Abstract
In the middle of a pandemic, patients with cough and fever are thought to have SARS-CoV-2 (severe acute respiratory syndrome coronavirus-2). It should be remembered that in the desert southwest of the United States, we have an ongoing epidemic of coccidioidomycosis (CM). There are additionally many other respiratory illnesses that could be confused with CoV-2 or overlooked. This is a case report of CoV-2 engrafted on chronic cavitary pulmonary CM. In a time where the coronavirus pandemic is becoming rampant, we demonstrate the case of a coinfection with cavitary pulmonary CM. In this case, the importance of detection of the coronavirus and treatment of the coinfection is explored.
Keywords: pulmonary coccidioidomycosis, cavitary coccidioidomycosis, CoV-2, SARS-Cov-2, corona virus, COVID19, pneumonia
Introduction
CoV-2 (coronavirus-2) is a worldwide pandemic with variable severity. Inevitably, the high frequency of this disease will coexist in individuals with many other disease entities. We recognize that individuals with chronic comorbidities such as chronic obstructive pulmonary disease and heart failure have increased morbidity and mortality from CoV-2 infection. It has been noted that patients with CoV-2 may be coinfected with influenza and other respiratory viruses.1 Bacterial superinfection, apparently less common than in influenza, has also been reported.2,3
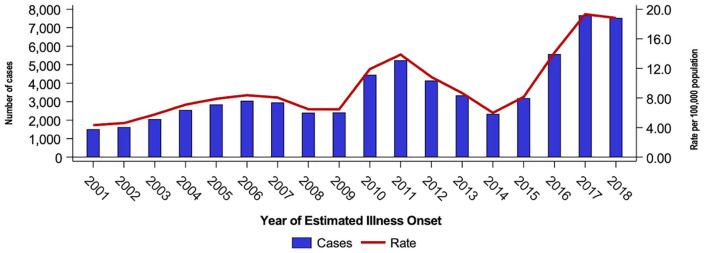
Coccidioidomycosis (CM) is an endemic dimorphic fungus whose frequency in the southwest United States in recent years is epidemic.3 The California Department of Public Health annual report for 2018 demonstrates a significant increase in CM cases since 2015. The reason for this increase remains unclear.4 The case rate as demonstrated in Figure 1 would indicate the CM is epidemic in California. There are similar data for Arizona (see Figure 1).
Figure 1.
Coccidioidomycosis and incidence rates by year of estimated illness onset, California, 2001 to 2018.4
It is inevitable that CoV-2 and CM will be found to coexist in individual patients. A variety of clinical scenarios are possible. Most probable would be a person who contracts pulmonary CM and subsequently develops CoV-2. It is noteworthy that the symptoms of the 2 diseases are extraordinarily similar and include fever, dry cough, dyspnea, myalgia, and headache.3,5,6
Radiographic changes may mimic each other at the margin. Less common will be new CoV-2 infection in individuals with chronic pulmonary CM disease, such as in our case.
CoV-2 may also complicate patients with protracted disseminated disease or primary infection with persistent inflammatory changes (ie, elevated C-reactive protein). Certainly, CoV-2 will occur in CM patients who have largely or entirely resolved their illness.
Methods
Expedited Kern Medical Institutional Review Board approval. Review of the patient’s record.
Case Report
Described is a 48-year-old Hispanic male with chronic cavitary pulmonary CM nonadherent with therapy and visits. He also had uncontrolled diabetes. He presented to his primary care provider after having 6 days of fever, cough, and body aches. The primary care provider diagnosed bronchitis and prescribed azithromycin.
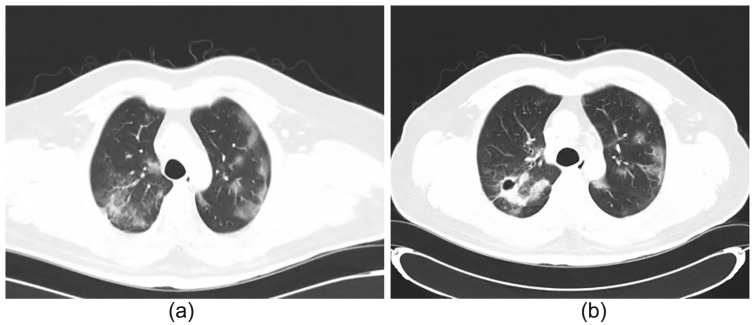
Two days later, the patient went to Kern Medical’s Emergency Department for weakness, progressive cough, fever, and body aches. His vital signs and physical examinations were unremarkable, including an oxygen saturation of 99% on room air. Complete blood count revealed lymphopenia (absolute lymphocyte count of 1000 cells/µL). Inflammatory markers were not obtained. Chemistry demonstrated a glucose of 317 mg/dL, albumin of 2.6 g/dL, and total protein of 8.3 g/dL. Blood cultures were negative. Rapid antigen testing for influenza A and B were negative. Chest X-ray was compared with prior imaging and revealed an increase in size of the cavitary lesion of the right upper lobe (see Figure 2).
