Abstract
The ocular surface has been suggested as a site of infection with Coronavirus‐2 (SARS‐CoV‐2) responsible for the coronavirus disease‐19 (COVID‐19). This review examines the evidence for this hypothesis, and its implications for clinical practice. Severe Acute Respiratory Syndrome Coronavirus‐2 (SARS‐CoV‐2), responsible for the COVID‐19 pandemic, is transmitted by person‐to‐person contact, via airborne droplets, or through contact with contaminated surfaces. SARS‐CoV‐2 binds to angiotensin converting enzyme‐2 (ACE2) to facilitate infection in humans. This review sets out to evaluate evidence for the ocular surface as a route of infection. A literature search in this area was conducted on 15 April 2020 using the Scopus database. In total, 287 results were returned and reviewed. There is preliminary evidence for ACE2 expression on corneal and conjunctival cells, but most of the other receptors to which coronaviruses bind appear to be found under epithelia of the ocular surface. Evidence from animal studies is limited, with a single study suggesting viral particles on the eye can travel to the lung, resulting in very mild infection. Coronavirus infection is rarely associated with conjunctivitis, with occasional cases reported in patients with confirmed COVID‐19, along with isolated cases of conjunctivitis as a presenting sign. Coronaviruses have been rarely isolated from tears or conjunctival swabs. The evidence suggests coronaviruses are unlikely to bind to ocular surface cells to initiate infection. Additionally, hypotheses that the virus could travel from the nasopharynx or through the conjunctival capillaries to the ocular surface during infection are probably incorrect. Conjunctivitis and isolation of the virus from the ocular surface occur only rarely, and overwhelmingly in patients with confirmed COVID‐19. Necessary precautions to prevent person‐to‐person transmission should be employed in clinical practice throughout the pandemic, and patients should be reminded to maintain good hygiene practices.
Keywords: ACE2, conjunctivitis, coronavirus, COVID‐19, ocular surface, SARS‐CoV‐2
Coronaviruses are separated into four types: alphacoronaviruses, betacoronaviruses, gammacoronaviruses and deltacoronaviruses. Alphacoronaviruses and betacoronaviruses infect mammals, and gammacoronaviruses and deltacoronaviruses predominantly infect birds. 1 The greatest diversity of coronaviruses have been found in bats and birds, suggesting that these are the primary reservoirs of these viruses, 1 with bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavirus. 2
Of the coronaviruses that are known to infect humans, human coronavirus (hCoV) 229E and NL63 are alphacoronaviruses and OC43, HKU1, severe acute respiratory syndrome coronavirus (SARS‐CoV), Middle East respiratory syndrome coronavirus (MERS‐CoV) and SARS‐CoV‐2 are betacoronaviruses. All coronaviruses are termed ‘enveloped’ viruses due to the lipid membrane that surrounds their capsid (protein), which in turn contains RNA (genetic material). Proteins protrude from their lipid envelope (Figure 1) and these can be imaged with electron microscopy as a corona surrounding the virus – hence their name. Coronaviruses contain four major structural proteins, the spike, nucleocapsid, membrane, and envelope proteins. The nucleocapsid, membrane and envelope proteins are mainly involved in forming and structuring the virus, whereas the spike protein is also involved in binding to host cells. 3
Figure 1.
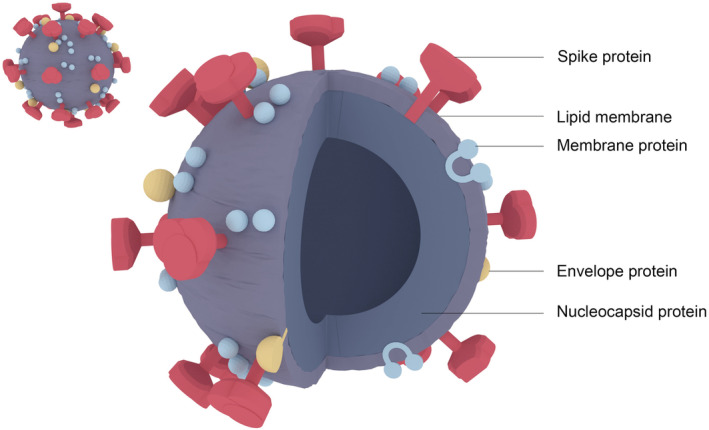
Representation of SARS‐CoV‐2 viral particles (drawn by Dr Chau‐Minh Phan, Centre for Ocular Research & Education, School of Optometry and Vision Science, University of Waterloo, Canada)
The coronavirus SARS‐CoV‐2 causes coronavirus disease 2019 (COVID‐19). COVID‐19 was declared a pandemic by the World Health Organization (WHO) on 11 March 2020 4 and at the time of writing, cases have been reported by nearly all countries and territories in the world (n = 212). 5 COVID‐19 has resulted in a large number of deaths, causing changes to the daily lives of many people and significant economic losses.
As of 5 May 2020, COVID‐19 has been confirmed in nearly three and a half million people and resulted in just over 230,000 deaths. 6 One of the first widely reported deaths due to SARS‐CoV‐2 was an ophthalmologist working at Wuhan Central Hospital in early January 2020, who reported he had contracted COVID‐19 from an asymptomatic glaucoma patient. He succumbed to the disease one month later. 7 Subsequently, there has been a great deal of interest in the scientific literature as well as in the lay press about the association of SARS‐CoV‐2 with the ocular surface. This has resulted in speculation regarding the safety of contact lenses,8, 9 as well as the potential for transmission of the virus to and from the ocular surface, with implications for transmission among the general population and specifically in ophthalmic care.
The authors conducted a recent review of the literature which indicates that contact lens wear is still a safe form of vision correction, as long as wearers continue to use good hygiene practices. 8 However, it is clear that much of the speculation regarding the potential to transmit SARS‐CoV‐2 to and from the ocular surface has not been based on an analysis of the available literature. Hence, the authors have conducted a thorough literature search in this area, and an assessment of this literature is presented in this review, particularly focusing on what is known about the ability of coronaviruses to adhere to ocular surface cells, the presence of coronaviruses at the ocular surface and the association of conjunctivitis with COVID‐19.
