Abstract
Here, we report a case of coexistence of a duplicate gallbladder and choledochal cyst, which was overlooked preoperatively and confirmed via intraoperative inspection and pathological examination. We concluded that a high index of suspicion is required to diagnose a double gallbladder, and special attention should be paid to preoperative radiological imaging when treating patients with choledochal cysts because these patients present a higher incidence of biliary anomalies.
Keywords: Duplicate gallbladder, duplication, choledochal cyst, cholangiopancreatography, biliary, cholecystectomy
Introduction
Gallbladder duplication, first reported by Boyden in 1926,1 is an extremely rare congenital biliary anomaly, with an estimated incidence of 1 in 4000 people. The development of radiological techniques, such as endoscopic retrograde cholangiopancreatography (ERCP), contrast-enhanced computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP), has led to increasing case reports of gallbladder duplication. Cela et al. reported a case of double gallbladder associated with a choledochal cyst.2 However, the diagnosis was based only on an imaging study without pathological examination. Here, we report a case of coexistence of a duplicate gallbladder and choledochal cyst, which was overlooked preoperatively and confirmed via intraoperative inspection and pathological examination. Because patients with choledochal cysts have a higher incidence of binary anomalies, a high index of suspicion is required for diagnosing a double gallbladder, and special attention should be paid to preoperative radiological imaging when treating these patients.
Case report
A 61-year-old man was admitted to our hospital for recurrent right epigastric pain and weight loss occurring for 6 months. Ultrasonography and contrast-enhanced abdominal CT showed saccular dilatation of the common bile duct and mild thickening of the gallbladder wall (Figure 1a). MRCP also showed saccular dilatation of the common bile duct, with a maximum diameter of 38 mm. T2-weighted magnetic resonance imaging revealed multiple gallbladder stones (Figure 1b–c).
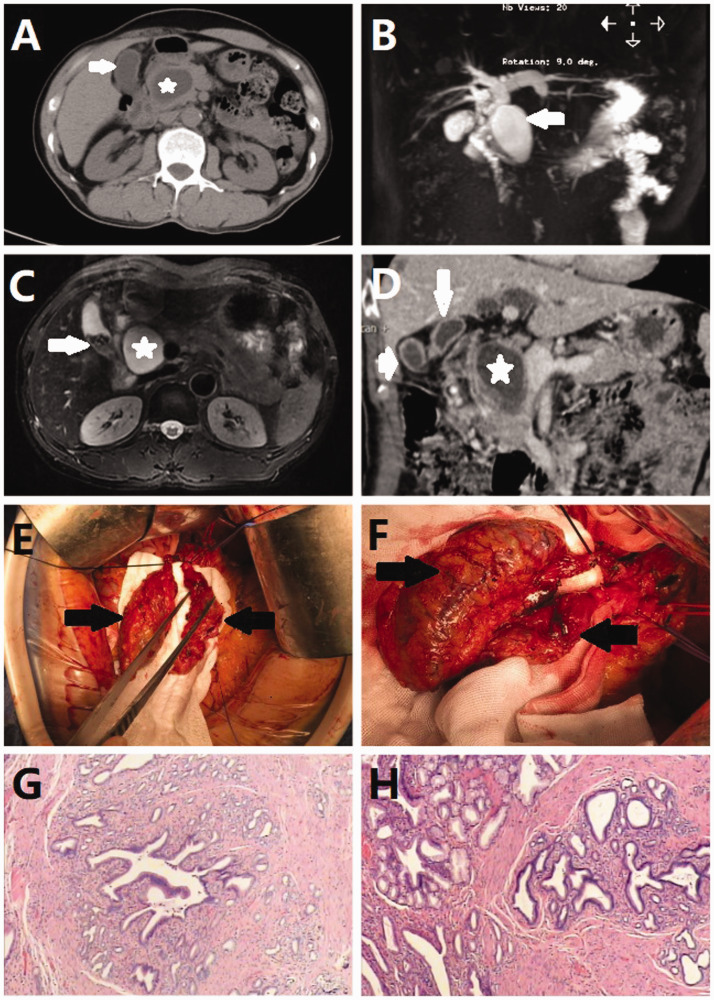
Figure 1.