Figure 2.
Chest X-ray at presentation demonstrating cavitary lesion of right upper lobe.
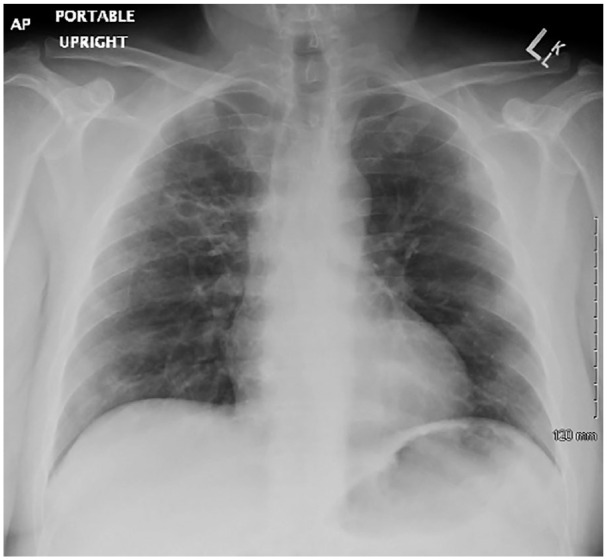
Computed tomography of the chest revealed ground-glass peripheral discreet infiltrates. New ground-glass opacities were distributed peripherally in bilateral lungs7,8 (see Figure 3a and b).
Figure 3.
(a and b) Computed tomography (CT) of the chest showed increased ground-glass opacities in bilateral lobes. These were not seen in previous CT chest.
Coccidioidal serologic tests were positive complement fixing antibodies, 1:32. Nasopharyngeal swab positive for SARS (severe acute respiratory syndrome)-CoV-2. Hospitalization and was not required and he was discharged home. The patient was called by the emergency department physician and informed of the results. This is the first reported case of cavitary pulmonary CM coinfection with CoV-2.
Discussion
The clinical symptoms of pulmonary CM and CoV-2 infection overlap. The majority of CoV-2 is more acute and CM has a more gradual progression of symptoms.5
Distinguishing laboratory features of CM can include an absolute eosinophil count >350 cells/µL.9,10 CoV-2 patients commonly demonstrate lymphopenia, thrombocytopenia, transaminases, and an increased ferritin level is typical.11,12 Both demonstrate elevated inflammatory markers including C-reactive protein and erythrocyte sedimentation rate.10
The radiographic features of the disease are significantly different. The typical radiologic manifestations of primary CM is a parenchymal process.13 The lung consolidation can be localized or multi-segmental. While usually, unilaterally it may be bilateral and extensive. The density can vary from ground glass to dense consolidation. The consolidation can also excavate forming thick- or thin-walled cavities.14
CM may be perihilar with evident lymphadenitis and is commonly basilar. The density can vary from ground glass to consolidation. Cavitation is a complication of primary CM.13,14 In this case, the computed tomography demonstrated a new infectious process superimposed on the chronic right upper lobe cavitary lesion, leading to cavitary expansion. The multiple ground-glass opacities, mostly peripherally located, were completely new developments for this patient.
CoV-2 typically manifests as bilateral peripheral opacification, with or without consolidation, intralobular crazy-paving, reverse halo sign, or other manifestations of organizing pneumonia. These findings are nonspecific and are also shared by other processes such as other viral pneumonias, drug toxicities, and connective tissue diseases.14 The less classic the presentation, the wider the differential of diseases that will manifest in a similar fashion. Differentiation by radiographic pattern alone is not reliable.