Literature search strategy
A literature search was conducted on 15 April 2020 in the Scopus database using the search terms ‘coronavirus’ AND ‘conjunctiv*’ OR ‘cornea’ OR ‘ocular surface’, which yielded 91 documents; and ‘SARS’ AND ‘conjunctiv*’ OR ‘cornea’ OR ‘ocular surface’, which yielded 189 documents. Further references were obtained by searching for keywords ‘ACE2’ AND ‘conjunctiv*’ OR ‘cornea’ OR ‘ocular surface’, which yielded two documents; and ‘Angiotensin converting enzyme‐2’ AND ‘conjunctiv*’ OR ‘cornea’ OR ‘ocular surface’, which yielded five documents.
The abstracts of all these documents were read, and those dealing with any coronavirus and the ocular surface tissues or conjunctivitis were downloaded and reviewed. In addition, the references contained in these downloaded documents were examined for other sources of information that would be pertinent to the review. In cases where documents were available with abstracts only in English but the full paper only in Chinese, if the abstract was thought to be pertinent, the paper was translated initially by Google Translate (https://translate.google.com.au) and then by Dr Renxun Chen, (University of New South Wales) for further review.
Coronaviruses
Coronaviruses are a relatively large group of viruses that can cause diseases in humans and other animals. Human coronaviruses hCoV‐229E, OC43, NL63, and HKU1 typically cause mild respiratory diseases, are seasonal (peaking in the winter) and have been around for decades. More recently, coronaviruses which can cause fatal infections in humans – SARS‐CoV in 2002–2003, MERS‐CoV in 2012 10 and of course SARS‐CoV‐2 in 2019 – have emerged. Coronaviruses also cause large economic losses as they can cause severe diseases in farm animals such as cows 11 and chickens12, 13 as well as domestic animals such as cats.14, 15 All viruses need to bind (adhere) to host cells, as the first step in their invasion of cells and subsequent replication. Coronaviruses use the spike protein that protrudes through their lipid envelope to bind to various receptors on host cells. 3
Binding of coronaviruses to host cells, and presence of receptors in ocular surface tissue
SARS‐CoV‐2 uses angiotensin converting enzyme‐2 (ACE2) as its receptor on human cells, and binding to this facilitates infection. 16 The mammalian serine protease TMPRSS2 or the protease Furin (also known as Paired basic Amino acid Cleaving Enzyme) appear to prime the spike protein for interaction with ACE2.17, 18 SARS‐CoV also binds to the cell‐surface protein ACE2 and this binding is required for the virus to infect cells. 19 The binding of SARS‐CoV‐2 to ACE2 is enhanced compared to that of SARS‐CoV due to several changes in the gene and hence amino acid sequence of the spike protein. 20 SARS‐CoV also binds to CD209 (dendritic cell [DC]‐specific intercellular adhesion molecule [ICAM‐3] grabbing non‐integrin; DC‐SIGN) and CD209L (L‐SIGN).21, 22, 23 MERS‐CoV binds to the cell‐surface molecule CD26 (DPP‐4) and this is facilitated by the cofactor CD66e (CEACAM5). 24
For the less pathogenic human coronaviruses, hCoV‐229E uses CD13 to infect cells, 25 OC43 and HKU1 bind to 9‐O‐acetylated sialic acid (Neu5,9Ac2), 26 and NL63 uses ACE2 to bind to host cells. 27 NL63 and SARS‐CoV first anchor to cells via heparan sulfate proteoglycans before interacting with the ACE2 entry receptor,19, 27, 28 but this binding alone is not sufficient for infection. 19 In fact many viruses, not just coronaviruses, utilise heparan sulfate on cell surfaces for initial binding. 29 Feline infectious peritonitis virus uses CD13 (aminopeptidase N) or CD209 to bind to its host cells. 15 Bovine coronavirus binds to 9‐O‐acetylated sialic acid on its host cells. 30
Table 1 presents a comparison of receptors for SARS‐CoV‐2, SARS‐CoV and MERS‐CoV on ocular surface and lung cells.31, 32, 33, 34, 35, 36, 37, 38, 39
Table 1.
Comparison of SARS‐CoV‐2, SARS‐CoV and MERS‐CoV receptors on ocular surface and lung
| Coronaviruses | Receptor | Role in human CoV disease | Ocular surface (cell types) | Lung |
|---|---|---|---|---|
|
SARS‐CoV SARS‐CoV‐2 |
ACE2 | Host cell receptor and essential for infection | + (conjunctival epithelium and fibroblasts; corneal epithelium) 31 | + (airway epithelia)32, 33 |
| TMPRSS2 | Primes spike protein for binding to ACE2 | – | + (airway epithelium) 34 | |
| CD209 | Cell‐to‐cell viral transfer | + (corneal dendritic cells) 35 | + (alveola macrophages) 36 | |
| MERS‐CoV | CD26 | Host cell receptor and essential for infection | +/− (conjunctival vascular endothelium) 37 | + (lung epithelia and endothelia) 38 |
| CD66e | Co‐receptor | +/− (palpebral conjunctiva) 39 | + (bronchial and alveolar epithelium) 32 |
+: the receptor has been found, −: there are no reports of the receptor on the ocular surface, +/−: found in tissue but only on non‐virally‐mediated inflamed tissue.
