Abstract
Objective
We investigated the “BURP” maneuver’s effect on the association between difficult laryngoscopy and difficult intubation, and predictors of a difficult airway.
Methods
Adult patients who underwent general anesthesia and tracheal intubation from September 2016 to May 2018 were included. The “BURP” maneuver was performed when glottic exposure was classified as Cormack–Lehane grade 3 or 4, suggesting difficult laryngoscopy. The thyromental distance, modified Mallampati score, and interincisor distance were assessed before anesthesia.
Results
Among this study’s 2028 patients, the “BURP” maneuver decreased difficult laryngoscopies from 428 (21.1%) to 124 (6.1%) cases and increased the difficult intubation to difficult laryngoscopy ratio from 53/428 (12.4%) to 52/124 (41.9%). For laryngoscopies classified as difficult without the “BURP” maneuver, the area under the curve (AUC) of the thyromental distance, modified Mallampati score, and interincisor distance was 0.60, 0.57, and 0.66, respectively. In difficult laryngoscopies using the “BURP” maneuver, the AUC of the thyromental distance, modified Mallampati score, and interincisor distance was 0.71, 0.67, and 0.76, respectively.
Conclusions
The “BURP” maneuver improves the laryngoscopic view and assists in difficult laryngoscopies. Compared with difficult laryngoscopies without the “BURP” maneuver, those with the “BURP” maneuver are more closely associated with difficult intubations and are more predictable.
Trial registration: www.chictr.org.cn identifier: ChiCTR-ROC- 16009050.
Keywords: “BURP” maneuver, difficult laryngoscopy, difficult tracheal intubation, airway management, intubation, laryngoscopic view
Introduction
Approximately 212.9 million patients worldwide undergo major surgical procedures requiring general anesthesia with invasive airway management (orotracheal or nasotracheal intubation) every year.1 During the presurgical evaluation, some parameters (such as the thyromental distance, modified Mallampati score, and interincisor distance) are assessed to predict difficult airways.2,3 However, difficult airways can occur unexpectedly. As a first step, anesthesiologists can perform simple and sometimes effective maneuvers to manage difficult laryngoscopy.4–6 Applying backward, upward, rightward, and posterior pressure on the larynx (i.e., displacement of the larynx in the backward and upward directions with rightward pressure on the thyroid cartilage) is called the “BURP” maneuver and has been well described by Knill.7 Takahata et al.5 reported that the “BURP” maneuver improved visualization of the larynx more than the “BACK” maneuver. The “BURP” maneuver changes the incidence of difficult laryngoscopy and intubation; however, no study has evaluated the relationship between difficult laryngoscopy and difficult intubation in different situations along with the predictors of a difficult airway, and little is known about whether the “BURP” maneuver can modify the ability of the most common clinical predictors (i.e., the thyromental distance, modified Mallampati score, and interincisor distance) to predict difficult laryngoscopy. Additionally, the following question arises: Should we defy difficult laryngoscopy, as with the “BURP” maneuver? Therefore, we performed this secondary analysis of a prospective observational study to investigate the relationship between difficult laryngoscopy with and without the “BURP” maneuver and difficult tracheal intubation and to possibly redefine difficult laryngoscopy. A secondary goal was to assess the efficiency of the “BURP” maneuver against three airway predictors when used in difficult laryngoscopy conditions.
Materials and methods
This study was designed according to the TRIPOD Checklist. The present study was an investigator-initiated, single-center, prospective observational study conducted from September 2016 to May 2018 at the Yijishan Hospital of Wannan Medical College (People’s Republic of China) and was approved by the Yijishan Hospital’s Institutional Review Board (Chairperson Prof. H. Cao; IRB approval no: (2013)91). Written informed consent was obtained from each participant prior to enrollment. No changes to the methods were applied after trial initiation. The trial was registered before patient enrollment at www.chictr.org.cn (the primary registries of the WHO Registry Network, No. ChiCTR-ROC-16009050, Principal investigator: Yao Weidong, Date of registration: 19 August 2016).
Ethics
This study was prospectively registered at www.chictr.org.cn (trial number: ChiCTR-ROC-16009050). The present study was an investigator-initiated, single-center, prospective observational study conducted from September 2016 to May 2018 at the Yijishan Hospital of Wannan Medical College (People’s Republic of China) and was approved by the Yijishan Hospital’s Institutional Review Board (Chairperson Prof. H. Cao; IRB approval no: (2013)91). Written informed consent was obtained from each participant prior to enrollment. No changes to the methods were applied after trial initiation.
