Abstract
Objective
Measures to decrease hospital length of stay and outpatient visits are crucial during the coronavirus disease 2019 (COVID-19) pandemic. Physician-guided home drain removal presents a potential opportunity for mitigating viral spread and transmission.
Methods
A prospective case series on patients undergoing major head and neck surgery with Jackson-Pratt drain placement was conducted. Patients were shown an infographic detailing drain care and removal at preoperative assessment and prior to discharge. At a 1-week follow-up telemedicine visit, patients were instructed to remove the drain under physician guidance. Patients were assessed 7 days after to determine complication rate and satisfaction.
Results
Twenty-five patients were enrolled with 100% patients undergoing successful drain removal at home with caregiver support. There were no complications reported at the 7-day postdrain removal time point, and overall patient satisfaction was high.
Discussion
Infographics and telemedicine are 2 synergistic strategies to guide safe and effective home drain removal.
Implications for Practice
This study demonstrates how telemedicine and an infographic can be effectively used in physician-guided home drain removal. During a time like the COVID-19 pandemic, innovative measures are necessary to curb transmission and infection rates. We propose a unique and replicable yet safe solution to limit unnecessary exposure and encourage other surgical providers to adopt a similar strategy.
Keywords: COVID-19, telemedicine, infographics, home health, drain removal, PS/QI
The coronavirus disease 2019 (COVID-19) pandemic originating from Wuhan, China, has now spread at an accelerated rate across the world, causing significant financial, social, and medical burdens. Affecting more than 1.3 million people alone in the United States as of May 12, 2020, there is no doubt that the COVID-19 pandemic will have lasting and profound implications on health care.1 In a concerted effort to limit spread of disease, hospitals have been encouraged to implement the unprecedented mandates of cancelling elective surgeries and limiting family member visitation rights. As nonelective cases like cancer operations are still ongoing, novel measures to provide quality and continuous care to such patients are crucial. An ideal protocol must consider limiting unnecessary exposure and infection risk in patients, their caregivers, and providers.
An area for potential technological innovation during the COVID-19 pandemic is surgical drain removal. Active surgical drains such as the Jackson-Pratt system are frequently used after surgery to minimize fluid accumulation in the postoperative period. By attaching a silicone drain to an evacuated bulb with flexible tubing, negative pressure is applied to reduce fluid at surgical sites, thus preventing hematoma and seroma formation.2,3 The drain is then secured to the body using an air knot. Although a drain placement is a minor step during the overall procedure, its importance is not to be underestimated. Drain management has significant implications in surgical wound healing and must be routinely monitored to ensure adequate evacuation of air in the bulb. Drains should also be removed in a timely fashion to prevent risk of wound contamination.4 Patients typically have 2 options regarding drain removal: they must either remain in the hospital for a few days until drain output is deemed acceptable or return for an outpatient visit.
Based on early epidemiologic data, the basic reproductive number (R0) of COVID-19 has been estimated to range from 2 to 3.5, indicating that 2 to 4 persons will be infected from an index patient.5,6 Requiring patients to remain in the hospital or return for an outpatient clinic visit with the sole intention of drain removal is thus associated with a nonnegligible risk in disease spread. Drain removal is a relatively uncomplicated procedure that solely requires cutting the anchoring knot. An intervention to reduce patient contact with health care providers is not only plausible but warranted to limit unnecessary exposure during the pandemic.