Expression of the gene for ACE2 has been shown in corneal and conjunctival epithelial cells, and preliminary evidence has been presented for the presence of the protein associated with these cells. 40 The isolated surface protein S240 of SARS‐CoV can bind to conjunctival epithelial and fibroblast cells and corneal epithelial cells, with this binding inhibited by soluble ACE2, indicating that the binding was being mediated through cell‐surface ACE2. 31 However, the authors did note that ‘the amount of ACE2 expressed in conjunctival and corneal cells and tissues (was) less than that in heart, lung tissues and Vero E6 cells’, and was approximately 50 per cent that of Vero E6 cells. 31 Another paper provided evidence of expression of mRNA for ACE2 in corneal epithelium with no evidence provided of mRNA from the conjunctiva. 41 The normalised expression of ACE2 in the corneal epithelial mRNA was only 20‐28 units, compared to > 400 units in the testes, > 200 units in the small intestine terminal ileum and > 100 units in the heart left ventricle. 41 The previously mentioned serine protease TMPRSS2 or Furin, which appear to prime the spike protein, had not been reported in tears or on corneal or conjunctival cells. However, 15 per cent of superficial conjunctival cells have been shown to have “greater‐than‐zero expression” of the gene for TMPRSS2, three per cent of cells in superficial conjunctiva and one per cent of limbal superficial cells have “greater‐than‐zero expression” of genes of both TMPRSS2 and ACE2. The mean level of expression of mRNA for ACE2 or TMPRSS2 in any ocular tissue was approximately 0.6 per cent, whereas the mean level of expression was greater (1.2–1.4 per cent) in most other tissues (such as nasal cavity, lung parenchyma, ileum, colon, heart) examined. 42
CD209 can be found on human corneal dendritic cells. 35 CD26 is not expressed in normal conjunctival tissue, and has only been found, and then only weakly expressed, in vascular endothelial cells of conjunctival tissue from biopsies of vernal conjunctivitis patients. 37 The only report of CD66e in the conjunctiva was from patients with trachoma who had gene expression in their upper palpebral conjunctiva. 39 There are no reports of CD26 or CD66e in cornea or tears. CD13 has not been reported on conjunctival or corneal epithelial cells, but has been found on human corneal keratocytes. 43 9‐O‐acetylated sialic acid has been found in human tears and on human corneal mucin. 44 Heparan sulfate has been found on human cornea and conjunctiva cells.45, 46
In summary, the ocular surface does possess the ubiquitous viral receptor heparan sulfate, which can facilitate initial viral attachment. However, this is not sufficient for coronavirus infection. Furthermore, lactoferrin that is present in high concentrations in tears (2 mg/ml) 47 prevents viral attachment to heparan sulfate. 19 The ocular surface appears to possess the SARS‐CoV‐2, SAR‐CoV and NL63 receptor ACE2, but may not possess the TMPRSS2 or Furin proteins, which is required for the spike protein of SARS‐CoV‐2 to bind to ACE2.
Furthermore, apart from 9‐O‐acetylated sialic acid, the other co‐receptors for coronaviruses (CD209, CD26, CD13, CD66e), have been found either in fibroblasts and dendritic cells that lie in tissue under the surface corneal and conjunctival epithelial cells, or have not been reported in ocular tissues. It is possible that the 9‐O‐acetylated sialic acid associated with proteins in tears can act as a decoy receptor, binding to the viruses and preventing them binding to cell‐associated 9‐O‐acetylated sialic acid. 44 Therefore, the evidence to date suggests that coronaviruses are unlikely to bind to ocular surface cells to initiate infection.
Animal studies of human coronavirus infection
Using animal models can help to determine whether the eye can become infected and the consequence of application of live virus to the eye. Unfortunately, most studies have not been designed specifically to examine the role of the eye in the disease process. Some studies have inoculated monkeys with SARS‐CoV intranasally and by topical application to the conjunctiva, and often also via their trachea.48, 49, 50 While the monkeys developed pneumonia, the role of the conjunctival inoculation cannot be analysed separately from the inoculation via the other routes.
However, an as yet non‐peer‐reviewed paper has been made available that directly compares inoculation of SARS‐CoV‐2 of rhesus macaque monkeys via their conjunctiva, trachea or stomach. 51 While the one monkey that received SARS‐CoV‐2 via their trachea had weight loss, the two monkeys that were inoculated via their conjunctiva had no weight loss. SARS‐CoV‐2 RNA was transiently found in the conjunctiva after one day only, and only in conjunctiva‐infected monkeys. For the conjunctiva‐infected and trachea‐infected animals, viral RNA could be found in nasal and throat swabs over the course of seven days. Interestingly, the conjunctiva‐infected animal on day 14 had the highest antibody levels to SARS‐CoV‐2.
The authors concluded that conjunctival inoculation resulted in a mild lung infection compared to the trachea inoculation. 51 Unfortunately, no histology was performed on the eye during the infection, and given the very transient level of virus found in the conjunctival samples, infection or inflammation probably did not occur. If there was infection of the ocular surface, then conjunctivitis and perhaps keratitis would be expected to be manifestations of the disease. This study does suggest, at least for relatively large inocula (the authors used 1 × 106 50 per cent tissue‐culture infectious doses), that viral particles on the eye can travel to the lung but that they are either reduced in their virulence or the numbers that reach the lung are very low, and so the resulting infection was very mild.
Association of coronaviruses with conjunctivitis
There has been one report of a woman who presented with rhinorrhoea, cough, nasal congestion, unilateral conjunctivitis, but no fever (although the subject had taken over‐the‐counter antipyretic medication) as the initial presentation of COVID‐19. 52 The case history indicates that the patient had returned from a vacation in the Philippines and had transited through San Francisco on her return to Canada. She had swum in the sea and hotel swimming pools on vacation, and a public swimming pool once on her return to Canada. Upon presentation to an ophthalmology clinic she was initially diagnosed with presumed herpetic keratoconjunctivitis, which was subsequently changed to presumed epidemic keratoconjunctivitis after initial antiviral medications did not appear to be affecting the disease. The conjunctivitis remained unilateral during the seven days of the investigation.