Patients
All adult patients undergoing an elective operation with general anesthesia were considered eligible for this study. The inclusion criteria were as follows: 1) American Society of Anesthesiologists score of <III, 2) planned invasive airway management (orotracheal intubation), 3) age of 18 to 95 years, 4) no history of oral maxillofacial malformation or neck surgery, 5) no missing incisors, and 6) no disturbance of consciousness and the ability to cooperate during a physical examination. The following exclusion criteria were applied: 1) withdrawal of consent, 2) known difficult intubation requiring awake fiberoptic intubation and other strategies, 3) subglottic stenosis, and 4) participation in other studies.
Preanesthetic airway assessments
A preoperative airway evaluation was performed in all patients by assessing the interincisor distance, modified Mallampati score, and thyromental distance. After the patient adaptively opened his or her mouth twice, the interincisor distance was measured as the space between the upper and lower incisors at maximal opening. The modified Mallampati score was determined according to the structure of the pharynx with the patient in a sitting position.8,9 The thyromental distance was measured from the thyroid notch to the tip of the jaw with the head extended.10
Induction protocol for general anesthesia
Before anesthetic induction, vital parameters (heart rate, electrocardiogram, pulse oximetry, and blood pressure) were monitored. Anesthesia was induced with midazolam (0.05 mg/kg), etomidate (0.3 mg/kg), or propofol (1–2 mg/kg); analgesia was provided by sufentanil (0.5–1.0 µg/kg); and neuromuscular blockade was achieved with rocuronium (0.6–0.9 mg/kg). After neuromuscular blockade had been achieved (approximately 3 minutes), direct laryngoscopy and endotracheal intubation were performed by the attending anesthesiologist, who was blinded to the airway assessment results.
The size of the endotracheal tube was selected by the anesthesiologist based on anthropometric measurements. Glottic exposure was graded according to Cormack–Lehane grading system.11 The anesthesiologists were allowed to adjust the laryngoscope position to achieve the best exposure when the first laryngoscopy attempt was performed.
Outcomes
The primary outcome was difficult laryngoscopy, defined as a Cormack–Lehane class 3 or 4 glottis view. To improve glottis exposure, the “BURP” maneuver was performed when Cormack–Lehane class 3 or 4 glottis exposure was encountered.4,5,7 Anesthesiologists who were well trained in the “BURP” maneuver performed the procedure and determined the optimal view of the glottis; the participating residents then followed this procedure. Glottal views with the “BURP” maneuver were also assessed by the attending anesthesiologists.
The attending anesthesiologists who were responsible for the patients had >5 years of experience in performing endotracheal intubation. Difficult intubation was defined as follows2,12: 1) >10 minutes required from blade placement in the mouth to intubation of the patient with conventional laryngoscopy, 2) three or more attempts, or 3) the need for another intubation technique such as fiber bronchoscopy-guided intubation, video laryngoscopy, intubation or ventilation with a laryngeal mask airway, or lighted stylets or light wands. Oxygenation was ensured during the intubation procedure, and mask ventilation was used before the next attempt to ensure that the blood oxygen saturation remained above 98%. In cases of difficult airways, we followed the recommendations of the American Society of Anesthesiologists guidelines.13
Statistical analysis
The SPSS version 16.0 statistical software package (SPSS Inc., Chicago, IL, USA) and MedCalc 12.7 software (MedCalc Software, Ostend, Belgium) were used to analyze the data, and the measured data are expressed as mean ± standard deviation. Grade and classification data are expressed as a frequency distribution. Count data were compared with the I2 test. The results of the diagnosis of difficult tracheal intubation were analyzed using Spearman’s correlation, the diagnostic consistency kappa coefficient, and the area under the receiver operator characteristic (ROC) curve (AUC). The sensitivity, specificity, odds ratio, and positive and negative predictive values for the interincisor distance, modified Mallampati score, and thyromental distance were calculated. The Youden index, which is calculated as the maximal difference between the sensitivity and 1 – specificity for the optimal cut-off point, was used to determine the criteria that predicted difficult laryngoscopy and difficult tracheal intubation. The difference was statistically significant at P < 0.005. Under the conditions of a type I error of <0.05 and type II error of <0.1, the sample of the original study (which included >2000 patients) was sufficient to observe whether the “BURP” maneuver improves the difficult laryngoscopy proportion from 10% to 6%14 and to assess the AUC of predictors for difficult laryngoscopy.
