Abstract
The number of CoViD-19 deaths more reliably tracks the progression of the disease across populations than the number of confirmed cases, but substantial age and sex differences in CoViD-19 mortality imply that the number of deaths should be adjusted for the age-and-sex composition of the population as well as its total size. Following well-established practices in demography, this article discusses several measures based on the cumulative number of CoViD-19 deaths and illustrate them with data from 362 national and subnational populations. The first measure is an unstandardized occurrence/exposure rate comparable to the Crude Death Rate. To date, we measured the highest value in New York, exceeding at its peak the state’s most recent annual Crude Death Rate. The second measure is an indirectly standardized rate which we show to perform quite like a directly standardized rate but without requiring a breakdown of CoViD-19 deaths by age and sex. Either way, standardization substantially modifies comparisons across populations: New Jersey has the highest unstandardized rate to date, but four states in Mexico and one in Brazil have higher standardized rates. Finally, extant life tables allow to estimate reductions in 2020 life expectancies, which are projected to exceed two years for New York, New Jersey and Peru, and possibly three years in Ecuador. To put these in perspective, with a 1.1-year projected reduction, the US life expectancy at birth should have in 2020 its largest annual decline since World War II and reach its lowest level since 2006.
Background
As of June 1st, deaths from the novel coronavirus disease 2019 (CoViD-19) had been reported in 186 of the 235 countries and territories of the United Nations system (UN). As with previous viruses whose carriers are mostly asymptomatic,1 the number of deaths due to CoViD-19 provides a lagged but more reliable indicator of its diffusion than the number of confirmed cases. Cumulative CoViD-19 death counts at a given time depend on the determination of the cause of death, delays in reporting deaths to central reporting agencies—different for deaths at home, in hospitals and other institutions—and delays in verification, consolidation and publication at reporting agencies. In the US, for instance, the grim milestone of 100,000 cumulative CoViD-19 deaths was reached at the end of May, when data from the Center for Disease Control and Prevention (CDC) suggested that the number of deaths in the country exceeded expectations based on past trends by close to 130,000.2 While CoViD-19 deaths might not be fully reported, the death undercount is both easier to estimate and an order-of-magnitude smaller than the proportion of unreported cases. CDC data from large-scale seroprevalence surveys suggest than the number of actual cases might be as much as 10 times the number of confirmed cases3—a situation in no way unique to the US.4 CoViD-19 mortality indicators are also more pertinent for assessing public-health measures that were intended less to reduce the eventual number of cases than to “flatten the curve” and eventually limit the number of CoViD-19 deaths by keeping the need for emergency hospitalizations below local hospital capacity.
For comparative purposes, cumulative death counts are affected by several demographic characteristics such as, foremost, population size. The deaths per capita ratio, however, represents the first rather than the only adjustment that can be taken towards more meaningful CoViD-19 mortality comparisons. Following well-established practices in demography,5 this article presents additional indicators that can be derived with additional demographic data. The corresponding measures are discussed using results for the 186 UN countries and territories with at least one death by June 1st. To illustrate issues of scale, the measures are also calculated at the subnational level (e.g., states or provinces) in China, the US, Brazil, Mexico, Italy and Spain—a total of 362 national and subnational populations.
Methods and Data
We first calculate an occurrence/exposure rate, the period Crude CoViD-19 Death Rate (CCDR):
where t1 is an initial time, DC[t1,t] a cumulative CoViD-19 death count between times t1 and t, and N(tm) an estimate of the total population size at time tm between time t1 and time t. The difference between this period rate and the deaths per capita ratio is easy to miss when the death count in the numerator, identical for both, is an annual number of deaths. In that case, the number of person-years in the denominator of the occurrence/exposure rate can indeed be approximated by the population size at some point during the year. However, the two are no longer directly comparable, and the metric of the ratio difficult to interpret, when the death counts correspond to periods of different durations. On the contrary, the CCDR is expressed in deaths per person-year and remains directly comparable to the annual Crude Death Rate (CDR) available for most populations. We first calculate the CCDR for the period starting on the day of the first CoViD-19 death in the population, which was obtained from World Health Organization (WHO) daily situation reports,6 and ending on August 8. The estimated deaths count on that day was obtained from Johns Hopkins University’s Center for Systems Science and Engineering (CSSE)7 and total population size was obtained from the UN.8 Additional sources used for sub-national units are referenced in the Technical Appendix (see online supplementary information). Using projections from the University of Washington’s Institute for Health Metrics and Evaluation (IHME),9 we also calculate a CCDR for the period ending on December 1.
