Abstract
Shelter-in-place policies have been considered effective in mitigating the transmission of the virus SARS-CoV-2. To end such policies, routine testing and self-quarantine of those testing positive for active infection have been proposed, yet it remains unclear how often routine testing would need to be performed among workers returning to workplaces, and how effective this strategy would be to meaningfully prevent continued transmission of the virus. We simulated SARS-CoV-2 polymerase chain reaction testing to estimate the frequency of testing needed to avert continued epidemic propagation as shelter-in-place orders are relaxed. We find that testing strategies less frequent than daily (e.g. weekly testing or testing once prior to returning to work) are unlikely to prevent workforce outbreaks without additional interventions. Even given unlimited testing capacity, the impact of frequent testing may not be sufficient to reliably relax shelter-in-place policies without risking continued epidemic propagation, unless other measures are instituted to complement testing and self-isolation.
Keywords: SARS-CoV-2, infection control, epidemiology, pandemic
Background:
Shelter-in-place policies have been considered effective in mitigating the transmission of SARS-CoV-2, the causative virus of COVID-19.1,2 As such policies end, routine testing in high-risk environments (e.g. hospitals, nursing facilities, essential workers) have been proposed to prevent workplace outbreaks. Yet it remains unclear how often routine testing would need to be performed in high-risk workplaces, and how effective such a strategy would be to prevent workplace outbreaks.
Objective:
To estimate the effectiveness of routine testing with SARS-CoV-2 polymerase chain reaction (PCR) to reduce workplace transmission of COVID-19.
Methods and Findings:
We developed a simulation model that included health states of susceptible to infection (non-immune), exposed to SARS-CoV-2, infectious, or recovered (immune). We used the latest available data on the natural history of SARS-CoV-2, including the duration of incubation period, relative infectiousness during pre-symptomatic and early infection stages, and 40% proportion of sub-clinical cases (see Appendix). We modeled an infectious outbreak within a community with a basic reproductive number (R0) of 2.4, corresponding to the number of secondary infections caused by an infected person in an entirely susceptible population.2,3 Workplace transmissions occurred with infectious contacts with the community and within the workforce. We used data on the sensitivity and specificity of PCR testing, as a function of day of infection given known time-varying sensitivity of this test modality.4 We evaluated routine PCR testing of various frequencies, from daily to once monthly testing. We estimated the projected reduction in the number of infectious working days for an infected employee, the primary outcome of this study. We assumed that persons self-isolated upon symptom onset, and persons with PCR-confirmed infection self-isolated one day after detection, while those that were not detected continued to work and potentially infect others. We estimated the effect of testing on the effective reproductive number (Re), while the testing program was in place. Monte Carlo sampling across the uncertainty ranges of each parameter was completed to estimate the range of possible outcomes (see Appendix). The code and data are available online (see Appendix).
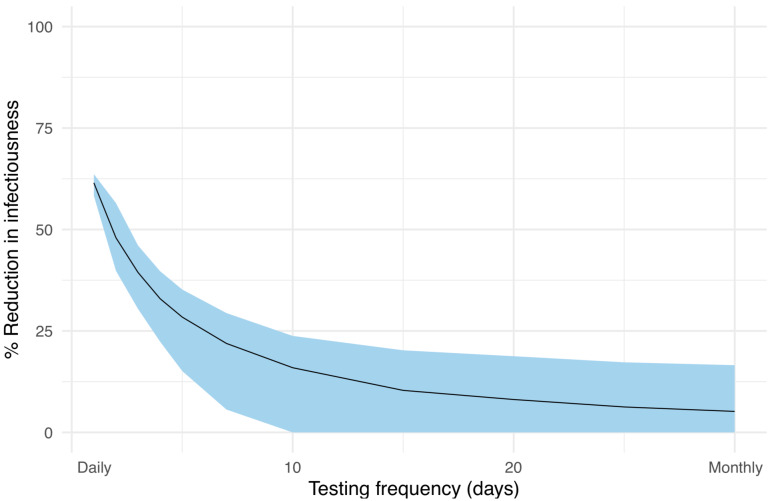
If workers are tested daily by PCR, we estimated a 59.8–64.5% reduction in the number of infectious days worked. By contrast, when testing each worker every three days, we observed a 37.7–41.7% reduction; when testing weekly, we observed a 19.8–23.8% reduction; and when testing monthly, we observed a 2.8–7.4% reduction (Figure 1).
Figure 1: Projected effectiveness of routine PCR testing frequency on reduction on transmission for high risk workers.
The x-axis refers to the frequency of PCR testing simulation from daily (testing frequency of 1 day) to once a month (testing frequency of 30 days). The y-axis represents the reduction in total number of infectious days attributable to each testing strategy. We estimate 40% of cases to be sub-clinical. Error bars represent the interquartile range of projected reduction, varying sensitivity and specificity of the PCR test and assumptions on natural history of transmission.