Results
A flow chart of patient inclusion throughout the study is depicted in Figure 1. Among the 2122 patients screened, 94 were excluded; the remaining 2028 patients were included in the analysis. A total of 428 (21%) patients showed a Cormack–Lehane class of 3 or 4 before the “BURP” maneuver. After the “BURP” maneuver, 124 (6.1%) patients were considered difficult laryngoscopy cases and 53 patients were considered difficult intubation cases (see Figure 1). Of the 53 difficult intubation cases, 51 patients were successfully intubated while only 2 patients experienced intubation failure (1 was switched to laryngeal mask ventilation and 1 was converted to awake fiberoptic intubation). Table 1 shows the anthropometric characteristics of the patients with and without difficult laryngoscopy before and after the “BURP” maneuver and the patients with difficult tracheal intubation after the “BURP” maneuver.
Figure 1.
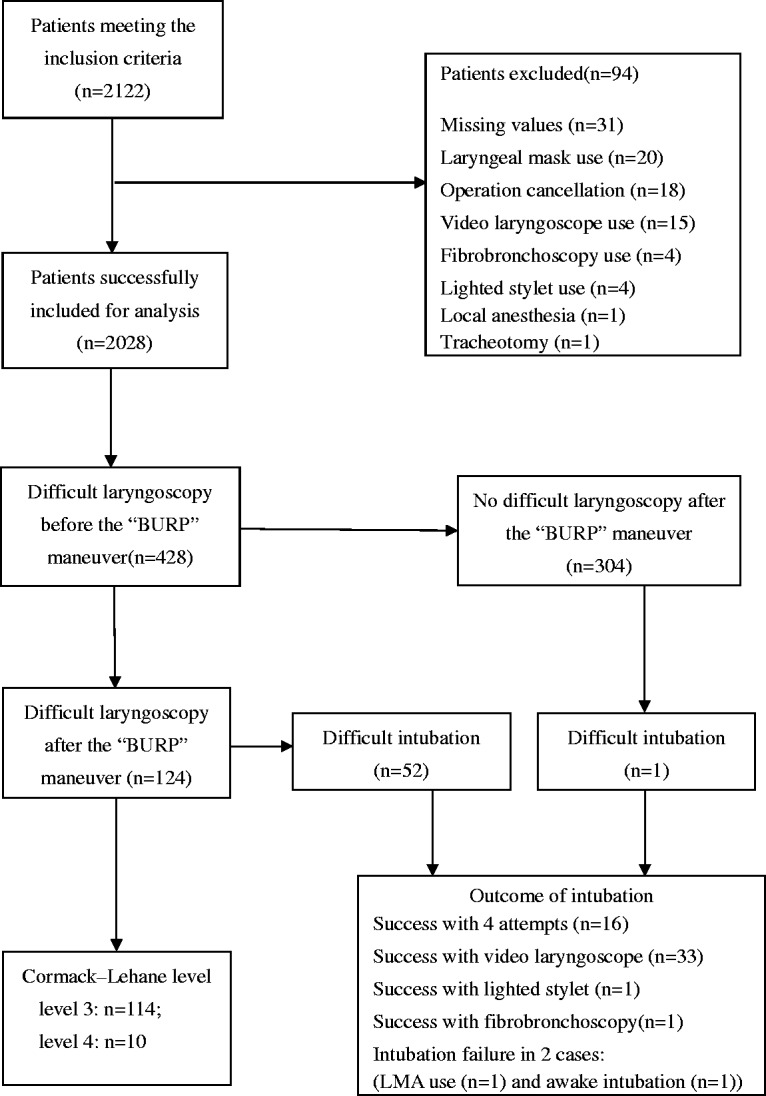
Study flow chart and outcomes of the included patients. LMA, laryngeal mask airway.
Table 1.