As age and sex variations in CoViD-19 mortality have been clearly established,10 the period rates should be adjusted to take into account differences in age and sex distributions. Direct age-and-sex standardization requires data on CoViD-19 deaths by age and sex, which are unavailable or unreliable for a majority of UN countries and territories and most sub-national populations. An alternative approach, known as indirect standardization, borrows an age-and-sex pattern of mortality from a well-documented population so that only the age-and-sex distribution of the populations of interest are required. Based on this approach, we calculate the Comparative CoViD-19 Mortality Ratio (CCMR):
where USMijC is the CoViD-19 death rate specific to age group i and sex j in the US and Nij(tm) is the size of the age group i for sex j in the population of interest. The reference age-and-sex death rates were obtained from the Centers for Disease Control and Prevention (CDC) weekly-updated distribution of CoViD-19 deaths by age and sex in the US, selected because this is to date the largest number of CoViD-19 deaths distributed by age and sex.11 Unavailable only for the 13 countries/territories whose population size is less than 90,000, population age-and-sex distributions for other countries/territories were taken from the UN data and, for subnational populations, from national statistical office data (see Technical Appendix, online supplementary information).
Multiplying a population’s CCMR by the US CCDR yields an Indirectly age-and-sex Standardized CoViD-19 Death Rate (ISCDR) for that population, with the US age-and-sex population distribution as the standard:
CCMR and ISCDR are again calculated for two periods, both starting with the first CoViD-19 death in the population and ending either on August 8, using CSSE estimates, or on December 1, using IHME projections.
Last, life expectancy at birth provides a summary indicator of mortality in a population in a more intuitive metric (years) than these rates. A standard demographic technique allows to estimate the impact that eliminating a cause of death would have on life expectancy at birth. When a prior period life table (i.e., not factoring CoViD-19 mortality) is available, applying this technique backward allows to translate a cumulative number of CoViD-19-deaths for a given period into a CoViD-19-induced reduction in male and female life expectancies at birth for that period. We used the IHME projections of the cumulative number of CoViD-19 deaths by December 1 as conservative projections of that number for the entire calendar year to derive new male and female 2020 life expectancies at birth in 244 populations with extant life tables (153 countries, plus Italian regions, Spanish autonomous communities and US states). Calculations required a previous projection of the male and female year-2020 life tables in these populations. For countries, these were again derived from UN data, by interpolation between the 2015–20 estimates and 2020–25 projections. For sub-national populations, life tables available from national statistical institutes were extrapolated to 2020. Additional details on their calculation are described in the Technical Appendix (see online supplementary information).
Results
To illustrate the properties of these indicators, we briefly describe results from the August-8 updates of the CCSE, IHME and CDC data. (Full results for that week, ranked on CCMR values, are also provided in the online supplementary information). Across countries (with at least 100,000 inhabitants), Belgium has the highest current-period CCDR value of any country (2.13 deaths per thousand person-years), followed by the United Kingdom, Peru, Sweden, Spain, Chile Italy, Brazil and the US. However, as many as 7 US states and 15 sub-national units in Brazil, Italy, Mexico and Spain have higher current-period CCDR value than Belgium, with the highest CCDR currently in New Jersey (4.44 per thousand).
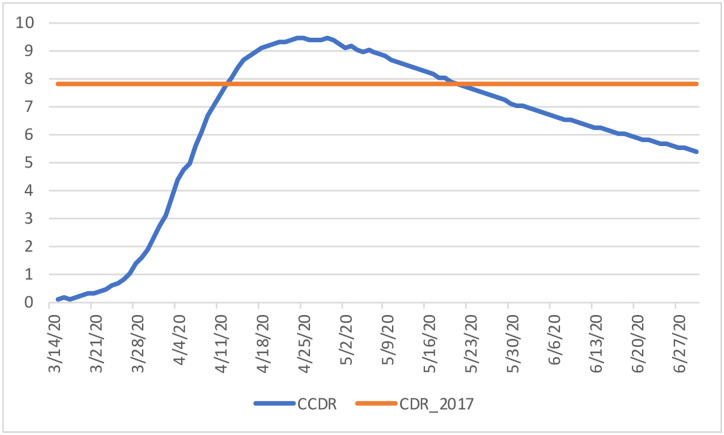
The main motivation for the CCDR is not to compare CoViD-19 mortality across populations, however, but rather to compare CoViD-19 and overall mortality. Of these 362 populations, New York has reached the highest CCDR value to date (9.44 per thousand on 4/25), above the state’s most recent annual CDR (7.83 per thousand in 2017).12 The period CCDR remained above the 2017 CDR until May 20 (Figure 1).