Seven days after the initial symptoms the patient was tested for SARS‐CoV‐2 after changes to screening recommendations occurred for new arrivals into Canada, and was positive. A retest of a conjunctival swab (which had been negative for chlamydia, gonorrhoea, and bacterial culture) taken five days after initial symptoms was reported to be weakly positive for viral RNA. 52
In a separate case report, 53 a 65‐year‐old woman who had returned to Italy from Wuhan in China was admitted to hospital one day after noticing symptoms and six days after returning to Italy. She presented with non‐productive cough, sore throat, coryza and bilateral conjunctivitis. Conjunctivitis persisted until day 16 after symptom onset and ocular swabs were positive for viral RNA up until 21 days after hospital admission. Interestingly, five days after it became undetectable in ocular swabs, RNA for SARS‐CoV‐2 was again present upon polymerase chain reaction (PCR), but only for this one day after which it was again undetectable. SARS‐CoV‐2 was able to be grown in cell culture from the first swab but no other swabs were submitted for viral culture. 52 A 65‐year‐old Iranian diabetic male presented with symptoms of a burning eye and discharge, with no fever, cough or other symptoms. He had no recent history of travel. An initial diagnosis of viral conjunctivitis was made. 54 Two days after initial presentation he reported with sudden‐onset fever and a swab of his nasopharynx was positive for SARS‐CoV‐2 by PCR. 54
In reports of 99 55 or 140 56 patients with SARS‐CoV‐2 from Wuhan China – the initial site of infection that resulted in the pandemic – conjunctivitis was not noted as a sign or symptom of the disease. Also, conjunctivitis was not noted as a sign or symptom in 32 confirmed COVID‐19 patients examined outside of Wuhan in China. 57 Of 17 COVID‐19 patients recruited in a prospective study in Singapore, none demonstrated ocular signs or symptoms of conjunctivitis at initial recruitment into the study, 58 but one developed conjunctival infection and chemosis during their hospital stay. 58 Only two patients of 72 confirmed COVID‐19 cases examined at Tongji Hospital in Shanghai were diagnosed with conjunctivitis (2.8 per cent). 59 A report of the WHO‐China Joint Mission which summarised 55,924 cases of COVID‐19 reported that only 0.8 per cent of patients had signs of conjunctival ‘congestion’. 60
Three patients out of 30 diagnosed with COVID‐19 pneumonia in Wuhan have been reported as having conjunctivitis (10 per cent). 61 One of these patients reported having red eyes, itching and blurred vision three days prior to being diagnosed with COVID‐19. Another of these patients, who had uveitis five years prior to COVID‐19, had a mild dry cough and fatigue two days prior to noticing binocular redness with foreign body sensation, with conjunctivitis confirmed by slitlamp biomicroscopy. The third patient developed conjunctivitis three days after being admitted to hospital with COVID‐19. 61
Thirty‐eight patients at Yichang Central People's Hospital China who were diagnosed with COVID‐19 had ocular examinations which resulted in 12 of these being diagnosed with epiphora, conjunctival congestion, or chemosis (32 per cent). 62 All of these patients were diagnosed with either moderate (4/12) or severe to critical (8/12) COVID‐19, and only one of the patients reported ocular symptoms (epiphora) as a first sign of possible COVID‐19. 62
A member of the national expert panel on pneumonia reported that he believed he had become infected with SARS‐CoV‐2 during an inspection of a hospital in Wuhan via his eyes, which had become red ‘several days’ prior to the onset of pneumonia. 63 However, the statement that the conjunctivitis occurred ‘several days’ before the onset of pneumonia has been refuted by Peng and Zhou 64 who refer to the original report as stating that conjunctivitis was noticed just two to three hours before development of fever and catarrhal symptoms, and that conjunctivitis probably occurred after COVID‐19 had developed into pneumonia.
In the case of infection with SARS‐CoV or MERS‐CoV, reports and reviews have not identified conjunctivitis as a sign or symptom, even in cases diagnosed early in their disease.65, 66, 67, 68 For disease caused by NL63, in a review of 15 studies which had a combined number of cases of over 7,500, 69 only a single study from France reported the appearance of conjunctivitis, and then conjunctivitis was seen in 17 per cent of the 300 cases. 70 NL63 was initially isolated from a child with both bronchiolitis and conjunctivitis, but the other seven cases in that first report did not have conjunctivitis as a noted sign or symptom. 71 Infections with HKU1 have not produced any associated conjunctivitis,72, 73 and while there is a report showing that a patient with Kawasaki disease infected with OC43/HKU1 had conjunctival injection, 74 this conjunctivitis was most likely due to the underlying Kawasaki disease.
It appears that (kerato)conjunctivitis is a rare manifestation of human coronavirus disease, and this was also the conclusion of Sun et al., who stated ‘The eye is rarely involved in human CoVs infection, conjunctivitis is quite rare in patients with SARS‐CoV and 2019‐nCoV (SARS‐CoV‐2) infection’. 75 However, all cases of (kerato)conjunctivitis, especially those with any associated upper respiratory tract symptoms (however mild), should be considered as potential COVID‐19 cases. In most cases that have reported conjunctivitis associated with coronavirus infection, the studies have been of patients in hospitals who would likely have presented with severe forms of COVID‐19. However, as COVID‐19 patients have been reported to have viral RNA detected in their plasma, and the case of keratoconjunctivitis 52 had a weak positive test for SARS‐CoV‐2 in a conjunctival swab, it is possible that the virus can appear at the ocular surface.
Detection of coronavirus at the ocular surface
SARS‐CoV‐2, SARS‐CoV and other coronaviruses may be able to appear at the ocular surface as the result of: (1) the conjunctiva being the direct inoculation site of virus from infected droplets; (2) migration via the nasolacrimal duct during upper respiratory tract infection; or (3) exudation through conjunctival vessels during the disease. The present authors have dealt with (1) in the section of adhesion of these viruses to ocular surface tissue, and concluded that this is an unlikely occurrence. In this section, the question as to whether the viruses can be found at the ocular surface and in tears is examined.