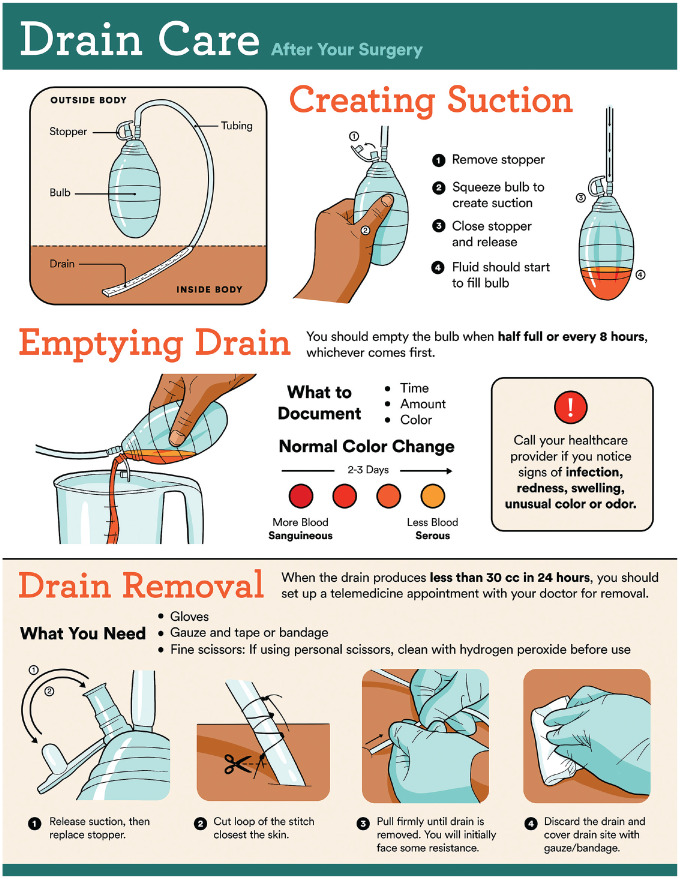
We propose the use of an infographic combined with telemedicine to educate patients on drain care and removal at home. The infographic is a powerful aid to visually represent step-by-step drain care and the removal process and would ideally be introduced in the preoperative surgical planning visit. The drain removal session would then be scheduled to occur under the careful guidance of the attending surgeon or advanced practice provider at the 1-week follow-up telemedicine visit. By repeating multiple iterations in a variety of forms, the hope is that patient comfort and ease with the procedure are increased over the period of multiple weeks. The objective of this study was to determine the utility of using telemedicine and infographics to inform and guide patients on drain removal at home while assessing complication rates.
Materials and Methods
Context
Between April 13, 2020, and May 12, 2020, all patients undergoing nonelective surgery with Jackson-Pratt drain placement were prospectively screened and enrolled in this study. All surgeries were performed by the senior author (K.R.) at the University of Pennsylvania Health System. The study was approved under the Quality Improvement/Quality Assessment exemption by the University of Pennsylvania Institutional Review Board.
Intervention
At the initial preoperative visit, patients were presented with an infographic detailing drain placement, what to expect for drain output, and steps on home drain removal ( Figure 1 ). Patients with caregiver support at home and willing to participate were identified and extensively counseled on the timing and step-by-step process of drain removal. After surgical intervention, drain removal techniques were again reiterated by nurses in the perioperative setting. Upon discharge, patients were provided with a sheet to record drain output as well as time, date, and amount/quality of output.
Figure 1.
Infographic demonstrating active surgical drain care and removal technique.
All patients were scheduled for a 1-week follow-up telemedicine visit for postsurgical assessment and planned drain removal. Prior to the visit, patients were provided with a handout and guidelines for optimization of their telemedicine visit.7 During the visit, the senior author (K.R.) instructed patients on how to remove the drain while using the infographic as a visual aid. With real-time physician guidance and caregiver support, patients were instructed to remove the attached bulb from suction, cut the anchoring air knot, and remove the drain. If the drain produced less than 30 mL over a 24-hour time period prior to their scheduled telemedicine visit, patients were instructed to call the office and move their initial follow-up visit. All patients who requested an earlier follow-up telemedicine visit received one within 24 hours. Patients were called 1 week after drain removal to evaluate whether any complications (ie, hematoma, seroma, bleeding, wound dehiscence, infection) had occurred. Patients were also surveyed at this time to ascertain their experience and satisfaction with using telemedicine and infographics to aid in drain removal.
