Abstract
Early on, geriatricians in Israel viewed with increasing alarm the spread of coronavirus disease 2019 (COVID‐19). It was clear that this viral disease exhibited a clear predilection for and danger to older persons. Informal contacts began with senior officials from the country's Ministry of Health, the Israel Medical Association, and the country's largest health fund; this was done to plan an approach to the possible coming storm. A group was formed, comprising three senior geriatricians, a former dean, a palliative care specialist, and a lawyer/ethicist. The members made every effort to ensure that their recommendations would be practical while at the same time taking into account the tenets of medical ethics. The committee's main task was to think through a workable approach because intensive care unit/ventilator resources may be far outstripped by those requiring such care. Recommendations included the approach to older persons both in the community and in long‐term care institutions, a triage instrument, and palliative care. Patient autonomy was emphasized, with a strong recommendation for people of all ages to update their advance directives or, if they did not have any, to quickly draw them up. Considering the value of distributive justice, with respect to triage, a “soft utilitarian” approach was advocated with the main criteria being function and comorbidity. Although chronological age was rejected as a sole criterion, in the case of an overwhelming crisis, “biological age” would enter into the triage considerations, but only in the case of distinguishing between people with equal non–age‐related deficits. The guideline emphasized that no matter what, in the spirit of beneficence, anyone who fell ill must receive active palliative care throughout the course of a COVD‐19 infection but especially at the end of life. Furthermore, in the spirit of nonmaleficence, the frail, very old, and severely demented would be actively protected from dying on ventilation. J Am Geriatr Soc 68:1370‐1375, 2020.
Keywords: COVID‐19, triage, Israel national guidelines
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) crisis is challenging us to look after our older patients, in the community, in nursing homes, and in the hospital. This population and especially the old‐old, the frail, those with cognitive impairment, and patients experiencing significant comorbidity are the most vulnerable to the serious consequences of this infection. Their clinical vulnerability is potentially exacerbated by the social phenomenon of ageism, where people are discriminated against solely on the basis of their chronological age, and by discriminatory societal norms based solely on chronological age. In this difficult and urgent context, we offer the following guidelines, involving three stages: community/nursing home, triage, and posttriage.
This report is the result of deliberations by an ad hoc committee convened to offer assistance in drawing up relevant national clinical guidelines to policy makers of Israel's Ministry of Health (MoH), the Israel Medical Association, and Israel's four health funds (health maintenance organizations [HMOs]). The chair is a geriatrician with experience in academia, clinical care, and government. Members included a senior internist who had also been dean of one of Israel's medical schools and two other senior geriatricians, one the head of the Israel Geriatrics Society and the second the chief geriatrician of the largest of the country's four health funds (HMOs). An experienced family physician who is head of Israel's Palliative Care Association was part of the group as well as an ethicist and lawyer who is the past president of the Israel Gerontology Society. The group worked via a modified Delphi process to draft recommendations to the relevant bodies. During our discussions and related to decisions taken, committee members made every effort to keep in mind and balance the principles of medical ethics as expressed through the values of autonomy, beneficence, nonmaleficence, and distributive justice.
Although space does not allow a detailed description, Israel's healthcare system is well organized and publicly run and financed. For all legal residents, it provides almost all health care free at point of service within the family of national health services, such as those operating in Canada, the United Kingdom, and many other European jurisdictions.1 As well, Israeli academic medicine is robust, and the country offers a well‐developed set of services for older people.2, 3 At the date of this writing, with a population of 9 million, there are 16,589 cases with a relatively low case‐fatality rate of 31/1,000,000. (For comparison: Spain has 272,646 cases, with a case‐fatality rate of 584/1,000,00; United Kingdom has 233,151 cases, with a case‐fatality rate of 495/1,000,000; United States has 1,457,593 cases, with a case‐fatality rate of 263/1,000,000; and Canada has 73,401 cases, with a case‐fatality rate of 145/1,000,000.)