Comparison of patients with and without difficult laryngoscopy before and after the “BURP” maneuver.
|
Difficult laryngoscopy before the “BURP” maneuver |
Difficult laryngoscopy after the “BURP” maneuver |
Difficult tracheal intubation after the “BURP” maneuver |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | (Yes)n = 428 | (No) n = 1600 | P value | Effect size | (Yes) n = 124 | (No) n = 1904 | P value | Effect size | (Yes) n = 53 | (No) n = 1975 | P value | Effect size |
| Sex (male/female) | 259/169 | 749/851 | <0.001 | 0.110 | 71/53 | 937/967 | 0.083 | 0.032 | 24/29 | 984/991 | 0.514 | 0.014 |
| Age (years) | 55 ± 13 | 48 ± 15 | <0.001 | 0.031 | 57 ± 13 | 49 ± 15 | <0.001 | 0.038 | 58 ± 11 | 50 ± 15 | <0.001 | 0.039 |
| Body mass index (kg/m2) | 24 ± 3 | 23 ± 3 | 0.004 | 0.046 | 23 ± 4 | 23 ± 3 | 0.373 | 0.024 | 23 ± 3 | 23 ± 3 | 0.525 | 0.026 |
| Thyromental distance (mm) | 75 ± 9 | 79 ± 10 | <0.001 | 0.040 | 71 ± 10 | 78 ± 9 | <0.001 | 0.082 | 67 ± 10 | 78 ± 9 | <0.001 | 0.116 |
| Interincisor distance (mm) | 38 ± 5 | 42 ± 6 | <0.001 | 0.092 | 36 ± 6 | 41 ± 6 | <0.001 | 0.155 | 34 ± 6 | 41 ± 6 | <0.001 | 0.214 |
| Modified Mallampati score of >2 (yes/no) | 114/314 | 205/1395 | <0.001 | 0.155 | 57/67 | 262/1642 | <0.001 | 0.212 | 31/22 | 288/1687 | <0.001 | 0.192 |
Data are shown as mean ± standard deviation or count.
Table 2 shows a comparison of anthropometric data and airway assessment parameters before and after the “BURP” maneuver in patients with difficult laryngoscopy in relation to tracheal intubation success. Patients with difficult laryngoscopy, either before or after application of the “BURP” maneuver, were characterized by shorter interincisor and thyromental distances and a higher rate of a modified Mallampati score of >2.
Table 2.
Comparison of patient changes in difficult laryngoscopy.
|
Difficult laryngoscopy before the “BURP” maneuver |
Difficult laryngoscopy after the “BURP” maneuver |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Difficult tracheal intubation (Yes) n = 53 | Difficult tracheal intubation (No) n = 375 | P value | Effect size | Difficult tracheal intubation (Yes) n = 52 | Difficult tracheal intubation (No) n = 72 | P value | Effect size |
| Sex (male/female) | 24/29 | 235/140 | 0.015 | 0.117 | 23/29 | 48/24 | 0.013 | 0.224 |
| Age (years) | 58 ± 11 | 55 ± 13 | 0.086 | 0.019 | 58 ± 11 | 57 ± 14 | 0.915 | 0.002 |
| Body mass index (kg/m2) | 23 ± 3 | 24 ± 3 | 0.763 | 0.004 | 24 ± 3 | 23 ± 4 | 0.820 | 0.012 |
| Thyromental distance (mm) | 67 ± 10 | 76 ± 9 | <0.001 | 0.098 | 67 ± 10 | 73 ± 8 | 0.001 | 0.065 |
| Interincisor distance (mm) | 34 ± 6 | 39 ± 5 | <0.001 | 0.180 | 34 ± 6 | 38 ± 6 | <0.001 | 0.112 |
| Modified Mallampati score of >2 (yes/no) | 31/22 | 83/292 | <0.001 | 0.271 | 30/22 | 27/45 | 0.026 | 0.120 |
Data are shown as mean ± standard deviation or count.