Follow-up imaging has not yet been done to radiographically correlate therapeutic response to antifungal treatment. Differences may exist in the therapeutic response of the right upper lobe chronic cavitation as compared with the multiple ground-glass opacities. In CM, clinical resolution of symptoms typically occurs before radiographic resolution with antifungal therapy. Radiographic resolution may take months to years or not at all for coccidioidal cavitary lesions. Coccidioidal ground-glass opacities are usually more acute findings and subsequent resolution is anticipated earlier.
The odds of developing severe respiratory failure in CM are quite low. The risk for ventilatory support is much higher in CoV-2.11
Conclusion
The coincidence of CoV-2 and CM is inevitable. This case has had a salutary outcome thus far. Moreover, it is probable that CoV-2 coinfection on more acute pneumonic cases or those with severe chronic pulmonary CM will have worse morbidity and mortality.1 The same may well hold true for patients with chronic disseminated disease, particularly if they have ongoing inflammation.
The patient with stable resolved pulmonary CM without significant permanent lung injury is not probably at risk for more severe CoV-2 than others of a similar age and comorbidity profile.7 This is also likely true for persons with stable disseminated disease without evident inflammation whether on or off antifungal therapy. The patient described in this report has improved from his CoV-2 infection despite active chronic coccidioidal disease with pulmonary cavitation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Ethical approval to report this case was obtained from the Kern Medical Institutional Review Board (Approval ID: 20020).
Informed Consent: Informed consent for patient information to be published in this article was not obtained because the patient was lost to follow-up.
ORCID iD: Valerie F. Civelli  https://orcid.org/0000-0002-1052-0144
https://orcid.org/0000-0002-1052-0144
References
- 1. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wild D. New guidelines released for managing COVI-19 patients. Published March 26, 2020. Accessed May 14, 2020 https://www.idse.net/Covid-19/Article/03-20/New-Guidelines-Released-for-Managing-COVID-19-Patients/57722
- 3. Freedman M, Jackson BR, McCotter O, Benedict K. Coccidioidomycosis outbreaks, United States and worldwide, 1940-2015. Emerg Infect Dis. 2018;24:417-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Surveillance and Statistics Section, Infectious Diseases Branch Division of Communicable Disease Control, Center for Infectious Diseases, California Department of Public Health. Epidemiologic summary of coccidioidomycosis in California, 2018. Accessed on April 10, 2020 https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/CocciEpiSummary2018.pdf
- 5. Johnson RH, Caldwell JW, Welch G, Einstein HE. The great coccidioidomycosis epidemic: clinical features. In: Einstein HE, Catanzaro A. eds. Coccidioidomycosis: Proceedings of the 5th International Conference on Coccidioidomycosis, Stanford University; August 24-27, 1994: Centennial Conference; Bethesda, MD: National Foundation for Infectious Diseases; 1996:77-87. [Google Scholar]
- 6. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application [published online March 11, 2020]. Ann Intern Med. doi: 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bhatraju P, Ghassemieh BJ, Nichols M, et al. COVID-19 in critically ill patients in the Seattle region—case series [published online March 30, 2020]. N Engl J Med. doi: 10.1056/NEJMoa2004500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American College of Radiology. ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. Published March 11, 2020. Accessed on March 22, 2020 https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection
- 9. Epstein F, Rothenberg M. Eosinophilia. N Engl J Med. 1998;338:1592-1600. [DOI] [PubMed] [Google Scholar]
- 10. Galgiani JN, Ampel NM, Blair JE, et al. Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis. 2016;63:e112-e146. [DOI] [PubMed] [Google Scholar]
- 11. McGonagle D, Sharif K, O’Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev. 2020;19:102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical update [published online April 2, 2020]. Front. Med. doi: 10.1007/s11684-020-0767-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jude CM, Nayak NB, Patel MK, Deshmukh M, Batra P. Pulmonary coccidioidomycosis, pictorial review of chest radiographic and CT findings. Radiographics. 2014;34:912-925. [DOI] [PubMed] [Google Scholar]
- 14. Simpson S, Kay F, Abbara S, et al. Radiographical Society North America Expert Censuses Statement on reporting Chest CT Findings Related to COVID 19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA [published online April 28, 2020]. J Thorac Imaging. doi: 10.1097/RTI.0000000000000524 [DOI] [PMC free article] [PubMed] [Google Scholar]