Abstract
This cross-sectional study examines prevalence of fit test failure of 2 types of N95 mask (dome-shaped and duckbill) during extended use or reuse among health care workers over 2 days in April 2020 in the UCSF emergency department.
Frontline health care workers are at high risk of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19).1 Personal protective equipment (PPE), including N95 respirators (N95s), is essential for prevention of COVID-19. The Centers for Disease Control and Prevention recommends that health care workers dispose of N95s after a single patient encounter. However, it recommends N95 extended use (wearing the same N95 for multiple patient encounters) and limited reuse (storing an N95 between encounters for use over multiple encounters) during critical PPE shortages.2,3 There are limited data regarding N95 reuse and extended use. Existing studies were conducted in laboratories, not clinical environments.4,5 Inadequate supplies of N95s have forced many emergency departments to implement various N95 reuse and extended use policies but without empirical evidence of their effectiveness. We examined the prevalence of N95 fit test failure while reusing 2 common types of N95 masks.
Methods
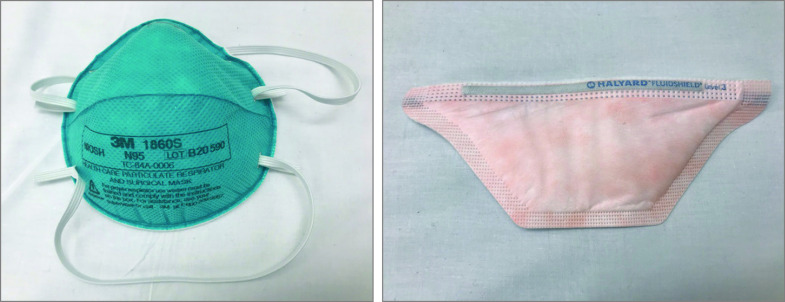
We performed a cross-sectional study of N95 fit at the University of California, San Francisco (UCSF) emergency department from April 4 to April 6, 2020. We enrolled a convenience sample of health care workers (physicians, nurses, nurse practitioners, physician assistants, and patient care technicians) on their clinical shifts when the researchers were present. All had passed a standard Occupational Safety and Health Administration–mandated N95 fit test within the last 1 to 2 years. We performed a qualitative fit test of dome-shaped (3M 1860) and duckbill (Kimberly-Clark 46727 or Halyard 46867) N95s (Figure) during various stages of extended use/reuse using a standardized hood and 3M FT-32 bitter testing solution. If participants could taste the solution, they failed the fit test and were fit with a new N95. We recorded health care worker characteristics, mask type, shifts used, and donnings/doffings. Our primary outcome was N95 fit test failure.
Figure. N95 Mask Types.
Left, dome-shaped. Right, duckbill.
Medians for continuous variables were compared using the Wilcoxon log-rank test. Proportions for categorical variables were compared using the Fisher exact test. For comparisons, a 2-sided α < .05 was considered statistically significant. Given the high failure rate of duckbill masks, we conducted a sensitivity analysis to examine the association between the amount of wear time and fit test failure in only dome-shaped masks. Data were analyzed using Stata version 16 (StataCorp). This study was categorized as exempt by the UCSF institutional review board.
Results
Among 68 participants, 66.2% were women and 48.5% were nurses. Dome-shaped N95s were used by 51 of 68 (75.0%); 17 of 68 (25.0%) used duckbill N95s. Overall, 38.2% of participants failed the fit test; 12 of 17 (70.6%) duckbill masks failed, compared with 14 of 51 (27.5%) dome-shaped masks. Among wearers of dome-shaped masks, fit test failure was associated with increased number of shifts worn (median, 4 shifts [interquartile range {IQR}, 3-5] vs 2 shifts [IQR, 1-3]; P < .001), increased donnings/doffings (median, 15 [IQR, 13-18] vs 8 [IQR, 4-12]; P < .001), and increased hours worn (14 [IQR, 10-30] vs 12 [IQR, 6-16]; P = .048) (Table).