The impetus for the committee's formation was a concern that, as was being observed in many European countries, such as Italy, Spain, and France, Israel's modest per capita intensive care unit (ICU) capacity would be overwhelmed by new cases, many of them older persons. However, the committee took a holistic approach to the challenge, examining three phases: the “upstream” issues, the triage instrument itself, and “downstream” concerns. We continuously reminded ourselves that we were only considering what to do in a “worst‐case scenario” and that if ICU supply met demand, our triage recommendations would be moot.
COMMUNITY/LONG‐TERM CARE INSTITUTIONS (“UPSTREAM” CONCERNS)
It is important to underline how important it is, as best one can, to support older persons (and their caregivers) in the community, as well as those high‐risk residents in the various long‐term care institutions. General principles and recommendations were:
Considering the principle of beneficence, to identify and supply the basic needs of older people who are at home (food, medications, social isolation) or in a long‐term institution. Given that initially the MoH instructed everyone (other than “vital” workers) to stay home and that younger people not visit older parents/grandparents, the health funds and municipal social services must do their best to locate and follow up these people in the community, keeping in mind the stresses that long‐term quarantine can bring to bear and offerings ways to alleviate them.4
Should an older person fall ill in the community, especially with COVID‐19 symptoms, the person must be quickly assessed. If his/her clinical condition allows and he/she so wishes, he/she can be treated at home. The U.S. Centers for Disease Control and Prevention offers sensible guidelines to this end (https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/care-for-someone.html; accessed April 6, 2020). For those who develop dyspnea, vital signs and oxygen saturation should be measured when available, to determine whether a patient can be cared for at home or whether more intensive treatment is required. If feasible, home oxygen therapy should be offered, as well as specific medications that might be approved by the MoH for oral COVID‐19 treatment. It is important to ensure that medications for attendant comorbidities not be forgotten.
If oxygen saturation measurement is not readily available at home, for those short of breath, a respiratory rate greater than 20 breaths per minute may indicate a worsening condition. Furthermore, for those who deteriorate but yet still wish to remain at home and whose families are capable of caring for them in this context, home palliation should be arranged as well as support for family members and other informal caregivers.
Should care at home not be possible, a triage instrument (see below) can help direct the health services to arrange for the next appropriate step: further assessment at the emergency room (ER) or transfer to a palliative care unit.
In an effort to boost and support patient autonomy, all persons, whether symptomatic or not, and especially those at high risk are urged to review (or consider signing if they have not yet) a continuing power of attorney and/or advance directives according to the relevant legislation (Legal Capacity and Guardianship Law, 1962; The Patients' Rights Act, 1996; and/or the Dying Patient Act, 2005); this is to determine if they wish either aggressive or palliative care should they fall ill. If transferred to another facility, these documents should accompany the patient.
Only in the face of an overwhelming imbalance between the numbers of those who fall severely ill and the health system's ability to supply acute care (especially ICU/ventilator), triage would be utilized, at the same time making every effort to uphold the principles of distributive justice. Although largely not appropriate for those in the community (with the possible exception of those older persons receiving homemaker benefits according to criteria of the Community‐Based Long Term Care Act, which is part of the National Insurance Act of 1995),2 those living in a long‐term institution could have the triage instrument filled out with and/or for them even before any clinical need becomes apparent.
Patients in long‐term care institutions comprise an extremely high‐risk group. This due to the fact that most persons in such facilities are of advanced age, usually frail, and experience multiple comorbidity, often including dementia, which makes the likelihood of surviving ventilation low. Furthermore, the institutional nature of these dwellings exposes residents to a greater chance of being infected than had they been under home isolation. Principles of care in these institutions, along with a warning that things could change rapidly, are discussed elsewhere.5 It is most important that personal protective gear be offered to staff to prevent cross infection as well as to protect workers and their families. The MoH must show firm leadership and offer clear guidelines to help these severely stressed institutions. This process has already begun with https://www.jpost.com/israel-news/calling-in-the-calvary-israel-fights-coronavirus-analysis-623672 a carefully designed national plan now in action. More such aid is and will be needed.