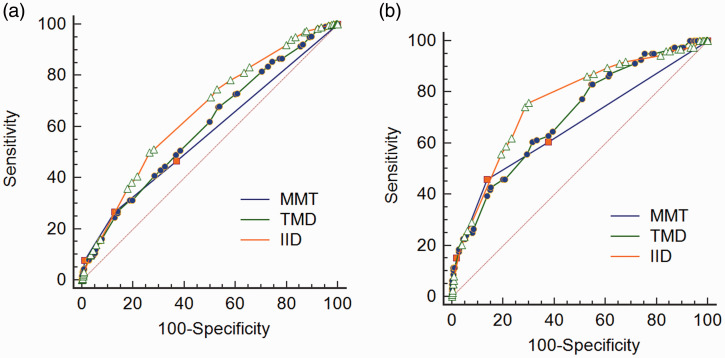
Table 3 shows the AUC, sensitivity, specificity, positive and negative predictive values, and optimal criteria of the thyromental distance, modified Mallampati score, and interincisor distance in predicting difficult laryngoscopy before and after the “BURP” maneuver. ROC curves of the thyromental distance, modified Mallampati score, and interincisor distance for predicting difficult laryngoscopy before and after the “BURP” maneuver are depicted in Figure 2. The AUCs of all predictors improved after the “BURP” maneuver.
Table 3.
Variables for predicting difficult laryngoscopy before and after the “BURP” maneuver (n = 2028).
| Variables | AUC(95% CI) | Criterion | Odds ratio (95% CI) | Sensitivity(95% CI) | Specificity(95% CI) | PPV(95% CI) | NPV (95% CI) | Misclassificationn (%) |
|---|---|---|---|---|---|---|---|---|
| Thyromental distance | ||||||||
| Before the “BURP” maneuver | 0.60 (0.58–0.62) | ≤78 mm | 1.84 (1.47–2.30) | 67.8 (63.1–72.2) | 46.6 (44.2–49.1) | 25.3 (23.9–26.9) | 84.4 (82.4–86.2) | 992 (48.9) |
| After the “BURP” maneuver | 0.71 (0.68–0.73) | ≤73 mm | 3.31 (2.28–4.81) | 60.5 (51.3–69.1) | 68.4 (66.2–70.5) | 11.1 (9.6–12.7) | 96.4 (95.5–97.1) | 651 (32.1) |
| Interincisor distance | ||||||||
| Before the “BURP” maneuver | 0.66 (0.63–0.68) | ≤38 mm | 2.77 (2.23–3.45) | 50.0 (45.2–54.8) | 73.5 (71.3–75.6) | 33.5 (30.8–36.4) | 84.6 (83.3–85.9) | 638 (31.5) |
| After the “BURP” maneuver | 0.76 (0.74–0.78) | ≤39 mm | 7.24 (4.75–11.05) | 75.8 (67.3–83.0) | 69.8 (67.7–71.9) | 14.1 (12.7–15.6) | 97.8 (97.0–98.4) | 578 (28.5) |
| Modified Mallampati score | ||||||||
| Before the “BURP” maneuver | 0.57 (0.55–0.59) | Score of >2 | 2.47 (1.91–3.20) | 26.6 (22.5–31.1) | 87.2 (85.5–88.8) | 35.7 (31.2–40.5) | 81.6 (80.7–82.5) | 519 (25.6) |
| After the “BURP” maneuver | 0.67 (0.65–0.69) | Score of >2 | 5.33 (3.66–7.77) | 46.0 (37.0–55.1) | 86.3 (84.6–87.8) | 17.9 (14.8–21.4) | 96.1 (95.4–96.7) | 329 (16.2) |
AUC, area under the receiver operating characteristic curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value.
Figure 2.
Receiver operating characteristic curve analysis of variables for predicting difficult laryngoscopy (a) before and (b) after the “BURP” maneuver. MMT, modified Mallampati test; TMD, thyromental distance; IID, interincisor distance.
Prediction of difficult intubation
The AUCs of the thyromental distance, modified Mallampati score, and interincisor distance for predicting difficult intubation were 0.77 (95% confidence interval [CI], 0.75–0.79), 0.75 (95% CI, 0.73–0.77), and 0.83 (95% CI, 0.82–0.85), respectively. The prediction criteria for difficult intubation, as determined by the Youden index, were a thyromental distance of ≤70 mm, an interincisor distance of ≤39 mm, and a modified Mallampati score of >2. The AUCs, sensitivities, specificities, positive and negative predictive values, and optimal criteria for the thyromental distance, modified Mallampati score, and interincisor distance for predicting difficult intubation are presented in Table 4. Figure 2 shows the ROC curves of the thyromental distance, modified Mallampati score, and interincisor distance for predicting difficult intubation.
