The COVID-19 pandemic is placing an unprecedented strain on health care systems across the world. Hospitals and medical practices have been asked to acclimate to this ever-changing environment by diverting personnel and equipment to help with this crisis.1
Within the outpatient setting the COVID-19 pandemic arouses the particular public health concerns of disease exposure and use of resources. An active clinic environment increases traffic on the hospital campus as well as potential exposure of patients and health care personnel; and it violates contamination strategies such as social distancing. This is especially troubling with the older urological patient population, which is at higher risk for complications from exposure to COVID-19. Furthermore, there are concerns about resource utilization, especially of personal protective equipment, as supply chains fail to meet demands in many health care settings.2
Indeed, every effort should be taken to keep our patients at home, and the rapid expansion of telehealth will allow for many outpatient evaluations to be completed virtually for the foreseeable future.3 While recent guidelines have provided a framework for determining which urology operations should be safely delayed, many questions remain with regard to triaging office-based procedures.4
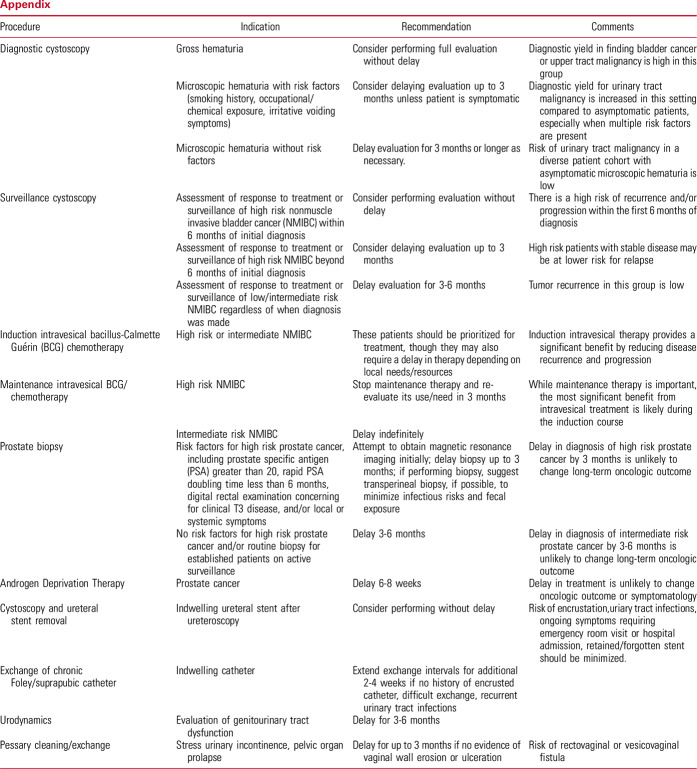
As a representative collection of urologists from several institutions across the U.S, with expertise in different subspecialty fields of urology, we provide a framework to help triage office-based procedures during the COVID-19 pandemic. These recommendations are based on the expert opinion of the authors. They are not intended to be strict guidelines, and are not endorsed by any specific society or panel from the American Urological Association. Furthermore, approaches to all of these urological problems must be tailored to individual settings, personnel and resources; and must always incorporate shared decision making between clinician and patient. The procedures evaluated are summarized in the Appendix.
Based on the best available data, recommendations are made as to which procedural evaluations should continue owing to diagnostic yield and risk of missed/delayed treatment. This is not meant to be a complete and exhaustive list; rather, it encompasses some of the most commonly performed procedures in the outpatient setting.
With regard to procedures targeted at the symptomatology of conditions, such as stress urinary incontinence (urethral bulking), interstitial cystitis (intravesical dimethyl sulfoxide instillation), lower urinary tract symptoms (UroLift®/Rezūm™), overactive bladder (intravesical Botox, percutaneous tibial nerve stimulation, peripheral nerve evaluation for InterStim), we believe these can safely be delayed for at least 3 to 6 months depending on individual settings, availability of resources and shared decision making.
Appendix.
References
- 1.World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. Accessed March 22, 2020. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Interim Guidance for Healthcare Facilities: Preparing for Community Transmission of COVID-19 in the United States. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html. Accessed March 22, 2020. [Google Scholar]
- 3.Hollander JE and Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. https://www.nejm.org/doi/full/10.1056/NEJMp2003539. Accessed March 22, 2020. [DOI] [PubMed]
- 4.Stensland KD, Morgan TM, Moinzadeh A, et al. : Consideration in the triage of urologic surgeries During the COVID-19 pandemic. Eur Urol Epub. https://els-jbs-prod-cdn.jbs.elsevierhealth.com/pb/assets/raw/Health%20Advance/journals/eururo/EURUROL-D-20-00380-1584548684213.pdf. Accessed March 15, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]