Inclusion criteria were patients >18 years old presenting with head and neck pathology undergoing major surgical procedure with drain placement. Exclusion criteria were patients who refused to participate or those without adequate caregiver support to assist in drain removal.
Study of Intervention
Data on patient demographics, perioperative details, and postoperative complications were recorded. Patient demographics included age, sex, race, and insurance status. Perioperative details included surgical procedure, quantity of drains, site(s) of placement, and hospital length of stay. Postoperative complications included hematoma or seroma formation, bleeding, wound dehiscence, or infection 7 days after drain removal.
Measures
The primary outcome was success of patient-directed drain removal. Secondary outcomes included complications with and after drain removal.
Analysis
All descriptive statistics were performed using RStudio (RStudio, Inc).
Ethical Considerations
The authors had no potential conflicts of interest. Patients who were uncomfortable with the idea of physician-guided home drain removal received the standard of care. Participation was voluntary, and patients had the right to withdraw from the study at any point and the option to return to the office for drain removal.
Results
Patient Demographics
The study recruited 25 of 35 possible patients undergoing nonelective procedures with Jackson-Pratt drain placement. The average age of patients was 55.6 ± 15.9 years with 60% male and 80% white ( Table 1 ). The most common insurance was private insurance in 16 (64%) patients followed by Medicare in 7 (28%) patients and Medicaid in 2 (8%) patients.
Table 1.
Patient Demographics (N = 25).
| Characteristic | Mean (SD) or No. (%) |
|---|---|
| Age, y | 55.6 ± 15.9 |
| Sex | |
| Female | 10 (40) |
| Male | 15 (60) |
| Race | |
| White | 20 (80) |
| Black | 3 (12) |
| Asian | 2 (8) |
| Insurance status | |
| Private insurance | 16 (64) |
| Medicaid | 2 (8) |
| Medicare | 7 (28) |
Perioperative Details
Most patients underwent oral cavity resection with neck dissection (8 patients, 32%), followed by parotidectomy (5 patients, 20%), cervicofacial advancement after Mohs surgery (3 patients, 12%), and transoral robotic surgery with neck dissection (3 patients, 12%) ( Table 2 ). Four patients (16%) underwent free flap reconstruction. Most patients were able to be discharged the same day as their surgery. The average hospital length of stay was 0.52 ± 0.46 days (range, 0-5 days). All patients received 1 drain, with 18 drains placed in the neck, 5 drains in the extremities, and 2 drains in the chest. All patients who underwent free flap reconstruction surgery had neck drains removed prior to discharge and had a longer average hospital length of stay at 2.5 ± 1.7 days (range, 1-5 days).
Table 2.
Perioperative Drain Details.
| Operation | No. | No. of drains per patient | POD discharge |
|---|---|---|---|
| Parotidectomy ± neck dissection | |||
| Malignancy | 3 | 1 | 0 |
| Benign | 2 | 1 | 0 |
| Oral cavity resection + neck dissection | 8 | 1 | 0 |
| Transoral robotic surgery + neck dissection | 3 | 1 | 1 |
| Excision of neck mass | 2 | 1 | 0 |
| Large cervicofacial advancement after Mohs surgery | 3 | 1 | 0 |
| ALT free flap reconstructiona | 2 | 1 | 2 |
| Fibula free flap reconstructiona | 1 | 1 | 5 |
| Pectoralis major flap reconstructiona | 1 | 1 | 1 |
Abbreviations: ALT, anterolateral thigh; POD, postoperative day.
All patients undergoing reconstruction surgery had neck drains removed prior to discharge.
Complications
No patients reported any complications such as hematomas, seromas, bleeding, wound dehiscence, or infection at the 7-day follow-up. No patients required immediate take back to the operating room or revision surgery.