Table 4.
Variables for predicting difficult tracheal intubation (n = 2028).
| Variables | AUC (95% CI) | Criterion | Odds ratio (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | Misclassificationn (%) |
|---|---|---|---|---|---|---|---|---|
| Thyromental distance | 0.77 (0.52–0.79) | ≤70 mm | 5.91 (3.37–10.35) | 60.4 (46.0–73.5) | 79.5 (77.6–81.3) | 7.3 (5.1–10.2) | 98.7 (98.0–99.2) | 626 (30.9) |
| Interincisor distance | 0.83 (0.82–0.85) | ≤39 mm | 20.93 (8.29–52.84) | 90.6 (79.3–96.9) | 68.6 (66.5–70.6) | 7.2 (5.3–9.4) | 99.6 (99.1–99.9) | 426 (21.0) |
| Modified Mallampati score | 0.75 (0.73–0.77) | Score >2 | 8.2 5 (4.71–14.46) | 58.5 (44.1–71.9) | 85.4 (83.8–86.9) | 9.7 (6.7–13.5) | 98.7 (98.1–99.2) | 310 (15.3) |
AUC, area under the receiver operating characteristic curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value.
Diagnostic consistency analysis of difficult laryngoscopy before and after the “BURP” maneuver with difficult intubation
Among the patients with difficult laryngoscopy for whom visualization of the glottis did not improve after the “BURP” maneuver, 41.9% (52/124) were considered to have difficult intubation. Among the patients for whom visualization of the glottis improved after the “BURP” maneuver, only 0.3% (1/304) had difficult intubation.
The paired I2 and agreement tests showed that the kappa value for comparison of difficult tracheal intubation with difficult laryngoscopy before the “BURP” maneuver was 0.18 (95% CI, 0.14–0.23); however, the kappa value for difficult tracheal intubation with difficult laryngoscopy after the “BURP” maneuver was higher at 0.57 (95% CI, 0.48–0.65).
Discussion
To the best of our knowledge, this is the first study to investigate the impact of the “BURP” maneuver on the performance of difficult airway predictors. The impact of this maneuver is illustrated by the improvement in laryngoscopy outcomes. Although all patients were assessed using three airway predictors, only those with initial laryngoscopy difficulties underwent the “BURP” maneuver. This is in line with clinical practice and medical ethics guidelines because for patients with good initial laryngoscopy, the “BURP” maneuver is unnecessary and does not change the classification of the results. The present study showed that the “BURP” maneuver is a meaningful method that can improve laryngoscopy and change the status of difficult laryngoscopy. Interestingly, difficult laryngoscopy became easier to predict when the “BURP” maneuver was used. The ROC analysis showed that the thyromental distance, interincisor distance, and modified Mallampati score had higher AUCs and Youden index values for predicting difficult laryngoscopy with than without “BURP” maneuver. These findings indicate that the “BURP” maneuver renders difficult laryngoscopy more predictable.
Our data show that the “BURP” maneuver reduced the incidence of difficult laryngoscopy (classified as a Cormack–Lehane class 3 or 4 laryngoscopic view) from 21.1% to 6.1% of a total of 2028 patients. These results are similar to those of a study by Ulrich et al.,15 although there is some difference in the incidence of difficult laryngoscopy. Notably, the kappa value of the comparison between difficult tracheal intubation and difficult laryngoscopy before the “BURP” maneuver was 0.18 (95% CI, 0.14–0.23), and this value increased to 0.57 (95% CI, 0.48–0.65) after the “BURP” maneuver. The “BURP” maneuver is an effective method to improve diagnostic agreement between difficult tracheal intubation and difficult laryngoscopy. In other words, the “BURP” maneuver improves the consistency of the concepts of difficult laryngoscopy and difficult intubation in terms of difficult airway management. Consistent with previous studies,4,5,7 the results of our study also confirm that the “BURP” maneuver is a reliable method and that difficult laryngoscopy is easier with the “BURP” maneuver. Knill7 proposed that applying pressure on the thyroid rather than the cricoid cartilage is more effective and that the direction of pressure used to displace the larynx should be backward, upward, and rightward rather than only backward.