Figure 1:
Estimated value of the period CCDR, New York (in deaths per 1,000 person-years, period starting on March 14 and ending on day shown on the horizontal axis) Sources: CDC (CDR) and authors’ calculations (CCDR, see technical appendix)
Ignoring seasonality and period trends in overall mortality, this indicates roughly equivalent mortality from CoViD-19 and from all other causes combined between March 14 (first CoViD-19 death) and May 20.
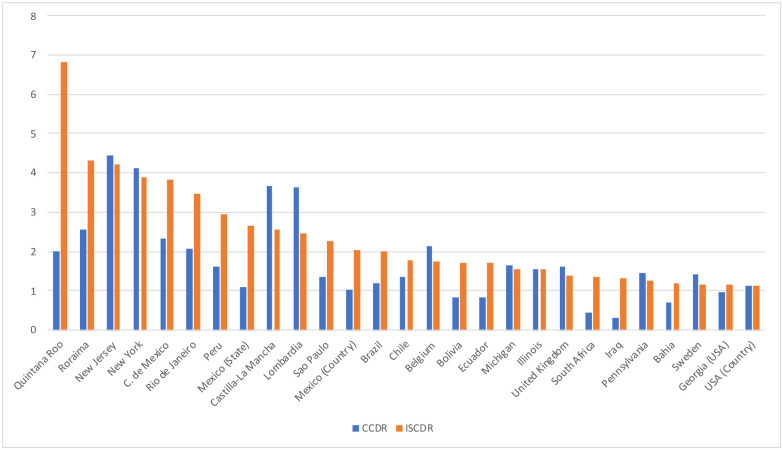
The effects of indirect age-standardization are illustrated in Figure 2, comparing current-period CCDR and ISCDR values for selected national and subnational populations. By construction, the CCMR equals 1 and the CCDR and ISCDR are the same in the US, but the standardized ISCDR is lower than the unstandardized CCDR in Europe, whereas the standardized rate can be two to three times the unstandardized rate in Mexico and South American countries.
Figure 2:
Estimated value of the CCDR and ISCDR (in deaths per 1,000 person-years), by country and subnational unit (countries and subnational units with the largest ISCDR values and a population size over 10 million plus subnational units with the largest ISCDR in their respective countries) Sources: Authors’ calculations (see technical appendix)
Quintana Roo (Mexico) currently has the highest standardized rate. Several other Mexican (Baja California, Tabasco, and Sonora) and one Brazilian States (Roraima) have standardized rates higher than New Jersey (only each country’s highest-rate sub-national populations and those with population of 10 million or more are shown in Figure 2).
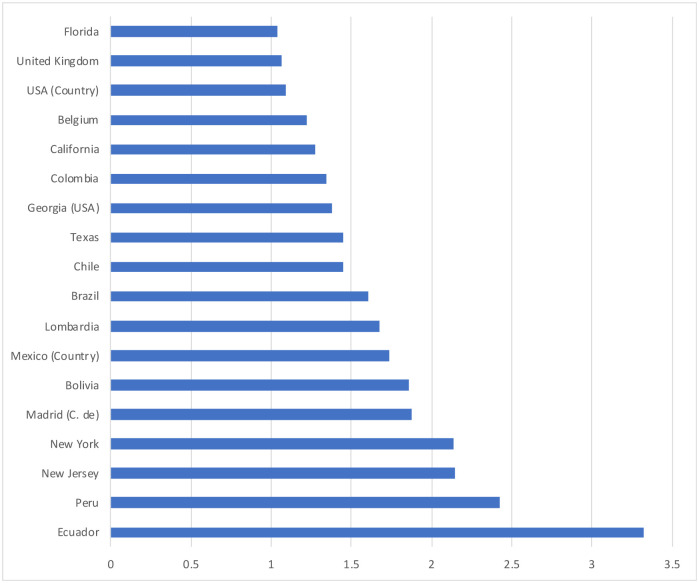
In Europe, reductions in 2020 life expectancies at birth are only projected to exceed one year in two countries, the UK and in Belgium, but larger reductions are projected at the sub-national level in parts of Italy (e.g., Lombardy) and Spain (e.g., Community of Madrid).
