To the Editor:
Quarantining dialysis patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a logistical challenge. Appropriately identifying noninfectiousness in patients is essential to safely lift quarantine measures. Serologic tests are used to establish previous infection with SARS-CoV-2, but the extent to which antibody positivity translates to actual immunity is currently unknown.1 Hemodialysis patients are known to have impaired humoral immune responses to vaccination and infection, and it is uncertain whether hemodialysis patients mount an effective antibody response against SARS-CoV-2.
Of our 282 maintenance hemodialysis patients, 7 developed SARS-CoV-2 infection between March 14 and April 7, 2020. All patients displayed symptoms of coronavirus disease 2019 (COVID-19) and tested positive for SARS-CoV-2 RNA on a nasopharyngeal swab on the day of symptom onset. Three patients died (at days 6, 11, and 36), 1 patient is currently still receiving mechanical ventilation, and 3 patients recovered clinically. Longitudinal serum sampling and nasopharyngeal swab tests were performed in 6 of 7 patients (1 patient died before follow-up samples were obtained).
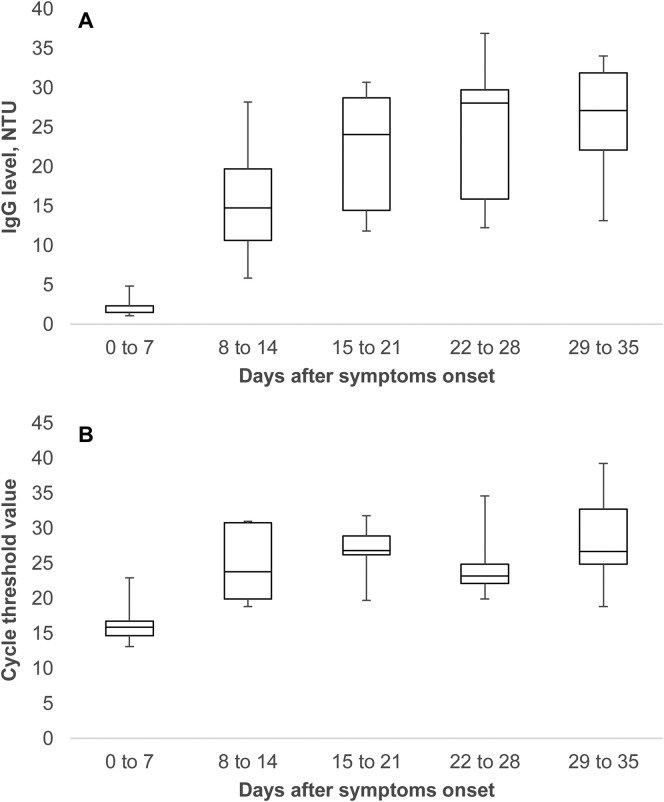
Overall immunoglobulin G (IgG) seroconversion rate was 100% and occurred in the second week after symptom onset. Antibody titer plateaued during the third week (Fig 1 A). Virus persisted in respiratory samples of nonsurvivors until death. In survivors, nucleic acid conversion time, defined as the interval from symptom onset to first negative RT-PCR result, was 34, 37, 37, and 44 days. Cycle threshold values, an inverse measure of nucleic acid concentration, were lowest in the first week of infection and remained relatively stable thereafter (Figure 1B).
Figure 1.
Dynamics of (A) anti–SARS-CoV-2 IgG in serum and (B) SARS-CoV-2 viral load in upper airways. IgG measured by N-protein–based ELISA3 (NovaLisa, NovaTec; validated in-house; approved by the Federal Agency for Drugs and Health Products). A level > 11 NTU (“NovaTec units”) is interpreted as positive, and 9-11 NTU, as borderline. Viral load measured by a laboratory-developed semi-quantitative real-time reverse transcriptase–polymerase chain reaction (RT-PCR) targeting the N (nucleocapsid) and RdRp (RNase-dependent RNA polymerase) genes. A phocine distemper virus was used as a control to test for extraction errors or presence of inhibitors. A cycle threshold value < 40 is interpreted as positive.
In conclusion, maintenance hemodialysis patients are able to mount an antibody response against SARS-CoV-2 that is similar in intensity and timing to that of the nondialysis population. However, anti–SARS-CoV-2 IgG antibodies appeared weeks before the actual clearance of the virus from the upper airways, suggesting that these antibodies are not neutralizing. Viral shedding persisted for more than 5 weeks after symptom onset in survivors. Although viral shedding does not necessarily equal infectiousness,2 awaiting negative RT-PCR testing on at least 2 sequential samples before lifting quarantine in hemodialysis patients is the prudent approach.
Article Information
Financial Disclosure
The authors declare that they have no relevant financial interests.
Acknowledgements
The authors thank Frank De Geeter, Manon Verhulst, and Jessica Van Besien for logistical support.
Peer Review
Received May 19, 2020. Direct editorial input from an Associate Editor and a Deputy Editor. Accepted in revised form May 29, 2020.
References
- 1.Melgaço J.G., Azamor T., Ano Bom A.P.D. Protective immunity after COVID-19 has been questioned: what can we do without SARS-CoV-2-IgG detection? Cell Immunol. 2020;353:104114. doi: 10.1016/j.cellimm.2020.104114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–469. [DOI] [PubMed]
- 3.Okba NMA, Muller MA, Li W, et al. SARS-CoV-2 specific antibody responses in COVID-19 patients [published online ahead of print April 8, 2020]. Emerg Infect Dis. https://doi.org/10.3201/eid2607.200841.