Table. Characteristics of Participants and Prevalence of Fit Failure (Dome-Shaped Masks Only).
| Characteristics | Total (N = 51) | Fit pass (n = 37) | Fit fail (n = 14) | P value |
|---|---|---|---|---|
| Sex, No. (%) | ||||
| Women | 33 (100) | 23 (69.7) | 10 (30.3) | .74a |
| Men | 18 (100) | 14 (77.8) | 4 (22.2) | |
| Health care worker type, No. (%) | ||||
| Nurse | 27 (100) | 20 (74.1) | 7 (25.9) | .77a |
| Physician | 11 (100) | 7 (63.6) | 4 (36.4) | |
| PCT/APP/otherb | 13 (100) | 10 (76.9) | 3 (23.1) | |
| Hours mask worn, median (IQR) | 12 (6-18) | 12 (6-16) | 14 (10-30) | .048c |
| Shifts mask worn, median (IQR) | 3 (2-4) | 2 (1-3) | 4 (3-5) | <.001c |
| Donnings/doffings, median (IQR) | 10 (5.5-15.5) | 8 (4-12) | 15 (13-18) | <.001c |
| Shifts mask worn, No. (%) | ||||
| 1 | 11 (100) | 11 (100) | 0 | <.001a |
| 2 | 12 (100) | 11 (91.7) | 1 (8.3) | |
| 3 | 13 (100) | 10 (76.9) | 3 (23.1) | |
| >3 | 15 (100) | 5 (33.3) | 10 (66.7) |
Abbreviations: APP, advanced practice provider; IQR, interquartile range; PCT, patient care technician.
By Fisher exact test.
Advanced practice provider includes nurse practitioners and physician assistants. Other includes registration clerks and pharmacists.
By 2-sample Wilcoxon rank sum test.
Discussion
This study found duckbill N95s had a high failure rate. Failure of dome-shaped masks was associated with increased use. N95 failure may contribute to SARS-CoV-2 transmission despite PPE use and deserves further study. Based on these preliminary data, health systems should closely evaluate N95 fit during extended use or reuse and limit duckbill mask use if alternatives are available.
Limitations include the study’s cross-sectional design; a cohort study is needed to determine directionality. The duration of wear and number of donnings/doffings were self-reported and may not be precise or accurate estimates. Precise time of failure was not measured. Prior studies have shown an inherent N95 fit failure rate,6 which may have affected outcomes. This observational study was subject to confounding (eg, mask quality, unobserved characteristics of wearer). Shifts worn, hours worn, and donnings/doffings are likely correlated: because of the low number of failures, multivariable adjustment was not performed. This study was designed to detect mask failure based on qualitative fit testing. Failed fit tests may not necessarily result in increased rates of infection.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Occupational Safety and Health Guide to the selection and use of particulate respirators: DHHS (NIOSH) publication 96-101. Centers for Disease Control and Prevention website. Published January 1996. Accessed May 7, 2020. https://www.cdc.gov/niosh/docs/96-101/default.html
- 3.National Institute for Occupational Safety and Health Recommended guidance for extended use and limited reuse of N95 filtering facepiece respirators in healthcare settings. Centers for Disease Control and Prevention website. Published March 2020. Accessed May 7, 2020. https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html#risksextended
- 4.Bergman MS, Viscusi DJ, Zhuang Z, Palmiero AJ, Powell JB, Shaffer RE. Impact of multiple consecutive donnings on filtering facepiece respirator fit. Am J Infect Control. 2012;40(4):375-380. doi: 10.1016/j.ajic.2011.05.003 [DOI] [PubMed] [Google Scholar]
- 5.Vuma CD, Manganyi J, Wilson K, Rees D. The effect on fit of multiple consecutive donning and doffing of N95 filtering facepiece respirators. Ann Work Expo Health. 2019;63(8):930-936. doi: 10.1093/annweh/wxz060 [DOI] [PubMed] [Google Scholar]
- 6.Zhuang Z, Bergman M, Brochu E, et al. Temporal changes in filtering-facepiece respirator fit. J Occup Environ Hyg. 2016;13(4):265-274. doi: 10.1080/15459624.2015.1116692 [DOI] [PMC free article] [PubMed] [Google Scholar]