Reductions are expected to be over one year in a larger number of countries across the Americas, from 1.1 years in the USA to 2.4 years in Peru and even 3.3 years in Ecuador. Substantial reductions are also projected for a number of US States, up to 2.1 years in New York and New Jersey). Reductions for males only are larger as well (e.g., 3.6 years in Ecuador).
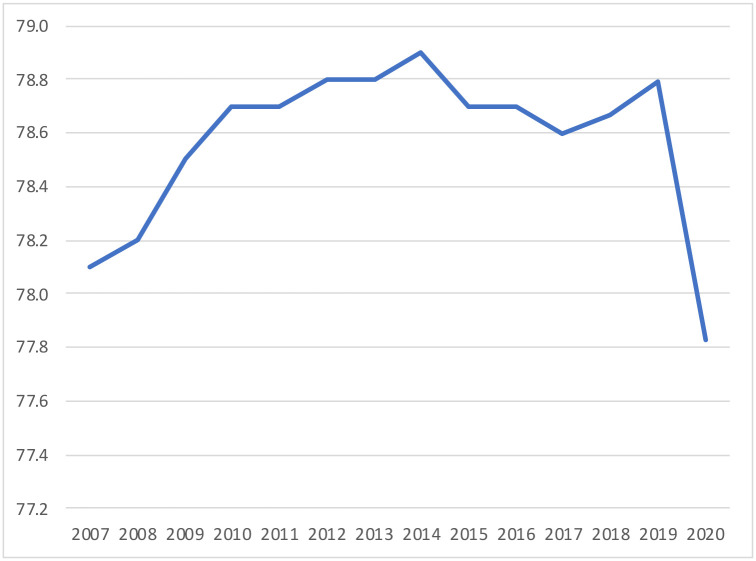
Projecting reductions in 2020 life expectancy at birth allows for comparison between the mortality impact of CoViD-19 and prior public health crises that might have interrupted the secular increase in life expectancies. In the US, for instance, a 1.1-year reduction would be unprecedented since World War II, far exceeding the reversals induced by the HIV epidemic (from 75.8 years in 1992 to 75.5 years in 1993) and the opioid-overdose crisis (from 78.9 years in 2014 to 78.6 years in 2017).13 Based on these projections, US life expectancy at birth would reach in 2020 its lowest level since 2006 (Figure 4).
Figure 4:
Estimated life expectancy at birth, U.S. population, both sexes, by year Sources: CDC (2009–2017), UN and authors’ calculations (2017–2020, see technical appendix)
Discussion
The results above illustrate the properties of different comparative indicators of CoViD-19 mortality. For comparisons across populations, the ISCDR, and CCMR on which it builds, control for three important factors that contribute to the cumulative count of CoViD-19 deaths in a population: the length of the period over which these deaths are cumulated, the size of the population, and its age-and-sex composition.
With respect to the first of these three factors, both the unstandardized and standardized rates are period indicators that increase and decrease as waves of the pandemic develop. Contrary to the death per capita ratio, which can only increase over time, the period rates begin to decline when the daily number of additional deaths drops below its average for the period. This property of the period rates accurately reflects for CoViD-19 mortality a temporal dimension that can often be neglected for overall mortality. This also implies, however, that comparing ISCDR values across populations at too different durations of exposure to CoViD-19 would not be meaningful. As shown in Figure 1, this is more problematic early in the diffusion of the epidemic.
With respect to the second factor, comparing ISCDR values at the national or sub-national levels illustrate that dividing by population size does not completely remove the effects of scale. To illustrate this, we estimated standardized rates at the subnational level in several countries, selected for both their size and within-country differences in CoViD-19 mortality. This showed that if Belgium, with 11.6 million inhabitants, still has the highest period CCDR across countries (besides San Marino), several subnational populations with populations over 10 million have higher CCDR values than Belgium (New York, Lombardy, Mexico City).