Wilson et al.4 used the criterion of an interincisor gap of 5 cm (approximately three finger breadths) to judge jaw movement and predict difficult airways. Khan et al.10 reported that an interincisor distance of <4.5 cm and a thyromental distance of <6.5 cm were predictors of difficult intubation. As noted in the present study, the best cut-off value of the interincisor distance for intubation is ≤39 mm, and the best cut-off value of the thyromental distance for intubation is ≤70 mm. Because of differences between Chinese and Western populations, a criterion of 5.0 or 4.5 cm for the interincisor gap or 6.5 cm for the thyromental distance is not suitable to predict difficult airways in Chinese patients. The present findings are similar to those of our previous study,2 in which we found that to predict difficult tracheal intubation, the best cut-off value of the interincisor distance is <38 mm and the best cut-off value of the thyromental distance is <70 mm. The Mallampati test8,16–18 is a scoring tool commonly used to predict difficult airways. A modified Mallampati score of >2 is an independent predictor of difficult airways.2 Consistent with this, our findings demonstrate that a modified Mallampati score of 3 or 4 indicates a difficult airway.
Study limitations
The present study has several limitations. First, this was a single-center, non-randomized study with a relatively narrow sample. All enrolled patients were older than 18 years and of Han Chinese ethnicity. Differences exist between Western and Asian populations, including differences in height, weight, and body mass index, and the results of the present study should not be arbitrarily extrapolated to Western populations. Large multicenter studies are still needed. Second, we did not perform ultrasonography, computed tomography, or magnetic resonance imaging of patients with difficult intubation because of the limited study conditions; therefore, we lacked the data needed to completely analyze the anatomical factors associated with difficult airways. Third, implementation of the “BURP” maneuver is not a random procedure because only patients with difficult laryngoscopy will undergo this maneuver. In our study, however, the anesthesiologists were scheduled by uninformed management decisions, and whether laryngoscopy difficulties occurred in the patients remained largely unknown. Therefore, although the anesthesiologists were not randomly assigned, there were no predictable factors that would cause bias. In addition, to reduce differences among operators, all anesthesiologists participating in this study were given the same standardized training on the “BURP” maneuver. Fourth, three airway assessment parameters (thyromental distance, modified Mallampati score, and interincisor distance) were assessed in this study because they are the most commonly used indicators of a difficult airway. More importantly, the data in this secondary analysis study are complete and available. Neck circumference and head and neck mobility are also very important; unfortunately, however, too many original data were missing to be used. Fifth, the degree of difficulty with regard to orotracheal intubation was lacking in this study, mainly for the following reasons. The original study defined difficult intubation based on three conditions: 1) >10 minutes required from blade placement in the mouth to intubation with conventional laryngoscopy, 2) three or more attempts prior to successful intubation, or 3) the need for advanced intubation techniques. However, this study lacked measures of intubation difficulty, such as intubation difficulty scores. Although the intubation times were fully recorded in this study, they did not reflect the difficulty of intubation because the Difficult Airway Society 2015 Guidelines for the Management of Unanticipated Difficult Intubation were referenced in the study,13 which limited the number of intubation attempts, and more difficult intubations were classified according to the third version of the standards. Analyzing the success rates of different intubation devices is also challenging; the selection of different intubation tools is difficult to prioritize because it is dependent on the preference and proficiency of the operator.
Conclusion
The “BURP” maneuver is a simple method for improving the management of difficult laryngoscopy. Difficult laryngoscopy was easier to predict with than without the “BURP” maneuver. Moreover, the “BURP” maneuver improved the diagnostic agreement between difficult tracheal intubation and difficult laryngoscopy, which means that difficult laryngoscopy under the “BURP” maneuver is truly “difficult.”
Acknowledgements
We are thankful to our colleagues in the Department of Anesthesiology and the intensive care unit of Wannan Medical College First Affiliated Hospital, Yijishan Hospital, for their help with sample collection.