A patient with keratoconjunctivitis who was later confirmed to have COVID‐19 had SARS‐CoV‐2 RNA in a two‐day‐old conjunctival swab. 52 Also, a patient in Italy who had bilateral conjunctivitis as part of their first symptoms was reported to have RNA in ocular swabs for 21 days after onset of symptoms, which included conjunctivitis. 53 SARS‐CoV‐2 was grown from the ocular swab taken three days after onset of symptoms. 53 However, another report shows that another patient who developed conjunctival infection and chemosis during their stay in the hospital had no viral RNA in tears. 58
Most other studies have examined COVID‐19 patients who have not been reported to have ocular signs or symptoms. One study collected 64 tear samples using a Schirmer strip from 17 confirmed COVID‐19 patients and analysed the tears using PCR to detect viral RNA. 58 The samples were collected during three weeks of the infection in the patients. While viral RNA could be detected in all nasopharyngeal swabs, no virus was grown from the tear samples and no viral RNA could be detected, even from those patients with symptoms of upper respiratory tract infection. 58 The authors concluded ‘the hypothesis of the lacrimal duct as a viral conduit may not be true’. A patient who presented with conjunctivitis that was later diagnosed with COVID‐19 had viral RNA detected in two subsequent conjunctival swabs. 58
Another study collected tears and conjunctival secretions using a swab of the lower fornix. 76 The study included 21 patients with ‘common‐type’ and nine patients with ‘severe‐type’ COVID‐19. Fifty‐eight conjunctival swab samples from 20 common‐type patients and nine severe‐type patients were all negative. Two conjunctival swabs of one common‐type patient yielded viral RNA upon PCR (three per cent). In contrast, 55 of 60 sputum samples were positive upon PCR (92 per cent). 76 A third study examined 63 confirmed COVID‐19 patients and four suspected patients by PCR for viral RNA of conjunctival swabs. 77 Only one conjunctival sample was confirmed positive by PCR, and the only patient with conjunctivitis was negative. 77
Ocular surfaces have also been sampled from patients infected with SARS‐CoV. One study used both PCR and viral culture of tears collected from the deep lower fornix using a swab and conjunctival scrapings of the lower palpebral conjunctiva of 17 confirmed SARS‐CoV cases. 78 That study was unable to detect virus using PCR and no virus was grown from any sample. 78
A second study used PCR to detect SARS‐CoV RNA in 36 tear samples from probable (serology confirmed) or suspect cases of SARS, collected by everting the eyelids and sweeping the inferior fornixes of both eyes with sterile cotton tipped swabs without topical anaesthesia. 79 Three of the eight probable cases were positive for viral RNA in their samples, while none of the 28 suspect cases were positive. 79 The three positive cases had tears collected within nine days of onset of their illness, whereas the five negative cases had samples collected on average 19.4 days after onset of symptoms.
Examining all of the studies that have attempted to isolate live virus or analysed ocular samples for viral RNA demonstrates that, at any stage of disease, viral RNA was detected in only five per cent of ocular surface swabs (9/178); in other words, 95 per cent of samples did not yield viral RNA, and, where attempted, no sample grew virus. As is acknowledged by Xia et al., 76 PCR can yield false positive and false negative data: false positive data due to sample contamination and false negative data due to sample degradation. Given the low number of positive samples and the high number of negative samples, the present authors feel that the data demonstrate that it is very unlikely that SARS‐CoV‐2 is present at the ocular surface during coronavirus infection. Thus, the hypotheses that the virus could travel from the nasopharynx or through the conjunctival capillaries during infection are probably incorrect.
Summary
Human coronaviruses bind to specific receptors on host cells. Binding of SARS‐CoV‐2 and SARS‐CoV to ACE2 is required for initiation of infection. There is some preliminary evidence for ACE2 expression on corneal and conjunctival cells, but most of the other receptors known to bind to coronaviruses appear to be found only on fibroblasts and dendritic cells that are found under the surface epithelial layers of the ocular surface. Lactoferrin in tears can inhibit coronavirus binding, as may decoy receptors such as 9‐O‐acetylated sialic acid on tear glycoproteins. Animal studies on human coronaviruses have not focused on the role of ocular surface binding in the infection process, apart from one study that showed conjunctival infection could lead to mild signs and symptoms of pneumonia, but only transient association of SARS‐CoV‐2 with the conjunctiva. While coronavirus infection is rarely associated with conjunctivitis, there have been occasional findings of conjunctivitis in confirmed COVID‐19 patients. Similarly, coronaviruses have been rarely isolated from tears or conjunctival swabs.
Further research
The expression of coronavirus receptors on ocular surface cells needs further confirmatory investigation. It would also be of interest to examine whether contact lens wear or ocular surface diseases such as dry eye disease are associated with increased expression of these receptors. The ability of tears to inhibit binding of coronaviruses to ocular surface cells is another area for research. This may identify substances that can be translated into new prophylaxis treatments to reduce the spread of coronaviruses in the environment.
Further studies, using animal models, on the role of contamination of the ocular surface on progression of the disease are urgently needed. These studies, as well as further studies with human cases of disease, will also help to definitively identify the virus at the ocular surface. As only one study has been able to grow SARS‐CoV‐2 from ocular swabs and then only reported growth early in the disease and did not attempt to grow viruses from subsequent ocular surface swabs, 53 studies should also then examine whether any ocular surface‐associated viruses are infective. Epidemiological studies and case reports should include analysis of ocular complications during coronavirus infection.
Clinical relevance
The conclusions from this review are clinically relevant both in terms of their implications for clinical practice, and in the wider education of patients. The nature of ocular examination demands that the eye‐care practitioner and patient are in close proximity to one another. Given the main mode of transmission of the virus is thought to be via person‐to‐person contact through respiratory droplets transmission (airborne or through direct contact), 80 it is unsurprising that ophthalmic practice has been significantly affected by the COVID‐19 pandemic.