Discussion
The COVID-19 pandemic represents an unprecedented time in the modern history of health care, motivating hospital systems and health care providers to find innovative ways to continue to provide quality health care to patients. New inventions and creative solutions are being implemented and reported in the literature at an unprecedented speed. We report the novel use of telemedicine and infographics to educate patients on drain care and removal after major head and neck surgery. Twenty-five patients were able to successfully use both strategies simultaneously to self-remove drains with no complications to date. To our knowledge, this is the first study detailing the use of telemedicine and an infographic to improve patient education, thus decreasing hospital length of stay and reducing need for in-person office visits.
Early drain removal has been shown to improve quality of life. Vos et al8 demonstrated that in 99 patients undergoing breast cancer surgery with placement of suction drains, patients who had their drains removed early (flow <30 mL/d) had significantly improved quality of life. No differences were observed in wound healing or the rate of infections, and up to 94% of patients preferred the earlier removal. A similar study in 5581 patients undergoing distal pancreatectomy demonstrated that early removal was associated with better clinical outcomes, such as death, fistula development, delayed gastric emptying, percutaneous drainage, length of stay, and readmission rates.9
It is no surprise that a major factor contributing to increased hospital length of stay and associated costs remains the use of surgical drains in head and neck surgery.10 While the use of neck drains following head and neck surgery is well detailed, timing of drain removal varies among surgeons and institutions. A prospective study was conducted by Harris et al11 in 47 patients who had undergone head and neck surgery to assess safety and cost-effectiveness of removing a neck drain when the amount of drainage was below 50 mL over a 24-hour period. Drain removal was successful in 91% of cases, with only 4 patients developing a seroma after removal. Other studies have demonstrated the efficacy and safety of early drain removal when output was less than 1 to 3 mL.12,13 Despite reported evidence supporting early drain removal, there continues to be considerable heterogeneity among otolaryngologists regarding drain usage, indication for insertion, and decision to remove.14 During an unknown and uncertain time like the COVID-19 pandemic, quality improvement projects to assess the use of surgical drains are crucial to limit unnecessary exposure for patients and health care staff. Although self-removing passive drains have already been successfully used in a unilateral neck dissection patient,15 this study demonstrates how the use of telehealth and infographics may be generalized in the appropriate clinical context.
With the restrictions of the COVID-19 pandemic to minimize infection risk, many hospitals are forbidding family members from visiting patients in the hospital and accompanying loved ones to their preoperative and postoperative visits. Such a mandate, while crucial to curb disease spread, may prevent caregivers from learning and asking questions about surgical drains and removal. As patients must typically remain in the hospital until drain output is deemed low enough by the physician (ie, <30 mL/24-hour period) or return to the outpatient clinic for drain removal, educating patients and caregivers on drain removal at home is an attractive strategy to minimize exposure. Drain removal is a technically simple procedure that does not necessitate increasing length of stay or a return outpatient clinic visit. To the appropriate candidate with proper education and guidance, drain removal can be performed at home with minimal risk.
We therefore propose using telemedicine and infographics as 2 synergistic strategies to improve patient education and minimize exposure risk to COVID-19. Even prior to the advent of the pandemic, telemedicine has provided significant cost savings and maintained high patient satisfaction in the otolaryngology community.16,17 Especially during the pandemic, telemedicine is a useful technique to provide care for patients while mitigating the clinical and financial impact of the pandemic.18,19 Another study completed by the authors assessed satisfaction in 100 patients using a validated telephone survey and found a high level of satisfaction with telehealth clinic visits.20 Infographics are an easy-to-understand, user-friendly method to communicate high-level health information to the layperson. The reporting of information combined with data visualization through charts and diagrams allows the typical reader to better remember and apply the information than reading alone.21 In our series of patients, the concept and process of drain removal was introduced multiple times through the combination of telemedicine and infographics before removal was attempted at home. By repeating several iterations of the same information during a multiweek time period, patients became more familiar and comfortable with the idea of individual drain removal.