Authors’ contributions
TY participated in the conception and design of the work; acquisition, analysis, and interpretation of the data; drafting of the manuscript; and revision of the manuscript for important intellectual content. RW participated in the design of the work; acquisition, analysis, and interpretation of the data; and the drafting of the manuscript. FL participated in the acquisition, analysis, and interpretation of the data; drafting of the manuscript; and revision of the manuscript for important intellectual content. BW participated in the conception of the work, acquisition and interpretation of the data, and drafting of the manuscript. MW participated in the design of the work, acquisition and interpretation of the data, and drafting of the manuscript. WY participated in the conception and design of the work; acquisition, analysis, and interpretation of the data; and drafting of the manuscript. XJJ participated in the conception and design of the work; acquisition, analysis, and interpretation of the data; drafting of the manuscript; and revision of the manuscript for important intellectual content. XCJ participated in the conception and design of the work; acquisition, analysis, and interpretation of the data; drafting of the manuscript; and revision of the manuscript for important intellectual content. All authors approved the final version of the submitted work and agreed with all aspects of the article, ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved.
Clinical trial registration
This study was prospectively registered at www.chictr.org.cn (trial number: ChiCTR-ROC-16009050).
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This work was supported by the Key Research and Development Program Projects in Anhui Province (201904a07020034), Hefei, China and Funding of “Peak” Training Program for Scientific Research of Yijishan Hospital, Wannan Medical College (GF2019G05).
ORCID iD
Wei-dong Yao https://orcid.org/0000-0003-0429-4053
References
- 1.Weiser TG, Haynes AB, Molina G, et al. Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet 2015; 385: S11. [DOI] [PubMed] [Google Scholar]
- 2.Yao W, Wang B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? Br J Anaesth 2017; 118: 601–609. [DOI] [PubMed] [Google Scholar]
- 3.Yao W, Zhou Y, Wang B, et al. Can mandibular condylar mobility sonography measurements predict difficult laryngoscopy? Anesth Analg 2017; 124: 800–806. [DOI] [PubMed] [Google Scholar]
- 4.Wilson ME, Spiegelhalter D, Robertson JA, et al. Predicting difficult intubation. Br J Anaesth 1988; 61: 211–216. [DOI] [PubMed] [Google Scholar]
- 5.Takahata O, Kubota M, Mamiya K, et al. The efficacy of the “BURP” maneuver during a difficult laryngoscopy. Anesth Analg 1997; 84: 419–421. [DOI] [PubMed] [Google Scholar]
- 6.Tamura M, Ishikawa T, Kato R, et al. Mandibular advancement improves the laryngeal view during direct laryngoscopy performed by inexperienced physicians. Anesthesiology 2004; 100: 598–601. [DOI] [PubMed] [Google Scholar]
- 7.Knill RL. Difficult laryngoscopy made easy with a “BURP”. Can J Anaesth 1993; 40: 279–282. [DOI] [PubMed] [Google Scholar]
- 8.Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J 1985; 32: 429–434. [DOI] [PubMed] [Google Scholar]
- 9.Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia 1987; 42: 487–490. [DOI] [PubMed] [Google Scholar]
- 10.Khan ZH, Mohammadi M, Rasouli MR, et al. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: a prospective study. Anesth Analg 2009; 109: 822–824. [DOI] [PubMed] [Google Scholar]
- 11.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39: 1105–1111. [PubMed] [Google Scholar]
- 12.Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118: 251–270. [DOI] [PubMed] [Google Scholar]
- 13.Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015; 115: 827–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Detsky ME, Jivraj N, Adhikari NK, et al. Will this patient be difficult to intubate?: The rational clinical examination systematic review. JAMA 2019; 321: 493–503. [DOI] [PubMed] [Google Scholar]
- 15.Ulrich B, Listyo R, Gerig HJ, et al. [The difficult intubation. The value of BURP and 3 predictive tests of difficult intubation]. Anaesthesist 1998; 47: 45–50. [DOI] [PubMed] [Google Scholar]
- 16.Naguib M, Malabarey T, AlSatli RA, et al. Predictive models for difficult laryngoscopy and intubation. A clinical, radiologic and three-dimensional computer imaging study. Can J Anaesth 1999; 46: 748–759. [DOI] [PubMed] [Google Scholar]
- 17.Arne J, Descoins P, Fusciardi J, et al. Preoperative assessment for difficult intubation in general and ENT surgery: predictive value of a clinical multivariate risk index. Br J Anaesth 1998; 80: 140–146. [DOI] [PubMed] [Google Scholar]
- 18.Naguib M, Scamman FL, O’Sullivan C, et al. Predictive performance of three multivariate difficult tracheal intubation models: a double-blind, case-controlled study. Anesth Analg 2006; 102: 818–824. [DOI] [PubMed] [Google Scholar]