Abstract
Perirectal abscesses often occur in the dorsal portion of the perirectal tissues. We report a patient who presented with fever, pain on defecation, and dysuria. He was found to have a perirectal abscess in the anterior perineum pressing on the urethra. After emergency surgery to drain the abscess, the symptoms improved.
Keywords: dysuria, magnetic resonance imaging, perirectal abscess
We present a case of perirectal abscess causing dysuria due to pressure on the urethra.

Introduction
Perirectal and perianal abscesses are common anorectal problems. They are twice as common in men as in women, with a mean age of 40 years in both sexes.1, 2 About 90% of idiopathic perianal abscesses arise because of anal cryptoglandular infection.3 An abscess develops when an anal crypt gland becomes obstructed with inspissated debris, permitting bacterial growth and abscess formation. Most abscesses occur posteriorly, as 8–12 anal glands are predominantly situated around the posterior pole of the anal circumference.4, 5 An anorectal abscess should be promptly drained surgically to relieve severe pain and decrease the risk of progression to severe cellulitis or sepsis.4 We present a case of perirectal abscess causing dysuria due to pressure on the urethra.
Case report
A 65‐year‐old man presented with a high fever, incomplete emptying of the bladder, and pain on defecation for 5 days. His temperature was 38.2°C, pulse 90 beats/min, blood pressure 120/70 mmHg, and respiratory rate 14. There was no perianal erythema, but mild redness was seen in the perineum (Fig. 1a,b). Rectal examination caused severe pain.
Figure 1.
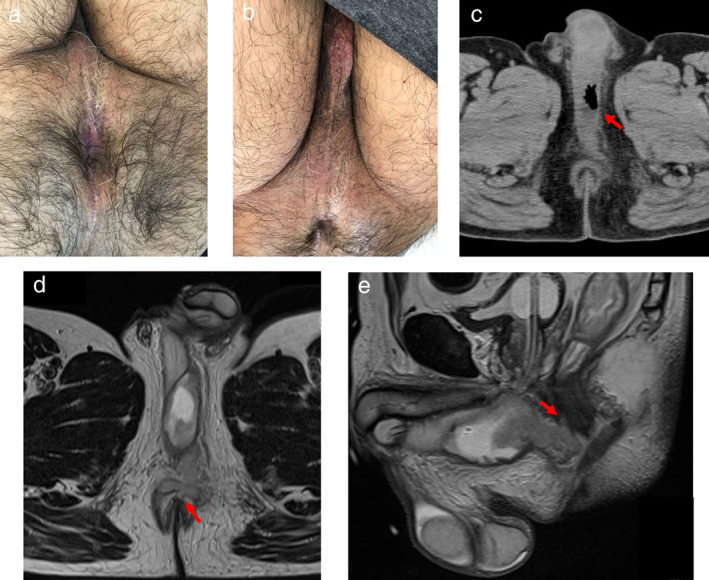
(a) No perianal redness is present, (b) but there is mild erythema of the perineum. (c) Computed tomography demonstrates a low‐density area with air in the perineum (red arrow). (d) Magnetic resonance imaging reveals continuity of the abscess with the anal canal at 12 o' clock (red arrow), (e) which is confirmed on the sagittal view (red arrow).
The white blood cell count was 19.5 × 109/L. The urinalysis was within normal limits. Computed tomography (CT) showed an air‐containing low‐density area in the perineum that was pressing on the urethra (Fig. 1c). On magnetic resonance imaging (MRI), the lesion had a high‐intensity signal on a T2 weighted image and was in continuity with the anal canal at 12 o' clock (Fig. 1d,e).
We diagnosed perirectal abscess and performed emergency surgery to drain it. There was some spontaneous drainage of pus through a crypt orifice located at 12 o' clock, but no superficial fistula was present. We laid open the crypt orifice and inserted a Penrose drain. After the operation, the patient's fever, defecation pain, and dysuria improved.