As alluded to above, it must be kept in mind that COVID‐19 is not the only threat to older persons. We recommend that anyone with symptoms that under normal circumstances would bring them to acute medical attention (e.g., chest pain, severe abdominal pain, symptoms of transient ischemic attack/cerebrovascular accident) should immediately seek help by calling an ambulance. Anecdotal information from colleagues in both cardiology and neurology from one of Israel's foremost teaching hospitals suggests that this phenomenon is now being observed, with some patients waiting an inordinate time before seeking acute hospital care, much to their detriment; and this despite these services operating adequately.
TRIAGE
As alluded to above, in the spirit of ensuring distributive justice, the following section is only relevant should a severe imbalance develop between ICU/ventilator availability and the demand for it due to an upsurge in COVID‐19 pneumonia cases. Otherwise, care pathways should remain as is the case when there is no crisis. At the time of article revision (May 17, 2020), it was still not necessary to consider the use of such an instrument.
The committee examined various relevant previously published guidelines, most of which dealt with the possibility of an influenza pandemic. Members were particularly impressed by a comprehensive 2006 report from Ontario, Canada, describing relevant principles underlying triage for a possible flu pandemic, presciently including possible solutions applicable to the COVID‐19 pandemic.6
As Israel's population is almost 80% Jewish, one must keep in mind the effect that the norms of this religion can have on decision making—both of health and political authorities as well as front‐line health personnel and their patients. For its part, Islam, the religion of the remaining 20% of Israel's population, takes a similar approach to end‐of‐life care so that from the point of view of religion most citizens, whether Jewish or Muslim, have a similar world view of the sanctity of life.7
In an analysis of the formal Jewish legal approach (Halacha) to issues of rationing during an influenza epidemic, Dienstag8 notes, “Triage is necessary in all cases where there are not enough resources to benefit those that need them. However, with a written protocol a clear‐headed approach to the triage could be formulated. Furthermore, a protocol would prevent doctors from falling down a slippery slope and committing acts which society has deemed unethical and possibly even criminal.”
The current coronavirus crisis has shown what can happen when health services are overwhelmed, such as is the case in Italy, Spain, and, more recently, in New York State. Although requiring confirmation, one report (The Jerusalem Post, March 22, 2020) described that Italian physicians were so overwhelmed by cases requiring ICU admission that they were not offering such treatment to anyone older than 60 years (https://www.jpost.com/International/Israeli-doctor-in-Italy-We-no-longer-help-those-over-60-621856, accessed April 5, 2020). There have also been numerous other articles in the press coming out of Spain and Italy pointing out that this kind of hasty and ill‐founded decision making may be spreading, including the desertion of older persons in long‐term institutions (https://www.nytimes.com/2020/03/25/world/europe/Spain-coronavirus-nursing-homes.html; accessed April 5, 2020). With all of this as background, the committee offers an alternative framework of planning based on triage principles. General triage principles (“soft utilitarianism”) include:
Priority is offered to severely affected patients who likely will die if they do not receive the treatment but who have a good prognosis if they are ventilated.
Next in line would be those for whom the chances of surviving the disease are significant even without treatment but would increase significantly under treatment.
Not offered ICU/ventilation are less affected patients who have a good prognosis even without such treatment.
Also not receiving ventilator/ICU (but receiving good palliative care) are those seriously affected patients who have a poor prognosis even when treated.
SPECIFIC TRIAGE CRITERIA FOR THE COVID‐19 PANDEMIC
Again, the committee reemphasizes that the triage model offered here is only to be considered in the face of a crisis situation where the number of cases presenting to the health system clearly threatens to overwhelm it. In such a dire scenario, it is certainly preferable to utilize an explicit model that has been prepared in advance, and that has undergone widespread consultation rather than allowing the evolution into a chaotic decision‐making process. We offer three criteria: functional ability, comorbidity, and “biological” age.