Twenty-five patients were prospectively enrolled into this study, and 100% patients reported successful removal of the surgical drain. Ten patients did not have help at home and/or were not comfortable with removing a drain at home and therefore returned for an in-person clinic visit for drain removal. A recent study on 71,440 weighted hospital admissions for head and neck cancer using the 2014 National Inpatient Sample database found that the average hospitalization cost was US$18,371 with an average length of stay of 6.6 days.22 Of those, 5163 patients (36.1%) underwent a major operating procedure with an average admission cost of $18,828 (95% CI, $17,988-$19,668). In addition to the significant costs associated with increased hospital length of stay, patients are at an increased risk for hospital-acquired conditions and nosocomial infections. Especially during the COVID-19 pandemic, limiting exposure risk and infection rates is paramount to reducing patient morbidity and helping curb disease transmission. Allowing patients to remove their drain at home further reduces travel time and expenses and inevitable opportunity costs associated with taking time off.
No complications (ie, seroma, hematoma, bleeding, dehiscence, infection) were observed in our cohort at 7 days after drain removal. Patients subjectively reported increased satisfaction with the entire process, citing “it was surprisingly easier than I thought” and “this is much easier than having to drive into the office.” When asked about the ease and comfort of drain removal, patients reported “the handout helped and knowing you [K.R.] were there watching the whole thing, we felt very comfortable.” Overall, patient satisfaction was high regarding the use of telemedicine and the infographic to guide drain removal.
There are a few limitations to our study. First, selection bias in our cohort may prevent generalizability to the overall patient population. Our study population had family members and/or caregiver support to assist with drain removal at home. Age and other related patient characteristics may have biased the lack of complications and satisfaction with the process. Patients who were uncomfortable were not coerced into participation. The combination of using telemedicine and infographics may prove to be challenging in older patients with less technological experience or caregiver support. Nonetheless, this study demonstrates the successful use of telemedicine and infographics in the appropriate candidate. Second, our patient cohort size was 25 patients, which may be underpowered to assess the true rate of complications after drain removal at home. However, given the urgent call for innovative measures to reduce exposure risk during the COVID-19 pandemic, the strategy of using telemedicine and infographics is timely and relevant.
Implications for Practice
This study demonstrates the effective and safe use of combining telemedicine and an infographic to educate and guide patients on drain removal at home. Decreasing hospital length of stay and number of postoperative outpatient visits is a cost-effective and essential goal during the COVID-19 pandemic to help mitigate unnecessary exposure to patients and providers. This is a sustainable and replicable approach to providing quality and continuous patient care and can be applied to other surgical fields outside of otolaryngology. Further studies assessing the use of both telemedicine and infographics in larger cohorts are necessary to measure complication rates and long-term outcomes. However, given the urgent nature of the COVID-19 pandemic, we encourage other otolaryngologists and surgeons to adopt a similar strategy and to use the infographic, as appropriate, in their own patient population.
Author Contributions
Beatrice C. Go, contributed to the design and acquisition of data for the work, helped draft the manuscript, approved of the final version to be published and agree to be accountable for all aspects of the work; Ryan Brewster, contributed to the design and acquisition of data for the work, helped draft the manuscript, designed the infographic, approved of the final version to be published and agree to be accountable for all aspects of the work; Risha Patel, contributed to the design and acquisition of data for the work, helped draft the manuscript, approved of the final version to be published and agree to be accountable for all aspects of the work; Karthik Rajasekaran, supervised the project, contributed to the conception of the work with critical revisions of the manuscript, approved of the final version to be published and agree to be accountable for all aspects of the work.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: None.