Many countries have temporarily stopped all routine appointments, moving to a service offering only emergency care during the height of the pandemic. Even with this precaution, in the case of a presumed ocular emergency, following initial remote consultation by phone or other electronic means, a face‐to‐face examination may still be deemed necessary. For these situations, eye‐care practitioners have been advised to take significant precautions to protect themselves and their patients from potential viral transmission. Five steps were recently summarised in relation to contact lens practice in particular,9, 81 including ensuring the patient is well, wearing personal protective equipment (PPE),81, 82, 83, 84, 85 installation of a protective shield on the slitlamp biomicroscope, 7 and thorough sanitisation of hands and all surfaces pre‐ and post‐visit. The precautions listed above are necessary to limit exposure of both the patient and eye‐care practitioner to the virus, and should remain in place until such time that the pandemic has been declared over or other measures can be implemented.
The conclusions shared in this review provide evidence and reassurance that the eye itself is unlikely to be a route for transmission, although this does not change the level of care required in clinical situations at present, given the potential to transmit the virus through airborne droplets and direct contact from the mouth and nose. One area that should be remembered, and already covered in this review, is that of the potential, albeit rare, for (kerato)conjunctivitis to present as the first sign of COVID‐19. All eye‐care practitioners must bear this in mind when triaging patients and considering how best to review, and potentially examine, or refer, a patient in this situation.
Given the need for contact lens wearers to touch their face and eyes on application and removal of their contact lenses, it is understandable that questions have been raised about the safety of continuing with contact lens use during the pandemic, as discussed in a recent paper by the present authors. 8 Despite the current review indicating that the eye is an unlikely site for SARS‐CoV‐2 infection, scrupulous contact lens hygiene practices should continue to be advocated, along with use of correct wear, care, cleaning and replacement of lenses and lens cases. This advice is true for all contact lens wearers in normal times, but especially relevant during the current pandemic, where access to routine eye care may be limited. Further, and in accordance with WHO and Centers for Disease Control recommendations,86, 87 it is important to remind all patients, regardless of their use of vision correction, to avoid touching their nose, mouth or eyes with unwashed hands.
Conclusion
Precautions employed by both eye‐care practitioners and patients during the COVID‐19 pandemic remain necessary to minimise viral transmission via person‐to‐person contact. It is reassuring to recognise that current evidence suggests the virus is unlikely to bind to the ocular surface to initiate infection, and that the ocular manifestations such as conjunctivitis and presence of SARS‐CoV‐2 in tears have so far only been found rarely and primarily in people with confirmed, symptomatic COVID‐19.
ACKNOWLEDGEMENTS
The authors wish to thank Dr Renxun Chen, School of Chemistry, The University of New South Wales, Sydney, Australia for help with translation of articles; and Dr Chau‐Minh Phan, Centre for Ocular Research & Education, School of Optometry and Vision Science, University of Waterloo, Canada for drawing of the coronavirus.
REFERENCES
- 1. Wertheim JO, Chu DKW, Peiris JSM et al. A case for the ancient origin of coronaviruses. J Virol 2013; 87: 7039–7045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Woo PCY, Lau SKP, Lam CSF et al. Discovery of seven novel mammalian and avian coronaviruses in the genus deltacoronavirus supports bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavi. J Virol 2012; 86: 3995–4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol 2015; 1282: 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . WHO Director‐General's opening remarks at the mission briefing on COVID‐19. 2020. [Cited 18 Apr 2020.] Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 5. World Health Organization . Coronavirus disease 2019 (COVID‐19) situation report – 89. 2020. [Cited 18 Apr 2020.] Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200418-sitrep-89-covid-19.pdf?sfvrsn=3643dd38_2.
- 6.World Health Organization. Coronavirus disease 2019. Geneva: World Health Organization, 2020; 2633.
- 7. Lai THT, Tang EWH, Chau SKY et al. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefe's Arch Clin Exp Ophthalmol 2020; 258: 1049–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones L, Walsh K, Willcox M et al. The COVID‐19 pandemic: important considerations for contact lens practitioners. Cont Lens Anterior Eye 2020. 10.1016/j.clae.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zeri F, Naroo SA. Contact lens practice in the time of COVID‐19. Cont Lens Anterior Eye 2020. 10.1016/j.clae.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Boileau MJ, Kapil S. Bovine coronavirus associated syndromes. Vet Clin North Am Food Anim Pract 2010; 26: 123–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hauck R, Gallardo RA, Woolcock PR et al. A coronavirus associated with runting stunting syndrome in broiler chickens. Avian Dis 2016; 60: 528–534. [DOI] [PubMed] [Google Scholar]
- 13. Bande F, Arshad SS, Omar AR et al. Pathogenesis and diagnostic approaches of avian infectious bronchitis. Adv Virol 2016; 2016: 4621659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hök K. Demonstration of feline infectious peritonitis virus in conjunctival epithelial cells from cats. APMIS 1989; 97: 820–824. [DOI] [PubMed] [Google Scholar]