Functional Ability
The assessment of functional ability is a core component of comprehensive geriatric assessment and is clearly correlated with patient outcomes and the likelihood of recovering from COVID‐19 infection, especially pneumonia. The assessment of functional ability can be performed using various instruments, such as the Functional Independence Measure, which is in widespread use in Israel. In the committee's view, however, in a context of urgent triage, for those in the community, it is preferable to use a much simpler assessment of “basic activities of daily living” (eating, dressing, bathing, transferring, toileting, mobility). Certainly, in this context, most patients admitted to skilled nursing facilities and to wards, for those experiencing dementia, would be considered functionally impaired.
Comorbidity
Data from international ICU experience clearly indicate that the presence of underlying disease has clear ramifications on patient outcomes. At the time of writing, most (but not all) patients dying from the disease around the world experienced significant comorbidity. Although time may not allow the formal use of the usual instruments (e.g., Charlson score), at the least triage teams should take into consideration that those with greater comorbidity will not do as well as those with fewer medical conditions.
Age
The committee gave much thought to this possible criterion, and members were especially concerned lest a panicked retreat into ageism occur under a dire scenario. Although chronological age alone should never be the sole criterion, one cannot ignore this measure, which has clear statistical relevance relating to life expectancy at a population level. For instance, although numbers are still limited, a U.K. critical care audit from the Intensive Care National Audit and Research Centre (April 4, 2020) showed poor COVID‐19 pneumonia ICU survival for those older than 70 years of less than a quarter (24.3%) versus more than three quarters survival (75.7%) for those aged 16 to 49 years.9 An even more recent study from northern Italy showed an equally dire prognosis for older men admitted to ICU. 10 In a situation of emergent triage, it is hard to ignore these stark figures.
That being said, there are some older people who may actually receive greater benefit from ICU care than younger patients, depending, of course, on other factors.11 Clearly, chronological age alone is not a good enough prognostic predictor and, insofar as possible, clinicians should try to judge accordingly. Although not an explicit criterion in the following table, the use of “biological” age was still felt to deserve legitimate “advisory” consideration, but only when combined with other factors that would allow for an estimation of “biological age” and the overall chance of recovery. In the spirit of distributive justice, such an age‐related consideration would only enter the equation were there a need to distinguish between two people of equal status regarding function and comorbidity.
Of interest is the fact that the Canadian group alluded to above did use an (unqualified) age of older than 85 years as one of their exclusion criteria for ventilation.6. Another relevant approach takes into account the years of life remaining as a relevant measure. Although older persons will tend to have fewer years to live, there will be younger patients with severe illness who would thus be triaged after some much older, healthy persons.
Clearly, these three criteria (functional level, comorbidity, and biological age) are not completely independent of each other (i.e., an older person will more likely be less functional and experience various comorbidities). On the other hand, functionally impaired younger patients with multiple illnesses would benefit less from an ICU/ventilator resource than an older but more robust individual. Although not a perfect system, using a combination of these two criteria (or in certain cases all three) will, the committee felt, cover many of the relevant axes in making these difficult decisions.
DESIGN OF A HOSPITAL (ER) TRIAGE SYSTEM
Whenever possible, the committee felt that the triage process should be supervised by a trained team that would make decisions at arm's length from the ICU team, whose sole task would be to look after patients triaged to them. Whenever possible, this triage group should include an intensivist, a geriatrician, a palliative care physician, and a senior nurse. For a detailed and clear‐minded approach to this important issue, see the article by Truog et al.12 Some have suggested that these teams would not only decide who is to receive ventilation but even be the body that ultimately determines who is to be discontinued from such treatment in the event that the ICU team feels that the patient is not responding to treatment; this is done to free up this resource for someone higher up the triage scale as well as to protect the ICU teams from undue pressure from colleagues and/or family members.
