Abstract
Objective
To analyze headaches related to COVID‐19 based on personal case experience.
Background
COVID‐19 is an infection caused by the new coronavirus SARS‐CoV‐2. The first reported case happened in Wuhan on December 1, 2019. At present, at least 1.8 million people are infected around the world and almost 110,000 people have died. Many studies have analyzed the clinical picture of COVID‐19, but they are focused on respiratory symptoms and headache is generically treated.
Methods
I describe and discuss my headaches during my COVID‐19 and I review the MEDLINE literature about headaches and COVID‐19.
Results
More than 41,000 COVID‐19 patients have been included in clinical studies and headache was present in 8%‐12% of them. However, no headache characterization was made in these studies. As a headache expert and based on my own personal clinical case, headaches related to COVID‐19 can be classified in the 2 phases of the disease. Acute headache attributed to systemic viral infection, primary cough headache, tension‐type headache and headache attributed to heterophoria can appear in the first phase (the influenza‐like phase); and headache attributed to hypoxia and a new headache, difficult to fit into the ICHD3, can appear if the second phase (the cytokine storm phase) occurs.
Conclusions
Several headaches can appear during COVID‐19 infection. All of them are headaches specified in the ICHD3, except 1 that occurs from the 7th day after the clinical onset. This headache is probably related to the cytokine storm that some patients suffer and it could be framed under the ICHD3 headache of Headache attributed to other non‐infectious inflammatory intracranial disease. Although the reported prevalence of headaches as a symptom of COVID‐19 infection is low, this experience shows that, very probably, it is underestimated.
Keywords: headache, coronavirus, COVID‐19, SARS‐CoV‐12, cytokine storm
Introduction
COVID‐19 is a coronavirus disease, caused by the coronavirus 2 of the severe acute respiratory syndrome (SARS‐CoV‐2). COVID‐19, it is currently understood, started in Wuhan, central China, on December 1, 2019, and was recognized by the WHO as a global pandemic on March 11, 2020. 1 , 2
SARS‐CoV‐2 is transmitted mainly through Flügge microdroplets, although contact and aerosol are other also possible routes of transmission. After an incubation period of between 2 and 24 days (average of 5 days), a predominantly respiratory clinical picture appears with fever, dry cough, and difficulty breathing. These symptoms are similar to those of influenza. Fatigue, myalgia, headache, nasal congestion, nausea, vomiting, diarrhea, hemoptysis, sore throat, myalgia, arthralgia, anosmia, and ageusia can also appear in a variable combination. Additionally, the initial clinical picture can be complicated by pneumonia, acute respiratory distress syndrome, and sepsis in some patients. 1 , 2
Seven types of coronavirus have been described as causing disease in humans. Four of them (HCoV‐229E, HCoV‐OC43, HCoV‐NL63, and HCoV‐HKU1) cause the common cold, but the other three, SARS‐Cov, MERS‐Cov, and the new SARS‐Cov2, can lead to much more severe respiratory infections in humans. SARS‐Cov caused SARS (Severe Acute Respiratory Syndrome) and MERS‐Cov provoked MERS (Middle East Respiratory Syndrome).
Regarding SARS, from November 2002 to August 2003, 8422 cases have been reported worldwide with a death toll of 916. 3 Headache was presented in 20%‐56% of patients 3 and was the 5th more frequent symptom after fever, non‐productive cough, mialgia, and chills/rigor.
Moreover, MERS affected 1542 worldwide patients from September 2012 with a death toll of 544. 4 Headache affected 11% and was the 6th most frequent symptom after fever, chills/rigors, cough, dry, and hemoptysis. 4 However, no characterization about headaches was performed in SARS and MERS studies.
At present, many clinical studies have been published focused in respiratory and intensive care aspects about COVID‐19. However, headache was only registered as a generic symptom in some of these studies. 5 , 6 , 7 , 8 , 9 , 10 , 11
In this paper, I present my clinical case of COVID‐19, and I detail the headaches I have experienced. In addition, I carry out a review on current data on headache and COVID‐19 infection.
Clinical Case
I am a healthy 51‐year‐old man with no clinical antecedents. I have no personal or family history of migraine. I am a neurologist, specifically a headache expert for 14 years. I work as head of the Headaches and Neuralgias Unit of a Neurology Department of a tertiary and university hospital that is the center of reference of the Health Integral Area Right‐Barcelona (covering a population of 406,000 people).
On March 17, 2020, I felt the first symptom of COVID‐19. It was a non‐productive cough in the form of increasingly frequent and intense paroxysms. About 6 hours later, I presented with a fever of 100.2°F and progressive fatigue.