References
- 1. Centers for Disease Control and Prevention. Cases in the U.S. Accessed May 12, 2020 https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- 2. Mamuyac EM, Pappa AK, Thorp BD, et al. How much blood could a JP suck if a JP could suck blood? Laryngoscope. 2019;129(8):1806-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khansa I, Khansa L, Meyerson J, et al. Optimal use of surgical drains: evidence-based strategies. Plast Reconstr Surg. 2018;141(6):1542-1549. [DOI] [PubMed] [Google Scholar]
- 4. Williams J, Toews D, Prince M. Survey of the use of suction drains in head and neck surgery and analysis of their biomechanical properties. J Otolaryngol. 2003;32(1):16-22. [DOI] [PubMed] [Google Scholar]
- 5. Zhao S, Lin Q, Ran J, et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang Y, Wang Y, Chen Y, et al. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92(6):568-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Prasad A, Brewster R, Newman JG, et al. Optimizing your telemedicine visit during the COVID-19 pandemic: practice guidelines for patients with head and neck cancer [published online April 28, 2020]. Head Neck. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vos H, Smeets A, Neven P, et al. Early drain removal improves quality of life and clinical outcomes in patients with breast cancer: results from a randomised controlled trial. Eur J Oncol Nurs. 2018;36:112-118. [DOI] [PubMed] [Google Scholar]
- 9. Seykora TF, Liu JB, Maggino L, et al. Drain management following distal pancreatectomy: characterization of contemporary practice and impact of early removal [published online January 30, 2019]. Ann Surg. [DOI] [PubMed] [Google Scholar]
- 10. Flam JO, Smith R V. What is the optimal time for removing drains in uncomplicated head and neck surgery? Laryngoscope. 2018;128(3):545-546. [DOI] [PubMed] [Google Scholar]
- 11. Harris T, Doolarkhan Z, Fagan JJ. Timing of removal of neck drains following head and neck surgery. Ear Nose Throat J. 2011;90(4):186-189. [DOI] [PubMed] [Google Scholar]
- 12. Kasbekar AV, Davies F, Upile N, et al. The management of vacuum neck drains in head and neck surgery and the comparison of two different practice protocols for drain removal. Ann R Coll Surg Engl. 2016;98(1):53-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Amir I, Morar P, Belloso A. Postoperative drainage in head and neck surgery. Ann R Coll Surg Engl. 2010;92(8):651-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Keane E, Fitzgerald CW, Smyth DA, et al. Drain usage in head and neck surgery: a national survey of thirty-five surgeons across ten units. Ir Med J. 2018;111(10):839. [PubMed] [Google Scholar]
- 15. Qualliotine JR, Orosco RK. Self-removing passive drain to facilitate postoperative care via telehealth during the COVID-19 pandemic. Head Neck. 2020;42(6):1305-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Philips R, Seim N, Matrka L, et al. Cost savings associated with an outpatient otolaryngology telemedicine clinic. Laryngoscope Investig Otolaryngol. 2019;4(2):234-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rimmer RA, Christopher V, Falck A, et al. Telemedicine in otolaryngology outpatient setting—single center head and neck surgery experience. Laryngoscope. 2018;128(9):2072-2075. [DOI] [PubMed] [Google Scholar]
- 18. Pollock K, Setzen M, Svider PF. Embracing telemedicine into your otolaryngology practice amid the COVID-19 crisis: an invited commentary [published online April 15, 2020]. Am J Otolaryngol Head Neck Med Surg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shokri T, Lighthall JG. Telemedicine in the era of the COVID-19 pandemic: implications in facial plastic surgery. Facial Plast Surg Aesthetic Med. 2020;22(3):155-156. [DOI] [PubMed] [Google Scholar]
- 20. Layfield E, Triantafillou V, Prasad A, et al. Telemedicine for head and neck ambulatory visits during COVID-19: evaluating usability and patient satisfaction [published online June 1, 2020]. Head Neck. doi:10.1002/hed.26285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Scott H, Fawkner S, Oliver C, et al. Why healthcare professionals should know a little about infographics. Br J Sports Med. 2016;50(18):1104-1105. [DOI] [PubMed] [Google Scholar]
- 22. Boakye EA, Johnston KJ, Moulin TA, et al. Factors associated with head and neck cancer hospitalization cost and length of stay: a national study. Am J Clin Oncol Cancer Clin Trials. 2019;42(2):172-178. [DOI] [PubMed] [Google Scholar]