Triage Tool Recommendation
Given all of the above, we offer a simplified tool that would allow the triage team (or in the absence of such a group, senior clinicians from anywhere along the patient stream (home, long‐term institution, ER) to make a reasoned and reasonable decision (Figure 1). This tool is based on expert opinion, accepted geriatric and palliative medical approaches, and gerontology concepts, as well as the structures, resources, and values of Israeli society and healthcare system. This tool, in a situation in which triage becomes necessary, will facilitate and support a stressed medical system to make every effort to ensure that a careful balance is maintained between societal needs and the rights of the individual patient.
Figure 1.
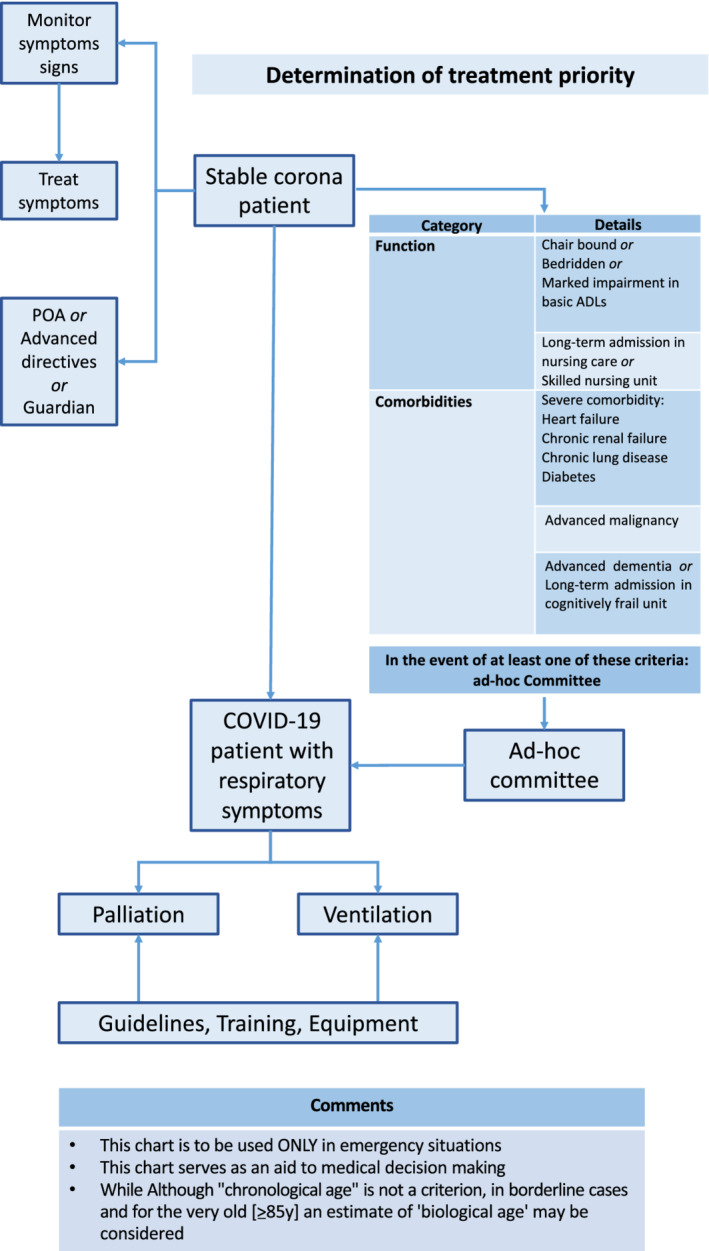
. Triage instrument for patients experiencing coronavirus 2019 (COVID‐19) and requiring intensive care unit/ventilator resource. ADL, activity of daily living.