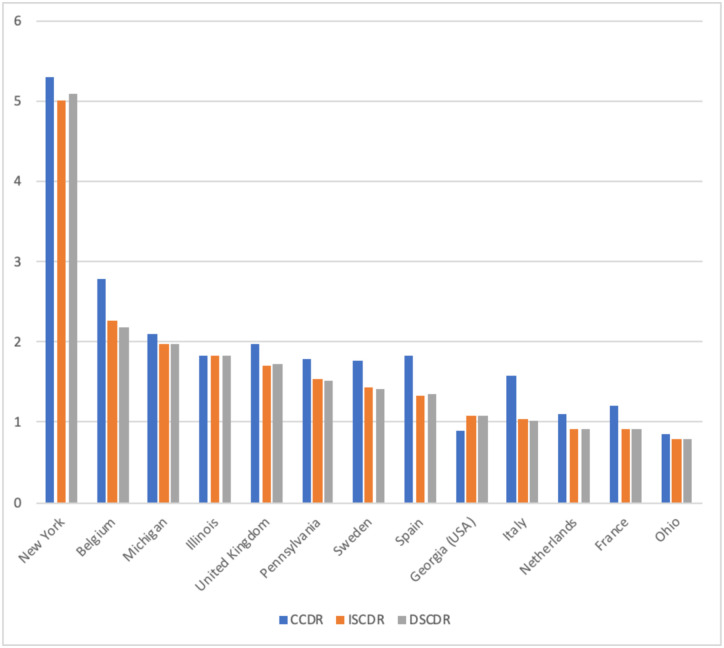
Disaggregation to smaller administrative units may allow for more meaningful comparisons, but might be impeded by data availability. In this respect, indirect standardization has the advantage of not requiring data on CoViD-19 deaths by age and sex that may not be available or reliable for smaller areas. As a breakdown of CoViD-19 deaths is available from a number of European countries14, 15 and US states, the ISCDR can actually be compared to a Directly age-and-sex Standardized CoViD-19 Death Rate (DSCDR) with the US age-and-sex population distribution as the standard. Comparing unstandardized with directly and indirectly standardized rate 7 European countries and 6 states, Figure 5 shows that indirect standardization is a valid alternative to direct standardization.
Figure 5:
Estimated value of the CCDR, ISCDR and DSCDR (in deaths per 1,000 person-years), by country and state (countries and subnational units with a population size over 10 million and the largest ISCDR values) Sources: CDC, Ined and authors’ calculations (see technical appendix)
Substantial uncertainties remain as regards the direct and indirect mortality impact of the pandemic. The direct impact concerns the number of CoViD-19 deaths, for which the main factors of uncertainty are (1) the degree to which CoViD-19 deaths have been properly reported as the cause of death and (2) the future diffusion and fatality rate of the virus. With respect to the latter, the CDC currently tracks no less than 15 forecasting models.16 Our choice of the IHME projections among those to illustrate the properties of the different indicators was not based on a quality assessment, which would be beyond our expertise. The IHME projections have a broader international coverage and longer time horizon that made them more suitable to illustrate the various indicators than other models. Comparisons with other models when populations and horizons overlap do not show the IHME projections as particularly alarmist. Adding that the current projections only run up to December 1st, the cumulative number of CoViD-19 deaths in 2020 appears more likely to be higher than lower than the numbers used here to calculate life expectancy reductions.
The indirect impact refers to the “downstream” effects of the pandemic and mitigating policies on mortality from other causes. Recent CDC data on excess deaths17 continues to suggest that the cumulative number of CoViD-19 deaths does not fully account for the overall increase in mortality, which could be due to under-reporting of CoViD-19 as a cause of death or an increase in other-cause mortality. All else equal, 2020 life-expectancy reductions would be under-estimated, regardless of whether CoViD-19 deaths are under-reported or mortality from other causes increases, because reductions are estimated on the assumption that mortality from other causes remains unchanged. We cannot rule out, however, a decline of mortality from other causes that would have been hidden initially by under-reporting of CoViD-19 deaths. In this case, the indirect impact would partially compensate the direct mortality impact of CoViD-19.18
To be sure, the rapidly evolving data and understanding of CoViD-19 mortality will likely continue to require frequent updates and flexibility. We update the values of the indicators discussed above weekly from updates of the CCSE, IHME and CDC data and shared them on a Github repository.19 These calculations can easily be customized for different periods, different geographical scales, or to accommodate uncertainty across different sources of estimates and forecast.