Discussion
Perianal and perirectal abscesses usually develop in the ischiorectal fossa, the intersphincteric space of the anal canal, or the rectal wall.4 Ischiorectal, intersphincteric, supralevator, and horseshoe abscesses are all classified as perirectal abscesses. These are usually located posteriorly because anal glands are situated near the posterior pole.4, 5 Clinically, an anorectal abscess often presents with severe pain in the anal or rectal area and fever. On physical examination, a patch of erythematous, indurated skin overlying the perianal skin may be noted in patients with a superficial abscess. A deeper abscess is often harder to diagnose and may require imaging to do so.6 Dysuria has not previously been reported as a symptom of perirectal abscess. In this case, upon MRI, the lesion had a high‐intensity signal on a T2 weighted image and was in continuity with the anal canal. In addition, the lesions caused urethral deformation due to extrinsic compression of the urethra. Therefore, we thought that a perirectal abscess compressed the urethra and caused dysuria. Residual urine feeling was ameliorated by draining and reducing the abscess from the crypt orifice. To the best of our knowledge, this the first report of a perirectal abscess involving the anterior perineum and causing dysuria.
Although imaging played a limited role in evaluation of perianal infections in the past, newer imaging techniques, especially MRI, are increasingly recognized as playing a crucial role in the initial evaluation.7 Its sensitivity is 100% and specificity 86% for detecting perianal fistulas.8 It is also extremely helpful for preoperative planning by outlining the extent and secondary ramifications of a fistula tract, as well as detecting anal and cutaneous openings and associated abscesses. T2‐weighted images provide good contrast between the hyperintense fluid in the fistula and the hypointense fibrous wall, allowing anatomic differentiation of the abscess from the internal and external sphincters.9 In this case, CT did not demonstrate continuity with the anal canal, but MRI did.
Early referral to a surgical team to discuss incision and drainage is recommended, as is avoidance of a trial of antibiotics that may delay definitive treatment. Because of the risk of deep infection, sepsis, or necrotizing soft tissue infection, patients who are immunosuppressed, have diabetes, or have evidence of sepsis or cellulitis require urgent drainage on the day of presentation.6 Our case illustrates the fact that a perirectal abscess may extend to the anterior perineum and cause dysuria.
Declaration of conflict of interest: None.
References
- 1. Sainio P. Fistula‐in‐ano in a defined population. Incidence and epidemiological aspects. Ann. Chir. Gynaecol. 1984; 356: 219–24. [PubMed] [Google Scholar]
- 2. Read DR, Abcarian H. A prospective survey of 474 patients with anorectal abscess. Dis. Colon Rectum. 1979; 356: 566–8. [DOI] [PubMed] [Google Scholar]
- 3. Parks AG, Gordon PH, Hardcastle JD. A classification of fistula‐in‐ano. Br. J. Surg. 1976; 356: 1–12. [DOI] [PubMed] [Google Scholar]
- 4. Pigot F. Treatment of anal fistula and abscess. J. Visc. Surg. 2015; 152: S23–9. [DOI] [PubMed] [Google Scholar]
- 5. Whiteford MH. Perianal abscess/fistula disease. Clin. Colon Rectal Surg. 2007; 356: 102–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK. Perianal abscess. BMJ. 2017; 356: j475. [DOI] [PubMed] [Google Scholar]
- 7. De Miguel Criado J, del Salto LG, Rivas PF et al MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics. 2012; 32: 175–94. [DOI] [PubMed] [Google Scholar]
- 8. Beets‐Tan RG, Beets GL, van der Hoop AG et al Preoperative MR imaging of anal fistulas: Does it really help the surgeon? Radiology. 2001; 218: 75–84. [DOI] [PubMed] [Google Scholar]
- 9. Yildirim N, Gokalp G, Ozturk E et al Ideal combination of MRI sequences for perianal fistula classification and the evaluation of additional findings for readers with varying levels of experience. Diagn. Interv. Radiol. 2012; 18: 11–19. [DOI] [PubMed] [Google Scholar]


