Abstract
There is ongoing debate regarding the role of aerosols in the transmission of SARS-CoV2 in the health care environment. Here, we report a case in which multiple operating room health care providers were exposed to a patient with asymptomatic SARS-CoV2 infection during a prolonged orthopedic surgical intervention and had no evidence of COVID-19 during the 14-day post-exposure period.
Key Words: Health care worker, Personal Protective Equipment, Covid-19, Exposure investigation, Aerosol-generating procedure
Current evidence suggests that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) is mainly transmitted via respiratory droplets produced during prolonged close contact to an infected person as well from contact with contaminated surfaces.1 Since the potential for SARS-CoV2 to remain viable in a closed environment as an aerosol for 3 hours was first reported, there has been ongoing concern about the role of airborne transmission, especially for health care providers (HCPs) involved in aerosol generating procedures (eg, endotracheal intubation, bronchoscopy).2 , 3 Additionally, transmission from asymptomatic and/or presymptomatic individuals has been reported, although the extent in which they play a role in widespread transmission remains uncertain.4 , 5 Here we describe the outcomes of several operating room (OR) HCPs exposed to a patient who was later discovered to have laboratory-confirmed asymptomatic SARS-CoV2 infection.
A 17-year-old man with no medical history was airlifted to the hospital in March 2020 immediately after a car accident in which he was an unrestrained front seat passenger and partially ejected through the windshield. On arrival, his chief complaint was left lower extremity pain. Complete review of systems was otherwise unremarkable. His temperature was 98.2 F (36.8 C) and O2 saturation on room air was 98%. On exam, he had an externally rotated left leg, and plain films revealed comminuted fractures involving the distal femoral shaft and a right bimalleolar ankle fracture. Chest X-ray was normal. He was placed in skeletal traction and later the same day underwent an intramedullary nail treatment of the left femoral fracture and an open reduction-internal fixation of the right ankle fracture.
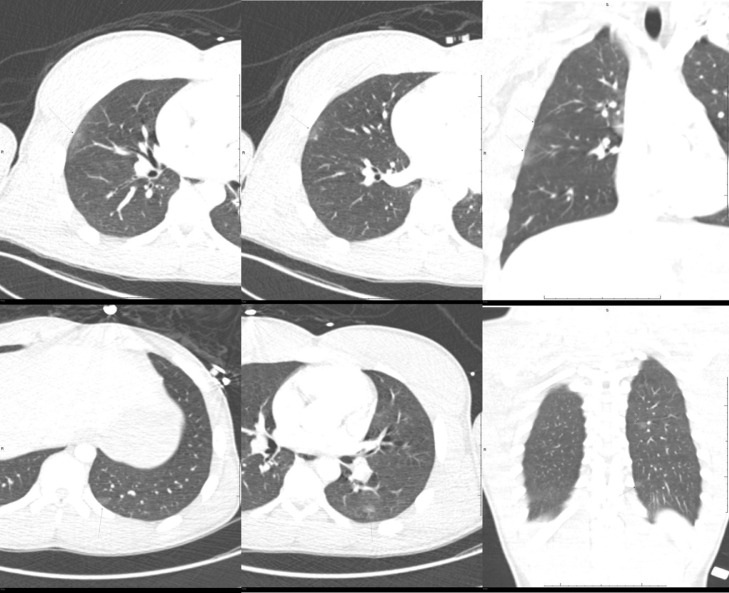
The duration of general anesthesia from start to finish was 6 hours and 5 minutes. Near the completion of the procedure, the lead surgeon was notified that the computed tomography of the chest performed as a part of a total body trauma scan had shown subtle peripheral, subpleural ground glass opacities, most prominent in the right upper and left lower lobe (Fig 1 ). These findings were felt to be due to pulmonary contusions; however, other etiologies could not be excluded given lack of other signs of thoracic traumatic injury. The case was discussed with our institution's Infection Prevention (IP) Coronavirus disease 2019 (COVID-19) response team. SARS-CoV2 testing was not recommended at that time, as the patient was asymptomatic. Nevertheless, OR staff changed their surgical attire to COVID-19 personal protective equipment (PPE) consisting of N95 mask, face shield, gowns, and gloves. On hospital day #2, the patient had a brief postoperative cough (which resolved less than 24 hours later) and, after further discussion, he was placed on contact and droplet isolation precautions and underwent SARS-CoV2 testing on via real-time polymerase chain reaction from a nasopharyngeal swab. The test returned positive 8 hours later. Other than leg pain, the patient remained without symptoms up to 14 days after the day of the accident.
Fig 1.
Computed tomography of the chest on presentation showing subtle ground glass opacities (indicated by thin arrows).