Supplementary Material
Figure 3:
Estimated reduction in life expectancy at birth for year 2020, both sexes (in years), by country and subnational unit (countries and subnational units with a current CCDR equal or larger than .5 deaths per thousand person-years) Sources: Authors’ calculations (see technical appendix)
Acknowledgment
The authors benefited from facilities and resources provided by the California Center for Population Research at UCLA (CCPR), which receives core support (P2C-HD041022) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). The authors thank Patrick Gerland for clarifications regarding UN demographic data, and Sam Preston, Jason Kerwin and Piedad Urdinola for comments on an earlier draft.
References
- 1.Brookmeyer R & Gail MH. AIDS epidemiology: a quantitative approach. Oxford, England: Oxford University Press, 1994. [Google Scholar]
- 2.Weinberger DW, Chen J, Cohen T et al. 2020. Estimation of Excess Deaths Associated With the COVID-19 Pandemic in the United States, March to May 2020. JAMA Intern Med. Published online July 1, 2020. doi: 10.1001/jamainternmed.2020.3391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Excess deaths associated with COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/commercial-lab-surveys.html. Last used July 2, 2020.
- 4.Modi C, Boehm V, Ferraro S, et al. How deadly is COVID-19? A rigorous analysis of excess mortality and age-dependent fatality rates in Italy. https://www.medrxiv.org/content/10.1101/2020.04.15.20067074v3. May 14, 2020. [Google Scholar]
- 5.Preston SH, Heuveline P & Guillot M. Demography: measuring and modeling population processes. Blackwell: Malden, MA, Oxford, England & Carlton, Australia, 2001. [Google Scholar]
- 6.World Health Organization. Daily situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Last used June 2, 2020.
- 7.Dong E, Du H & Gardne L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Inf Dis (forthcoming). https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30120-1/fulltext. February 19, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019, Online Edition. Rev. https://population.un.org/wpp/Download/Standard/CSV/. Last used June 2, 2020.
- 9.University of Washington, Institute for Health Metrics and Evaluation. COVID-19 projections. https://covid19.healthdata.org/. Last used June 12,2020.
- 10.Dowd JB, Andriano L, Brazel DM, et al. Demographic science aids in understanding the spread and fatality rates of COVID-19. PNAS 2020,117: 9696–8. 10.1073/pnas.2004911117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Provisional COVID-19 death counts by sex, age and state. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku. Last used June 12, 2020. [Google Scholar]
- 12.Kochanek KD., Murphy SL, Xu JQ & Arias E. 2019. Deaths: final data for 2017. NVSR 2019,68(9). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- 13.Arias E, & Xu JQ. United States life tables, 2017. NVSR 2019,68(7). Hyattsville, MD: National Center for Vital Statistics. [Google Scholar]
- 14.National Institute for Demographic Studies (INED). The demographics of COVID-19 deaths. https://dccovid.site.ined.fr/en/. Last used June 9, 2020. [Google Scholar]
- 15.Guilmoto CZZ. 2020. COVID-19 Death Rates by Age and Sex and the Resulting Mortality Vulnerability of Countries and Regions in the World. MedRxiv https://www.medrxiv.org/content/10.1101/2020.05.17.20097410v1 [Google Scholar]
- 16.Centers for Disease Control and Prevention. COVID-19 forecasts: Cumulative deaths. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/forecasting-us.html. Last used June 9, 2020.
- 17.Centers for Disease Control and Prevention. Commercial Laboratory Seroprevalence Survey Data. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Last used June 9, 2020. [Google Scholar]
- 18.Guillot M & Khlat M. 2020. Epidémie de Covid-19: quell impact sur l’espérance de vie en France? https://theconversation.com/epidemie-de-covid-19-quel-impact-sur-lesperance-de-vie-en-france-141484. Last used July 1, 2020.
- 19. https://github.com/statsccpr/ind-cov-mort.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.