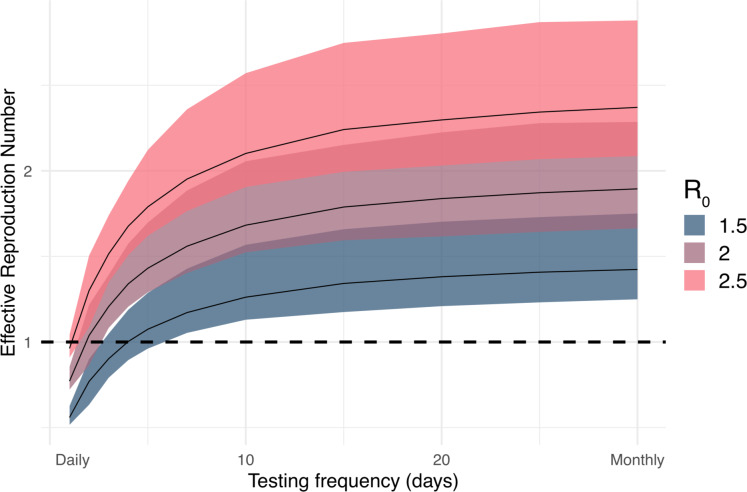
In our simulations, the optimal testing frequency and effective reproduction number (Re) were sensitive to changes in the basic reproduction number (R0, secondary infections caused by an infectious person without any testing or intervention in place), the true value of which remains unclear (Figure 2). If the workplace R0 = 2,2,3 workers would have to be tested at least every two days to prevent an outbreak amongst the workforce (to reach Re < 1), unless other measures were added to testing and self-isolation. If assuming R0 = 2.5,2,3 workers would have to be tested every day. Conversely, if other interventions bring R0 = 1.5, testing every 3–4 days (twice weekly) would suffice (see Appendix).
Figure 2: Projected effective reproduction number in a susceptible workplace under different testing scenarios.
We estimated the effectiveness of increasing frequency of routine PCR testing to reduce the effective reproductive number, under various assumption on the true underlying basic reproductive number. The x-axis refers to the frequency of PCR testing simulation from daily (testing frequency of 1 day) to once a month (testing frequency of 30 days). The y-axis represents the effective reproductive number (Re), which is the average number of people infected by the average person with SARS-CoV-2. The goal is to reduce the effective reproductive number below one to prevent ongoing transmission. Bounds represent the interquartile range.
Discussion:
Our findings imply that in high-risk settings with ongoing community-based transmission, daily PCR testing followed by self-isolation would likely be required to prevent workplace outbreaks if implemented without additional interventions. Due to the imperfect sensitivity of PCR testing, even with frequent testing, a meaningful proportion of infected persons may be missed. We find that strategies with less frequent testing - such as weekly testing or testing once prior to returning to work - would have insufficient reduction in number of infectious days.
The study has limitations in the model assumptions and available data. Transmission of SARS-CoV-2 is documented to have high degree of heterogeneity across settings, whereas we used a transmission rate that considered an average among high-incidence settings such as nursing homes. Our model focuses on outbreaks amongst the workforce in contained high-risk environments, rather than the population at large; it thus assumes workplaces do not provide this level of routine testing to non-workers (e.g. patients, customers). Furthermore, routine PCR testing would require substantial resources, logistical support, and high participation from the population.5
In conclusion, these findings support that routine testing strategies can provide benefit to reduce transmission in high-risk environments with frequent testing but may require complementary strategies to reliably prevent resurgence of case counts to relax shelter-in-place policies. Further evidence should be generated on the use of strategies in combination with testing, including masking, ventilation changes, disinfection, and physical distancing.
Supplementary Material
Acknowledgments
E.T.C acknowledges support by the National Science Foundation Graduate Research Fellowship under Grant No. DGE 1656518. NCL is supported by the University of California, San Francisco. B.Q.H acknowledges support by the National Science Foundation Graduate Research Fellowship under Grant No. DGE 1656518 and the National Library of Medicine under Training Grant T15 LM 007033. Funding sources had no role in the writing of this correspondence or the decision to submit for publication.
Footnotes
Declaration of interests
SB serves on the City of San Francisco’s Department of Public Health street outreach team for homeless adults affected by COVID-19, as a provider at the HealthRight360 Integrated Care Center, and as an employee of Collective Health, all of which provide COVID-19 testing. The views expressed here reflect the opinions of the authors and not necessarily those of affiliated organizations.
References
- 1.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Aff (Millwood). 2020:101377hlthaff202000608. [DOI] [PubMed] [Google Scholar]
- 2.Koo JR, Cook AR, Park M, et al. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26(5):672–675. [DOI] [PubMed] [Google Scholar]
- 4.Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. Variation in False-Negative Rate of Reverse Transcriptase Polymerase Chain Reaction-Based SARS-CoV-2 Tests by Time Since Exposure. Ann Intern Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.