(a) CT scan revealing mild thickening of the gallbladder wall (arrow) and a choledochal cyst (asterisk). (b) MRCP showing saccular dilatation of the common bile duct (arrow). (c) T2-weighted MR image showing a choledochal cyst (asterisk) and multiple gallstones (arrow). (d) Abdominal CT showing double gallbladders (arrow and arrowhead) and a choledochal cyst (asterisk). (e, f) Double gallbladders observed during the operation. (g, h) Postoperative histopathology showing chronic cholecystitis of the main gallbladder and adenomyomatosis of the accessory gallbladder.
CT: computed tomography; MRCP: magnetic resonance cholangiopancreatography; MR: magnetic resonance.
The patient was diagnosed with a type I choledochal cyst, cholelithiasis and chronic cholecystitis; we planned to perform an open cholecystectomy and choledochal cyst resection with a hepaticojejunostomy. During the procedure, when mobilizing the Calot triangle, we observed an additional ductal structure after identifying the cystic duct and marked this ductal structure, thinking it might be a variant right hepatic duct. We dissected the gallbladder using a retrograde method, and after separating the gallbladder from the liver, a cystic mass remained near the gallbladder fossa, which was connected to the marked ductal structure. We mobilized the cystic mass and found that it was an accessory gallbladder with an independent cystic duct. We removed both gallbladders and successfully performed the choledochal cyst excision with hepaticojejunostomy (Figure 1e–f). Both gallbladders contained multiple gallstones. Postoperative pathological results indicated chronic cholecystitis of the main gallbladder and adenomyomatosis of the accessary gallbladder. The choledochal cyst wall showed fibrotic changes, with small bile duct hyperplasia but no evidence of malignancy (Figure 1g–h).
After the surgery, we reviewed the contrast-enhanced abdominal CT with radiologists and found some clues indicating a duplicate gallbladder, which were unnoticed preoperatively (Figure 1d). The patient recovered well and was discharged 7 days postoperation. The patient’s condition remained good, with no significant findings during the 6-month follow-up. The patient provided written informed consent for publication of this case report and any accompanying images.
Discussion
Both double gallbladder and congenital choledochal cysts are unusual congenital biliary anomalies, with estimated incidences of 1 in 4000 and 1 in 100,000 people, respectively.3 Double gallbladder is thought to develop embryologically from either a single primordium, which divides around the fifth or early sixth weeks of embryonic life, or from two separate primordia.4 Harlaftis’s classification of double gallbladders categorizes anatomical variations based on embryological origin. Type 1 double gallbladders arise from the same primordium but split later in development; therefore, they can be identified by a common cystic duct that drains both gallbladders. Although the septate gallbladder is a single cystic structure separated into two structures by an involuting wall, both gallbladders are joined at the base where they drain into a single cystic duct. With type 2 double gallbladders, a distinct primordium gives rise to the duplicate gallbladder, which has its own second cystic duct. In our case, the double gallbladders had a separate cystic duct draining into the common bile duct; therefore, it was a type 2 double gallbladder.5 In some cases, duplicate gallbladders have been found incidentally during surgery because accessory gallbladders are easily overlooked during the preoperative imaging analysis, as in the present case. Duplicate gallbladders do not need to be removed prophylactically for asymptomatic patients.6 Indications for removing a duplicate gallbladder are the same as those for a single gallbladder: mild-to-moderate acute cholecystitis, gallstones (>2 cm), chronic cholecystitis, common bile duct stones, mild biliary pancreatitis, cholecystic polyps (>1 cm), and porcelain gallbladder.4 When a cholecystectomy is performed, both gallbladders should be removed, even if one appears healthy, to prevent a repeated cholecystectomy.7 In our experience, the following issues should be addressed when treating patients with duplicate gallbladders or unexpected cystic masses of the bile duct during surgery. 1) The accessory gallbladder should be differentiated from other biliary anomalies, especially type II choledochal cysts, during the procedure because different conditions may require different procedures. Intraoperative indocyanine green (ICG) fluorescence cholangiography, a novel and simple navigation tool for delineating the extrahepatic biliary tract, may help if gross inspection is unreliable. Intraoperative cholangiography is recommended during difficult laparoscopic cholecystectomies to reduce the risk of bile duct injury.8 Proper use of intraoperative ICG fluorescence cholangiography may help identify a double gallbladder and help in making decisions during the procedure. 2) If an unexpected ductal structure exists at the Calot triangle during a cholecystectomy, clinicians should consider a possible duplicate gallbladder with independent cystic ducts or a variant right hepatic duct. The unexpected ductal structure should be retained until it can be identified.