In the context of that moment of coronavirus infection in Spain (the first case was diagnosed on January 31, 2020, and on March 17 there were already 11,178 patients diagnosed and 491 deaths), I decided to isolate myself from my family in a room in my house to avoid possible risk contact. The real‐time reverse transcriptase‐polymerase chain reaction (RT‐PCR) for SARS‐CoV‐2, of nasal and pharyngeal swab, proved positive the next day.
Anosmia, disgeusia, severe fatigue, and dizziness progressively appeared for the next three days. I did not feel dyspnea nor myalgias. The fever was not intense: 99.5°F‐100.4°F and responded to acetaminophen.
In those three days, I felt various types of headaches. The first one was an episodic headache that met the ICHD3 criteria of Acute headache attributed to systemic viral infection (code 9.2.2.1). 12 It was a diffuse pain, moderate in intensity, which was clearly related to the fever and similar to that of any viriasis such as influenza, with good response to acetaminophen.
Additionally, other headaches appeared in this first phase of the disease. The second headache met the ICHD3 criteria of Primary cough headache (code 9.2.2.1). 12 This headache occurred only in association with coughing. It presented with sudden onset and was brief, lasting less than 2 minutes. It was posterior and bilateral and did not present any associated symptoms.
All the reported headaches easily improved after taking acetaminophen. After the first three days, there was a positive evolution and the headache attributed to systemic viral infection disappeared with the disappearance of the fever. The cough headache remained but trended toward improvement. The rest of the COVID‐19 symptoms also underwent a clear and progressive improvement.
At this point, a 3rd headache progressively appeared. It consisted of a pressing bilateral pain that met the ICHD3 criteria of Tension‐type headache (code 2). 12 The spontaneous pain was mild, but I presented pericranial tenderness to palpation in sternocleidomastoid, splenius, and trapezius muscles. This headache did not present any associated symptoms. Some possible trigger factors can play a role in this tension‐type headache: (1) A cervicogenic factor consisting of myofascial pain due to forced and sustained cervical postures to use mobile phone applications in bed. (2) A stress factor due to the anxiety comported by the possibility of a bad evolution of COVID‐19. (3) Insomnia due to anxiety. Another underlying headache to tension‐type headache could be a possible Headache attributed to heterophoria (code A11.3.5) 12 related to persistent and stressful visual tasks of searching for information about COVID‐19 and communication with family and friends through mobile phone applications. This tension‐type headache also easily improved after taking acetaminophen.
However, on the 7th day after the first COVID‐19 symptom, the fever reappeared with 100.4°F and a new headache appeared different from the previous ones. It was diffuse, continuous, moderate in intensity, and expansive. It was accompanied by neck stiffness and mild photophobia; and worsened with postural changes of the head and routine physical activity. This headache is difficult to integrate under any ICHD3 headings. Moreover, dyspnoea on great exertions appeared and severe fatigue increased. Paroxysmal cough increased severely, so the cough headache also intensified. Other new symptoms appear as cold extremities, tachycardia, and altered mental status.
The next day I returned to the hospital. I presented the following vital signs: heart rate: 104 beats per minute; blood pressure: 122/81 mmHg; respiratory rate 28 breaths per minute; temperature: 99.3°F. The auscultation showed a bilateral lung crackle pattern. Finally, chest radiography (Fig. 1) showed bilateral infiltrations in the lung parenchyma suggestive of COVID‐19 pneumonia.
Fig. 1.
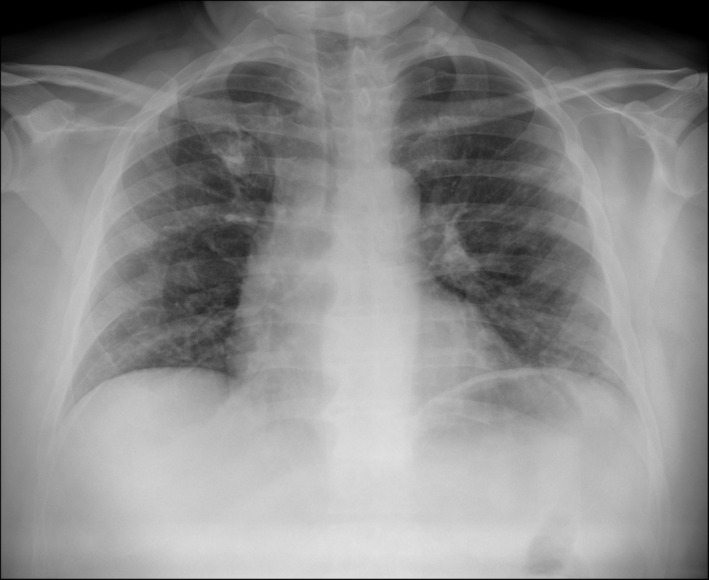
Chest radiography showing bilateral infiltrations in the lung parenchyma suggestive of COVID‐19 pneumonia.