Patient Preferences and Legal Planning Tools (Advance Directives and Continuing Powers of Attorney)
There will be those, both old and young, who may not wish to receive ICU/ventilator care should they be struck by COVID‐10 pneumonia. These people could be in the community, nursing homes, or even hospital. To respect their autonomy (and only incidentally to help reduce pressure on the hospital/ER/ICU), above all, the committee supported utilizing such an option. Those individuals who clearly express their wish to forgo interventions should formalize their preferences as advance directives and/or continuing powers of attorney, in accordance to Israeli legislation (see above).
POSTTRIAGE (“DOWNSTREAM” CONCERNS)
After triage, patients would be sent to the most appropriate framework given the resources available at that time: to the ICU, a hospital medical ward, palliative care, or home.
Palliative Care
Regarding the principle of beneficence, for those who require respiratory support but for whom ventilation is not assigned or available, for any reason, it is essential to continue personal, humane nursing care utilizing recognized palliative medical techniques to alleviate suffering. Furthermore, the situation of older institutionalized patients being deserted and left to die alone and unattended must be avoided at all costs.
The provision of palliative care is especially critical for older patients in long‐term nursing care and wards for the cognitively impaired. Because many of these patients are functionally and/or cognitively impaired, they are among the most vulnerable older people in society. For these patients, a triage decision limiting ICU/ventilator care where this resource is either not available or judged to be inappropriate should not mean that they are denied a “good death” in the case of severe COVID‐19 infection. With this in mind, it is important to immediately begin to provide palliative care training to nursing home staff, medical and nursing, as well as provide support and assistance to family members and other informal caregivers.
Further guidelines have been provided by the Israel Palliative Medicine Association (appended to the Hebrew language version of these ad hoc committee guidelines). They offer guidance on the symptomatic treatment of dyspnea, the use of hypodermoclysis, and the use of terminal sedation for dying patients.
Primum Non Nocere
For those older patients with severe co‐morbidity and or end‐stage dementia, the use of mechanical ventilation has been shown to be of little benefit, often futile.13 As well, cognitively impaired people will not be capable of making an informed decision nor will they understand what is desired of them during weaning (in the extremely likely stage that this might happen). Common sense and the ethical principle of nonmaleficence demand that we actually protect such vulnerable older people from dying in this uncomfortable and ignominious way unrelated in any way to the principles of triage.
CONCLUSION
A committee of experts convened to establish guidelines for triage of older adults with COVID‐19 infection in Israel. The group made every effort to produce guidelines while keeping the accepted principles of medical ethics in mind. The underlying assumption of the committee was that premorbid function and comorbidity were the main factors to consider. Chronological age alone is not usually a useful consideration when triage is required. That being said, in the fraught situation of deciding between two otherwise similar candidates, “biological age” should be considered.
We have emphasized that the options addressed here are only to be considered in a true emergency situation, at a time when difficult choices need to be made in the face of an overwhelming imbalance between needs and resources; all this in an attempt to take autonomy, beneficence, nonmaleficence, and distributive justice into account and to reach a sometimes difficult balance among them (Table 1). Such an ethically conflicted situation is now playing out in northern Italy and Spain and even in many states in the United States. The committee was concerned lest this dire scenario might play out in Israel too. As such, although mortality rates in Israel are now falling and the system seems to be holding up, at least for now, it is still essential to be prepared with a realistic plan should there be worsening of the situation (second wave). This proposal takes the special case of Israel's older citizens into account, with the hope that we should be fortunate enough never to have to implement such a program.
Table 1.
Selection of Issues Addressing Ethical Principles
| Ethical principle | Relevant issues addressed |
|---|---|
| Autonomy | Remind persons of all ages to draw up (or renew) advance directives addressing relevant domains, such as accessing hospital care and ventilator support |
| Beneficence | Ensuring palliative care principles are addressed throughout spectrum of care, but especially for those patients not offered ventilator support posttriage |
| Nonmaleficence | Protecting vulnerable older persons (e.g., frail, significant cognitive decline, multiple severe comorbidities) from being ventilated and subsequently undergoing an undignified death |
| Distributive justice | Designing and managing a triage mechanism via an open and transparent process meant to offer the greatest good to the greatest number (“soft utilitarianism”) |
ACKNOWLEDGMENTS
An earlier draft of these guidelines was published in Hebrew on the website of the Israel Medical Association (section 7, pages 22‐36; https://www.ima.org.il/userfiles/image/hanhayotCoronaUnions2020.pdf).