In 1977, Todani and colleagues described five categories of congenital choledochal cysts.9 Types I and II are the more common classifications, presenting as saccular dilation and diverticula of the common bile duct, respectively. Less than 1% of patients exhibit both types; this is classified as mixed type I and II. The etiology of congenital choledochal cysts is unclear. Some investigators believe that pancreatic juice reflux into the biliary tree plays an important role in choledochal cyst formation.9 An anomalous pancreaticobiliary ductal union or Oddi dysfunction can cause pancreatic juice regurgitation.9 Because choledochal cysts may be malignant, they should be surgically excised once the diagnosis is confirmed. Only one case of an imaging study showing coexistence of choledochal cysts and a duplicate gallbladder was previously reported, and the patient did not undergo surgical resection.2 In our study, we demonstrated a case of a coexisting duplicate gallbladders and choledochal cyst, which were treated via surgical resection because of a type I choledochal cyst and chronic cholecystitis. Although no standard treatment exists for this unique disease, we recommend resecting the choledochal cyst and duplicate gallbladder with a simultaneous hepaticojejunostomy.
In conclusion, we reported a case of gallbladder duplication in a patient with a choledochal cyst. This case highlights the importance of accurately diagnosing and managing cystic masses of the bile duct. Intraoperative cholangiography performed by experienced surgeons will help treat this unusual condition. Finally, whether an internal relationship exists between gallbladder duplication and choledochal cysts is unclear.
Authors’ contributions
CZ, HZ, ZY, ZM and BH were the clinicians in charge of the cases and determined the medical options in the patient's clinical course. CZ, HZ, ZY and BH performed the surgery. All authors reviewed the data and participated in writing the manuscript. CZ, HZ and ZM were responsible for the concept, critical contribution and revision to this manuscript. All authors read and approved the final manuscript.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This study was supported by the National Natural Science Foundation of China (project nos. 81702783 and 81672475) and the Natural Science Foundation of Guangdong Province (project no. 2017A030310574).
ORCID iD
Baohua Hou https://orcid.org/0000-0002-8517-7600
References
- 1.Miyajima N, Yamakawa T, Varma A, et al. Experience with laparoscopic double gallbladder removal. Surg Endosc 1995; 9: 63–66. [DOI] [PubMed] [Google Scholar]
- 2.Cela D, Hidri B, Aliu D. Duplication of the gallbladder associated with choledocal cyst: a case report. Int J Sci Res 2016; 5: 2097–2099. [Google Scholar]
- 3.Tracy LE, Imagawa DK. Massive congenital choledocal cyst. Liver Int 2014; 34: e161. [DOI] [PubMed] [Google Scholar]
- 4.Smelt JL, Wright H, Sagar J, et al. Laparoscopic removal of a double gallbladder for cholelithiasis: a case report. Ann R Coll Surg Engl 2011; 93: e105–e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harlaftis N, Gray SW, Skandalakis JE. Multiple gallbladders. Surg Gynecol Obstet 1977; 145: 928–934. [PubMed] [Google Scholar]
- 6.Zhou H, Yang Y, Sun AL. [Cholecystopathy in one of the double gallbladders: ultrasonic diagnosis in one case]. Di Yi Jun Yi Da Xue Bao 2004; 24: 1446–1447. [PubMed] [Google Scholar]
- 7.Muralimohan R, Delu A, Beduya D. Right upper quadrant pain: when being in the “fold” means double trouble. Dig Dis Sci 2015; 60: 3230–3233. [DOI] [PubMed] [Google Scholar]
- 8.Flum DR, Dellinger EP, Cheadle A, et al. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA 2003; 289: 1639–1644. [DOI] [PubMed] [Google Scholar]
- 9.Saeed A, Assiri A. Choledochal cyst and biliary stone. J Ayub Med Coll Abbottabad 2018; 30: 127–129. [PubMed] [Google Scholar]