The peripheral capillary oxygen saturation was 93% under ambient. The arterial blood gas analyses obtained by arterial puncture showed a hypoxemia of pO2 68 mmHg [72‐105], pCO2 40.8 mmHg [30‐45], pH 7.47 [7.35‐7.45], bicarbonate 28.8 mmol/L [22‐25], and oxygen saturation 0.94 [0.92‐0.99]. This hypoxemia, induced by the respiratory failure caused by COVID‐19, can also contribute to headache. The ICHD3 establishes the Headache attributed to hypoxia and/or hypercapnia (code 10.1) 12 as no specific headache that evolves parallel to hypoxia.
Laboratory determinations showed hypertransaminasemia with ALT 58 U/L [0‐37 U/L], AST 76 U/L [0‐41 U/L], and GOT 98 U/L [0‐54 U/L]. Muscle parameters were also increased: LDH 287 U/L [125‐243] and CK 208 [0‐174 U/L]. Acute‐phase reactants were disturbed: procalcitonin 0.09 ng/mL [0.00‐0.05 ng/mL], C‐reactive protein 33.8 mg/L [0.0‐5 mg/L], ferritin 1422 μg/L [20‐350 μg/L], and D‐Dimer 633 ng/L [0‐500 ng/L]. The rest of biochemistry parameters was normal.
Regarding hematologic parameters: blood count, hematocrit, haemoglobin, and leukocytes count were normal. However, the leukocyte formula showed a lymphopenia of 0.83 × 10E9/L [1.00‐4.00 × 10E9/L], affecting all the populations (TCD4, TCD8, B, and NK), mainly to TCD8+ with the presence of big and granulate lymphocytes. The platelet count was also low: 121 × 10E9/L [140‐350 × 10E9/L].
Serologies for mycoplasma and cytomegalovirus were negative, and the detection of streptococcus pneumoniae and Legionella pneumophila antigens in urine was also negative.
I was admitted to the hospital and started treatment with hydroxychloroquine and azithromycin plus oxygen therapy by means of a nasal catheter at 3 L/min. Fever, headache, and fatigue immediately disappeared after the second dose of hydroxychloroquine. Lymphopenia also disappeared after 48 hours and the rest of acute‐phase reactants progressively improved. I completed the treatment with hydroxychloroquine 100 mg b.i.d. for 5 days (after a first day load of 200 mg b.i.d.) and azithromycin 500 mg once a day for three days. After 7 days of admission, I was discharged with mild dyspnea at great exertions and a moderate cough. I write this paper after 27 days from the onset of symptoms, fully recovered, although I remain isolated at home.
Discussion
Headache has been associated with COVID‐19 in 6.5%‐53% of patients in recent studies 5 , 6 , 7 , 8 , 9 , 10 that included more than 1200 patients. Only three of these studies 8 , 9 , 10 included more than 100 patients and headache was present in 8% (6.5%‐21%). A meta‐analysis 11 prior to these studies included more than 40,000 patients from 60 studies and estimated a headache presentation average of 12% (4%‐23%). Headache seems to be the 5th most frequent COVID‐19 symptom after fever, cough, myalgia/ fatigue, and dyspnea. 11
However, headache is not the focus of published papers about COVID‐19. At present, the majority of these papers are focused on the respiratory and intensive care aspects of COVID‐19 and they do not characterize headache. They only talk about it in a generic fashion. For these reasons, headaches reported by these studies can be a mixture of tension‐type headache and headaches attributed to systemic viral infection, heterophoria, cough or hypoxia. Moreover, they also do not explain at what point the headache appears: initial phase or after 7‐10 days. Furthermore, it is not specified whether the patients had previous headaches to the COVID‐19. Finally, all the published studies are Chinese and differences are likely across other countries.
