesions were observed on (c) the buttocks of Patient 2 and (f) the thigh of Patient 4.
Histological examination was similar in all patients, revealing a normal basket‐weave stratum corneum, and mild to moderate spongiosis in epidermis. The dermis showed dilated vessels filled with neutrophils, extravasation of red blood cells, and lymphocytic perivascular and interstitial infiltrate. Basal vacuolar changes with interface dermatitis were observed in one patient, and lymphocytic exocytosis in another (Fig. 2). All patients were treated with systemic corticosteroids with progressive resolution of the skin lesions within 2–3 weeks.
Figure 2.
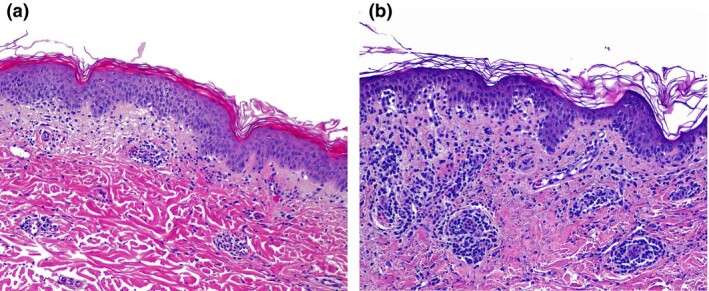
(a) Histological examination of Patient 1 showed normal basketweave stratum corneum, mild to moderate spongiosis and lymphocytic exocytosis in the epidermis, while the dermis showed dilated vessels filled with neutrophils, extravasation of red blood cells, and lymphocytic perivascular and interstitial infiltrate. (b) Patient 3 had basal vacuolar changes with interface dermatitis.
We are facing challenging times in dermatology. New information and details of cutaneous manifestations possibly related to COVID‐19 are emerging every day. Further studies are needed to evaluate whether these lesions are associated with the virus, the drugs used or any other conditions. EM is linked to infectious agents in 90% of cases, while drug‐associated EM is reported in < 10%. Herpes simplex virus and Mycoplasma pneumoniae are the main agents, but other viruses have been reported, such as adenovirus, coxsackievirus and parvovirus B19.8 We suggest that this EM‐like or target‐like exanthem might be another pattern of exanthem associated with COVID‐19 infection. Recent articles have also reported targetoid lesions in exanthems of patients with COVID‐19 infection.9, 10 In addition, the presence of pseudovesicles and enanthem are two clues that suggest an infectious cause rather than a drug reaction. However, we cannot positively exclude the involvement of the various drugs administered to the patients. To our knowledge, this is a first observation that will require further investigation.
Acknowledgement
We thank all the health workers who have been fighting against COVID‐19 in Spain. Special thanks to dermatologists G. Segurado, A. Hermosa, M. Prieto, A. Gonzalez, C. Pindado, O. M. Moreno‐Arrones, A. Ballester, N. Jimenez, S. Vaño, B. Perez and M. Fernandez.
Contributor Information
J. Jimenez‐Cauhe, Departments of Department of Dermatology Ramón y Cajal University Hospital Universidad de Alcalá de Henares Instituto de investigación Sanitaria del Hospital, Ramón y Cajal (Irycis) Madrid Spain
D. Ortega‐Quijano, Departments of Department of Dermatology Ramón y Cajal University Hospital Universidad de Alcalá de Henares Instituto de investigación Sanitaria del Hospital, Ramón y Cajal (Irycis) Madrid Spain
I. Carretero‐Barrio, Department Pathology Ramon y Cajal University Hospital Universidad de Alcalá de Henares Instituto de investigación Sanitaria del Hospital, Ramón y Cajal (Irycis) Madrid Spain
A. Suarez‐Valle, Departments of Department of Dermatology Ramón y Cajal University Hospital Universidad de Alcalá de Henares Instituto de investigación Sanitaria del Hospital, Ramón y Cajal (Irycis) Madrid Spain
D. Saceda‐Corralo, Departments of Department of Dermatology Ramón y Cajal University Hospital Universidad de Alcalá de Henares Instituto de investigación Sanitaria del Hospital, Ramón y Cajal (Irycis) Madrid Spain
C. Moreno‐Garcia del Real, Department Pathology Ramon y Cajal University Hospital Universidad de Alcalá de Henares Instituto de investigación Sanitaria del Hospital, Ramón y Cajal (Irycis) Madrid Spain
D. Fernandez‐Nieto, Departments of Department of Dermatology Ramón y Cajal University Hospital Universidad de Alcalá de Henares Instituto de investigación Sanitaria del Hospital, Ramón y Cajal (Irycis) Madrid Spain
References
- Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020; 345: e212–e213. 10.1111/jdv.16387 [DOI] [PubMed] [Google Scholar]
- Fernandez‐Nieto D, Ortega‐Quijano D, Segurado‐Miravalles G et al. Comment on: Cutaneous manifestations in COVID‐19: a first perspective. Safety concerns of clinical images and skin biopsies. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tammaro A, Adebanjo GAR, Parisella FR et al. Cutaneous manifestations in COVID‐19: the experiences of Barcelona and Rome. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez‐Cauhe J, Ortega‐Quijano D, Prieto‐Barrios M et al. Reply to “COVID‐19 can present with a rash and be mistaken for dengue”: petechial rash in a patient with COVID‐19 infection. J Am Acad Dermatol 2020. 10.1016/j.jaad.2020.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manalo IF, Smith MK, Cheeley J, Jacobs R. A dermatologic manifestation of COVID‐19: transient livedo reticularis. J Am Acad Dermatol 2020. 10.1016/j.jaad.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez‐Nieto D, Jimenez‐Cauhe J, Suarez‐Valle A et al. Characterization of acute acro‐ischemic lesions in non‐hospitalized patients: a case series of 132 patients during the COVID‐19 outbreak. J Am Acad Dermatol 2020. 10.1016/j.jaad.2020.04.093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccolo V, Neri I, Filippeschi C et al. Chilblain‐like lesions during COVID‐19 epidemic: a preliminary study on 63 patients. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokumbi O, Wetter DA. Clinical features, diagnosis, and treatment of erythema multiforme: a review for the practicing dermatologist. Int J Dermatol 2012; 51: 889–902. [DOI] [PubMed] [Google Scholar]
- Amatore F, Macagno N, Mailhe M et al. SARS‐CoV‐2 infection presenting as a febrile rash. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damme van C, Berlingin E, Saussez S, Accaputo O. Acute urticaria with pyrexia as the first manifestations of a COVID‐19 infection. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16523 [DOI] [PMC free article] [PubMed] [Google Scholar]