We thank Dr Antonio Cherubini, Italy; Dr Joaquim Oristrell Salvà, Spain; Dr Charles Sprung, Israel; and Dr Howard Bergman, Canada, for their helpful comments on an earlier draft of this article.
Conflict of Interest
None.
Author Contributions
A.M.C. wrote the first draft, and all coauthors contributed to subsequent versions, including the final article.
Sponsor's Role
None.
REFERENCES
- 1. Clarfield AM, Manor O, Gabi BN, et al. Health and health care in Israel: an introduction. Lancet. 2017;389:2503‐2513. 10.1016/S0140-6736(17)30636-0. [DOI] [PubMed] [Google Scholar]
- 2. Dwolatzky T, Brodsky J, Azaiza F, Litwin H, Jacobs J, Clarfield AM. Health care challenges of an aging population in Israel (part of the Lancet Israel Country Series). Lancet. 2017;389:2542‐2550. [DOI] [PubMed] [Google Scholar]
- 3. Clarfield AM, Paltiel A, Gindin Y, Morganstin B, Dwolatzky T. Country profile: Israel. J Am Geriatr Soc. 2000;48:980‐984. [DOI] [PubMed] [Google Scholar]
- 4. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ouslander J. Coronavirus19 in geriatrics and long‐term care: an update. J Am Geriatr Soc. 2020;68(5). 10.1111/jgs.16464 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 6. Christian MD, Hawlyruck L, Wax RS, et al. Development of a triage protocol or critical care during an influenza pandemic. CMAJ. 2006;175(11):1377‐1381. doi:10.1503/cmaj.060911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clarfield AM, Gordon M, Markwell H, Alibhai S. Ethical issues in end‐of‐life geriatric care: the approach of three monotheistic religions: Judaism, Catholicism and Islam. J Am Geriatr Soc. 2003;51:1149‐1154. [DOI] [PubMed] [Google Scholar]
- 8. Dienstag A. Rationing During a Flu Epidemic. https://www.yu.edu/sites/default/files/legacy//uploadedFiles/Academics/Seminary/RIETS/Programs/Jewish_Medical_Ethics/Verapo_Yerapey/Rationing%20During%20a%20Pandemic%20Flu.pdf. .
- 9. Intensive Care National Audit and Research Centre . ICNRC Report on COVID‐19 in Critical Care, Apr 4, 2020. file:///C:/Users/markclar/Downloads/ICNARC%20COVID-19%20report%202020–04-04.pdf%20(2).pdf. .
- 10. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS‐CoV‐2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574‐1581. 10.1001/jama.2020.5394 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sprung C, Artigas A, Kesecioglu J, et al. The Eldicus prospective, observational study of triage decision making in European intensive care units: part II: intensive care benefit for the elderly. Crit Care Med. 2012;40(1):132‐138. 10.1097/CCM.0b013e318232d6b0. [DOI] [PubMed] [Google Scholar]
- 12. Truog RD, Mitchell C, Daley GQ. The toughest triage — allocating ventilators in a pandemic. N Engl J Med. 2020. 10.1056/NEJMp2005689 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 13. Teno JM, Gozalo P, Mor V. Association of increasing use of mechanical ventilation among nursing home residents with advanced dementia and intensive care beds. JAMA Intern Med. 2016;176(12):1809‐1816. 10.1001/jamainternmed.2016.5964. [DOI] [PMC free article] [PubMed] [Google Scholar]