An exposure investigation was launched due to the occurrence of endotracheal intubation without recommended PPE (Table 1 ). A line list of all HCPs present in the OR was created; eleven HCPs were potentially exposed. Individual telephone interviews were conducted by IP to determine exposure type. This revealed that the patient underwent rapid intubation inside the OR using a GlideScope video laryngoscope(Verathon Medical Inc., Bothell, WA)due to presence of a cervical collar. Only 3 HCPs were involved in intubation. They had worn routine surgical attire (surgical mask, gloves) with one additionally wearing goggles. All 3 were deemed to have had a high-risk exposure and were placed on quarantine at home for 14 days per CDC guidance.6 They were advised to perform twice-daily temperature monitoring and symptom check (cough, shortness of breath, and sore throat). The other 8 HCPs were not deemed to have had a high-risk exposure (they were not present or involved in intubation) and were allowed to continue working with temperature monitoring and symptom check (cough, shortness of breath, and sore throat) for 14 days.
Table 1.
Exposure investigation from laboratory confirmed COVID-19 patient in the OR
| HCP in the OR | Title | Present during AGP | COVID-19 Personal Protective Equipment during AGP (N95 mask, gowns, gloves, face shield) | Symptom development during 14-day incubation period from exposure | SARS-CoV2 test performed | Placed on quarantine at home for 14-days |
|---|---|---|---|---|---|---|
| HCP1 | Anesthesiologist | Yes (intubation) | No | Dry cough (onset few hours post procedure) | Yes, negative | Yes |
| HCP2 | Anesthesiologist | Yes (extubation) | Yes | No | No | No |
| HCP3 | CRNA | Yes (intubation) | No | No | No | Yes |
| HCP4 | CRNA | Yes (extubation) | Yes | No | No | No |
| HCP5 | CRNA | No | No | No | No | No |
| HCP6 | Circulator | Yes (intubation) | No | No | No | Yes |
| HCP7 | Circulator | No | No | No | No | No |
| HCP8 | Orthopedic surgeon | No | No | No | No | No |
| HCP9 | Orthopedic resident | Yes (not involved in intubation, not at head end of the table) | No | No | No | No |
| HCP10 | Scrub technician | No | No | No | No | No |
| HCP11 | Scrub technician | Yes (not involved in intubation, not at head end of the table) | No | No | No | No |
AGP, aerosol-generating procedure; CRNA, certified registered nurse anesthetist; HCP, health care personnel; OR, operating room; .
A single HCP (1/11) who assisted with intubation developed a dry cough a few hours postprocedure; no other symptoms were reported. SARS-CoV2 testing was performed and returned negative. This HCP recovered and returned to work 14 days later without issues. The other 10 of 11 HCPs remained asymptomatic throughout the 14-day monitoring period. Due to testing capacity limitations at the time, those asymptomatic HCPs were not offered SARS-CoV2 testing. Both asymptomatic quarantined HCPs returned to work 14 days later without issues. At the time of submission (32 days after the exposure event), we have not identified any suspected nosocomial transmission of SARS-CoV2 in our institution.
Protecting HCPs must be one of the main priorities for both health care institutions and federal, state, and local public health officials.7 It is known that patients with SARS-CoV2 infection can shed viable virus in their nasopharynx prior to onset of symptoms.8 The exact frequency of asymptomatic SARS-CoV2 infections remains unknown, but has been estimated to be at least 20%.9 In the context of known shortages of PPE, a safe optimization strategy should be implemented so supplies can be extended and available when needed most. A key part of this strategy is to reserve filtering respirators (eg, N95 masks) for aerosol generating procedures, which carry the highest risk of exposure.
Here, we report a significant event in which several HCPs who were not using respirators were exposed to an asymptomatic patient with laboratory-confirmed SARS-CoV2 infection and abnormal chest imaging without developing clinical illness suggestive of SARS-CoV2. The major limitation of our report is that we were not able to test for SARS-CoV2 infection in 10 of 11 HCPs, however, it is reassuring that all remained asymptomatic during the period of observation. It is very unlikely that the cough developed by a single HCP was related to the exposure incident. Given testing limitations at the time, we were unable to test asymptomatic patients for SARS-CoV2 infection prior to surgical interventions, though we are now adopting this practice in our institution. Additional studies are needed to better understand the transmission risks in the perioperative environment during the current pandemic, which will be key not only to ensure the protection of health care personnel, but also to provide evidence for a responsible use of PPE.
Footnotes
Financial support: None reported.
Ethics statement: Informed consent was obtained from the patient included in the study.
Conflicts of interest: All authors report no conflicts of interest relevant to this article.
References
- 1.CDC – National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. Interim infection prevention and control recommendations for patients with suspected or confirmed Coronavirus disease 2019 (COVID-19) inhealthcare settings. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Published: 2020. Accessed April 16, 2020.
- 2.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kohanski MA, Palmer JN, Cohen NA. Aerosol or droplet: critical definitions in the COVID-19 era [Published online ahead of print 2020 Apr 23]. Int Forum Allergy Rhinol. 10.1002/alr.22591. Accessed July 10, 2020. [DOI] [PMC free article] [PubMed]
- 4.Hu Z, Song C, Xu C, et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;63:706–711. doi: 10.1007/s11427-020-1661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC – National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. Interim U.S. guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with Coronavirus Disease 2019 (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Published: 2020. Accessed April 16, 2020.
- 7.The Lancet COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25:2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]