- 15. Van Hamme E, Desmarets L, Dewerchin HL et al. Intriguing interplay between feline infectious peritonitis virus and its receptors during entry in primary feline monocytes. Virus Res 2011; 160: 32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yan R, Zhang Y, Li Y et al. Structural basis for the recognition of SARS‐CoV‐2 by full‐length human ACE2. Science 2020; 367: 1444–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoffmann M, Kleine‐Weber H, Schroeder S et al. SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020; 181: 271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoffmann M, Kleine‐Weber H, Pöhlmann S. A multibasic cleavage site in the spike protein of SARS‐CoV‐2 is essential for infection of human lung cells. Cell Press 2020; 10.1016/j.molcel.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lang J, Yang N, Deng J et al. Inhibition of SARS pseudovirus cell entry by lactoferrin binding to heparan sulfate proteoglycans. PLoS One 2011; 6: e23710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shang J, Ye G, Shi K et al. Structural basis of receptor recognition by SARS‐CoV‐2. Nature 2020. 10.1038/s41586-020-2179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jeffers SA, Tusell SM, Gillim‐Ross L et al. CD209L (L‐SIGN) is a receptor for severe acute respiratory syndrome coronavirus. Proc Natl Acad Sci U S A 2004; 101: 15748–15753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shih Y‐P, Chen C‐Y, Liu S‐J et al. Identifying epitopes responsible for neutralizing antibody and DC‐SIGN binding on the spike glycoprotein of the severe acute respiratory syndrome coronavirus. J Virol 2006; 80: 10315–10324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yang Z‐Y, Huang Y, Ganesh L et al. pH‐dependent entry of severe acute respiratory syndrome coronavirus is mediated by the spike glycoprotein and enhanced by dendritic cell transfer through DC‐SIGN. J Virol 2004; 78: 5642–5650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Arabi YM, Balkhy HH, Hayden FG et al. Middle east respiratory syndrome. N Engl J Med 2017; 376: 584–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yeager CL, Ashmun RA, Williams RK et al. Human aminopeptidase N is a receptor for human coronavirus 229E. Nature 1992; 357: 420–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hulswit RJG, Lang Y, Bakkers MJG et al. Human coronaviruses OC43 and HKU1 bind to 9‐O‐acetylated sialic acids via a conserved receptor‐binding site in spike protein domain A. Proc Natl Acad Sci U S A 2019; 116: 2681–2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Milewska A, Nowak P, Owczarek K et al. Entry of human coronavirus NL63 into the cell Aleksandra. J Virol 2018; 92: e01933‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Milewska A, Zarebski M, Nowak P et al. Human coronavirus NL63 utilizes heparan sulfate proteoglycans for attachment to target cells. J Virol 2014; 88: 13221–13230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cagno V, Tseligka ED, Jones ST et al. Heparan sulfate proteoglycans and viral attachment: true receptors or adaptation bias? Viruses 2019; 11: 596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schwegmann‐Weßels C, Herrler G. Sialic acids as receptor determinants for coronaviruses. Glycoconj J 2006; 23: 51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sun Y, Liu L, Pan X et al. Mechanisms of the action between the SARS‐Cov S440 protein and the ACE2 receptor in eyes. Int J Ophthalmol 2006; 6: 783–786. [Google Scholar]
- 32. Klaile E, Klassert TE, Scheffrahn I et al. Carcinoembryonic antigen (CEA)‐related cell adhesion molecules are co‐expressed in the human lung and their expression can be modulated in bronchial epithelial cells by non‐typable Haemophilus influenzae, Moraxella catarrhalis, TLR3, and type I and II int. Respir Res 2013; 14: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hamming I, Timens W, Bulthuis MLC et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol 2004; 203: 631–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Donaldson SH, Hirsh A, Li DC et al. Regulation of the epithelial sodium channel by serine proteases in human airways. J Biol Chem 2002; 277: 8338–8345. [DOI] [PubMed] [Google Scholar]
- 35. Mayer WJ, MacKert MJ, Kranebitter N et al. Distribution of antigen presenting cells in the human cornea: correlation of in vivo confocal microscopy and immunohistochemistry in different pathologic entities. Curr Eye Res 2012; 37: 1012–1018. [DOI] [PubMed] [Google Scholar]
- 36. Tailleux L, Pham‐Thi N, Bergeron‐Lafaurie A et al. DC‐SIGN induction in alveolar macrophages defines privileged target host cells for mycobacteria in patients with tuberculosis. PLoS Med 2005; 2: e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Abu El‐Asrar AM, Struyf S, Al‐Kharashi SA et al. Expression of T lymphocyte chemoattractants and activation markers in vernal keratoconjunctivitis. Br J Ophthalmol 2002; 86: 1175–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zou H, Zhu N, Li S. The emerging role of dipeptidyl‐peptidase‐4 as a therapeutic target in lung disease. Expert Opin Ther Targets 2020; 24: 147–153. [DOI] [PubMed] [Google Scholar]
- 39. Burton MJ, Rajak SN, Hu VH et al. Pathogenesis of progressive scarring trachoma in Ethiopia and Tanzania and its implications for disease control: two cohort studies. PLoS Negl Trop Dis 2015; 9: e0003763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lin L, Yan S, Xin P et al. Expression of SARS coronavirus S protein functional receptor‐angiotensin‐converting enzyme 2 in human cornea and conjunctiva. Chin Ophthalmic Res 2004; 22: 561–564. [Google Scholar]
- 41.Sun K, Gu L, Ma L et al. Atlas of ACE2 gene expression in mammals reveals novel insights in transmission of SARS‐Cov‐2. bioRxiv 2020. 10.1101/2020.03.30.015644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sungnak W, Huang N, Bécavin C et al. SARS‐CoV‐2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020. 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Choong PF, Mok PL, Cheong SK et al. Mesenchymal stromal cell‐like characteristics of corneal keratocytes. Cytotherapy 2007; 9: 252–258. [DOI] [PubMed] [Google Scholar]
- 44. Argüeso P, Sumiyoshi M. Characterization of a carbohydrate epitope defined by the monoclonal antibody H185: Sialic acid O‐acetylation on epithelial cell‐surface mucins. Glycobiology 2006; 16: 1219–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Akhtar J, Tiwari V, Oh MJ et al. HVEM and nectin‐1 are the major mediators of herpes simplex virus 1 (HSV‐1) entry into human conjunctival epithelium. Investig Ophthalmol Vis Sci 2008; 49: 4026–4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Huang AJW, Li DQ, Li CH et al. Modulation of corneal vascularization. Ocul Surf 2005; 3: S190–S193. [DOI] [PubMed] [Google Scholar]
- 47. Willcox MDP. Tear film, contact lenses and tear biomarkers. Clin Exp Optom 2019; 102: 350–363. [DOI] [PubMed] [Google Scholar]