Although the majority of SARS‐CoV‐2‐infected people may have no or mild diseases, some people develop respiratory distress and pneumonia. This last clinical picture presents between the 7th and 10th day after symptom onset (average of 8 days), and can require mechanical ventilation and ICU admission. 13 , 14 A secondary hemophagocytic lymphohistiocytosis (sHLH) has been invoked as the cause of the COVID‐19 worsening between the 7th and the 10th day after the symptom onset. sHLH is a hyperinflammatory syndrome characterized by a hypercytokinemia. It presents with unremitting fever, cytopenias, hyperferritinemia, and acute respiratory distress syndrome. An authentic cytokine storm occurs with an increase of interleukin (IL) IL‐2, IL‐6, IL‐7, and IL‐10, TNFα, granulocyte‐colony stimulating factor, interferon‐γ inducible protein 10, monocyte chemoattractant protein 1, and macrophage inflammatory protein 1‐α. 13 , 15
The headache that appears between the 7th and the 10th days can be provoked by this cytokine storm, by the way of an aseptic meningeal reaction, and could be included in the ICHD3 heading Headache attributed to other non‐infectious inflammatory intracranial disease (Code 7.3.3). 12 An alternative heading could be Headache attributed to exposure to other substances (Code 8.1.11), 12 cytokines.
Headache is the more frequent neurologic symptom in COVID‐19. A first report establishes that neurologic manifestations appear in 36% of COVID‐19 patients. 16 Dizziness (16.8%) and headache (13.1%) are the more frequent, followed by peripheral nervous system symptoms (8.9%), impaired consciousness (7.5%), and acute cerebrovascular disease (2.8%). 16 In fact, the first case of meningitis/encephalitis, with detection of SARS‐Cov‐2 RNA in CSF, has been reported. 17 Finally, despite CSF analyses obtained by lumbar puncture not being a part of the usual examination of COVID‐19 patients, a direct CNS role of SARS‐Cov‐2 in COVID‐19 respiratory failure has been invoked as a hypotheses. 18
The prevalence of headaches in COVID‐19 infection seems to be underestimated in terms of variety and clinical description because in the current studies the focus has likely been directed toward severe respiratory patients. The presentation of headache in COVID‐19 patients after the improvement of the “influenza” phase, between the 7th and the 10th day of the clinical onset, can be a predictor marker of the onset of the cytokine storm. An aseptic meningeal inflammation induced by this cytokine storm can be the subjacent substrate of the 7th day headache in COVID‐19 patients. For all these reasons, we need prospective clinical studies specifically analyzing headaches in COVID‐19 patients.
Statement of Authorship
Category 1
(a) Conception and Design
Robert Belvis
(b) Acquisition of Data
Robert Belvis
(c) Analysis and Interpretation of Data
Robert Belvis
Category 2
(a) Drafting the Manuscript
Robert Belvis
(b) Revising It for Intellectual Content
Robert Belvis
Category 3
(a) Final Approval of the Completed Manuscript
Robert Belvis
Conflict of Interest: None
Funding: None
References
- 1. Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID‐19): A clinical update. Front Med. 2020;10. doi: 10.1007/s11684-020-0767-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adhikari SP, Meng S, Wu YJ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID‐19) during the early outbreak period: A scoping review. Infect Dis Poverty. 2020;9:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hui DS, Wong PC, Wang C. SARS: Clinical features and diagnosis. Respirology. 2003;8:S20‐S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shehata MM, Gomaa MR, Ali MA, Kayali G. Middle East respiratory syndrome coronavirus: A comprehensive review. Front Med. 2016;10:120‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS‐Cov‐2) outside of Wuhan, China: Retrospective case series. BMJ. 2020;368:792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liu M, He P, Liu HG, et al. [Clinical characteristics of 30 medical workers infected with new coronavirus pneumonia]. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:209‐214. [DOI] [PubMed] [Google Scholar]
- 9. Tian S, Hu N, Lou J, et al. Characteristics of COVID‐19 infection in Beijing. J Infect. 2020;80:401‐406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jin X, Lian JS, Hu JH, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus‐infected disease 2019 (COVID‐19) with gastrointestinal symptoms. Gut. 2020;320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Borges do Nascimento IJ, Cacic N, Abdulazeem HM, et al. Novel coronavirus infection (COVID‐19) in humans: A scoping review and meta‐analysis. J Clin Med. 2020;9:E941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Headache Classification Committee of the International Headache Society ( IHS ) . The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1‐211. [DOI] [PubMed] [Google Scholar]
- 13. Pedersen SF, Ho YC. SARS‐CoV‐2: A storm is raging. J Clin Invest. 2020;130:2202‐2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chen G, Wu D, Guo W, et al. Clinical and Immunologic features in severe and moderate Coronavirus Disease 2019. J Clin Invest. 2020;137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mehta P, McAuley DF, Brown M, et al. COVID‐19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033‐1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;10. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moriguchi T, Harii N, Goto J, et al. A first case of meningitis/encephalitis associated with SARS‐Coronavirus‐2. Int J Infect Dis. 2020;94:55‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS‐CoV2 may play a role in the respiratory failure of COVID‐19 patients. J Med Virol. 2020;10. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]