- 48. Kuiken T, Fouchier RAM, Schutten M et al. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet 2003; 362: 263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lawler JV, Endy TP, Hensley LE et al. Cynomolgus macaque as an animal model for severe acute respiratory syndrome. PLoS Med 2006; 3: 677–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fouchier RAM, Kuiken T, Schutten M et al. Koch's postulates fulfilled for SARS virus. Nature 2003; 423: 240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Deng W, Bao L, Gao H et al. Ocular conjunctival inoculation of SARS‐CoV‐2 can cause mild COVID‐19 in Rhesus macaques. bioRxiv 2020. 10.1101/2020.03.13.990036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cheema M, Aghazadeh H, Nazarali S et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID‐19). Can J Ophthalmol 2020. 10.1016/j.jcjo.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Colavita F, Lapa D, Carletti F et al. SARS‐CoV‐2 isolation from ocular secretions of a patient with COVID‐19 in Italy with prolonged viral RNA detection. Ann Intern Med 2020. 10.7326/M20-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khavandi S, Tabibzadeh E, Naderan M et al. Corona virus disease‐19 (COVID‐19) presenting as conjunctivitis: atypically high‐risk during a pandemic. Cont Lens Anterior Eye 2020. 10.1016/j.clae.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chen N, Zhou M, Dong X et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang JJ, Dong X, Cao YY et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy 2020. 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 57. Zhu W, Xie K, Lu H et al. Initial clinical features of suspected coronavirus disease 2019 in two emergency departments outside of Hubei, China. J Med Virol 2020. 10.1002/jmv.25763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Seah IYJ, Anderson DE, Kang AEZ et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID‐19) patients. Ophthalmology 2020. 10.1016/j.ophtha.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhang X, Chen X, Chen L et al. The evidence of SARS‐CoV‐2 infection on ocular surface. Ocul Surf 2020. 10.1016/j.jtos.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. World Health Organization . Report of the WHO‐China joint mission on coronavirus disease 2019 (COVID‐19). 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- 61. Ye Y, Song Y, Yan M et al. Novel coronavirus pneumonia combined with viral conjunctivitis: three cases report. Zhonghua Yan Ke Za Zhi 2020; 38: 242–247. [Google Scholar]
- 62. Wu P, Duan F, Luo C et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID‐19) in Hubei Province, China. JAMA Ophthalmol 2019; 2020: 10–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Lu CW, Liu XF, Jia ZF. 2019‐nCoV transmission through the ocular surface must not be ignored. Lancet 2020; 395: e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Peng Y, Zhou YH. Is novel coronavirus disease (COVID‐19) transmitted through conjunctiva? J Med Virol 2020. 10.1002/jmv.25753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Chan JFW, Lau SKP, To KKW et al. Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS‐like disease. Clin Microbiol Rev 2015; 28: 465–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hui DS, Wong PC, Wang C. SARS: clinical features and diagnosis. Respirology 2003; 8: S20–S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hui DSC, Zumla A. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am 2019; 33: 869–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Fan CK, Yieh KM, Peng MY et al. Clinical and laboratory features in the early stage of severe acute respiratory syndrome. J Microbiol Immunol Infect 2006; 39: 45–53. [PubMed] [Google Scholar]
- 69. Abdul‐Rasool S, Fielding BC. Understanding human coronavirus hCoV‐NL63. Open Virol J 2010; 4: 76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Vabret A, Mourez T, Dina J et al. Human coronavirus NL63, France. Emerg Infect Dis 2005; 11: 1225–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Van Der Hoek L, Pyrc K, Jebbink MF et al. Identification of a new human coronavirus. Nat Med 2004; 10: 368–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Esper F, Weibel C, Ferguson D et al. Coronavirus HKU1 infection in the United States. Emerg Infect Dis 2006; 12: 775–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Kanwar A, Selvaraju S, Esper F. Human coronavirus‐HKU1 infection among adults in Cleveland, Ohio. Open Forum Infect Dis 2017; 4: ofx052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Giray T, Biçer S, Küçük Ö et al. Four cases with Kawasaki disease and viral infection: aetiology or association? Le Infez Med 2016; 4: 340–344. [PubMed] [Google Scholar]
- 75. Sun C, Wang Y, Liu G et al. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Preprints 2020: 2020030271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Xia J, Tong J, Liu M et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS‐CoV‐2 infection. J Med Virol 2020; 92: 589–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zhou Y, Zeng Y, Tong Y et al. Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctiva. medRxiv 2020. 10.1101/2020.02.11.20021956. [DOI] [Google Scholar]
- 78. Chan WM, Yuen KSC, Fan DSP et al. Tears and conjunctival scrapings for coronavirus in patients with SARS. Br J Ophthalmol 2004; 88: 968–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Loon SC, Teoh SCB, Oon LLE et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol 2004; 88: 861–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Centers for Disease Control and Prevention. How COVID‐19 spreads. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Ftransmission.html. [PubMed]
- 81. Centers for Disease Control and Prevention . Using personal protective equipment (PPE). 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html.
- 82. Otter JA, Donskey C, Yezli S et al. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J Hosp Infect 2016; 92: 235–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Public Health England . COVID‐19: infection prevention and control (IPC). 2020. Available at: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control.
- 84. Lian KY, Napper G, Stapleton FJ et al. Infection control guidelines for optometrists 2016. Clin Exp Optom 2017; 100: 341–356. [DOI] [PubMed] [Google Scholar]
- 85. Qiao C, Zhang H, He M et al. Symptomatic COVID‐19 Infection in Eye Professionals in Wuhan China. Ophthalmology 2020. 10.1016/j.ophtha.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. World Health Organization . Coronavirus disease (COVID‐19) advice for the public. 2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 87. Centers for Disease Control and Prevention . How to protect yourself & others. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html.


