The COVID-19 disease pandemic has included over 1 million confirmed infections and more than 50,000 reported deaths worldwide since it began in Wuhan, China, in December 2019 (1). The United States had 374,329 cases and 12,064 deaths by early April 2020 (2). Patients typically present with fever, sore throat, dry cough, dyspnea, malaise, and myalgia (3). Gastrointestinal symptoms present in 3%–50% of cases (3), include nausea, vomiting, abdominal pain, and diarrhea. We have treated 3 men with COVID-19 pneumonia associated with colitis or colonic ileus.
Case 1: A 38-year-old, previously healthy man presented with fever, chills, myalgias, dyspnea, severe diffuse abdominal pain, and diarrhea for 4 days after exposure to his ill wife and children. He denied chest pain, dysuria, nausea, and vomiting. His temperature was 102.7 °F, respiratory rate 18 breaths/min, oxygen saturation 92%, heart rate 80 beats/min, and blood pressure 140/70 mm Hg. Examination revealed an ill appearance, diffuse rales bilaterally and tenderness of the left and right lower abdominal quadrants. Laboratory results included a normal white blood cell count (WBC), lymphopenia (19.5%), neutrophilia (73%), monocytosis (13%), and elevated alanine aminotransferase (ALT, 87 U/L), aspartate aminotransferase (AST, 53 U/L), C-reactive protein (CRP, 69 mg/L), lactate dehydrogenase (LDH, 261 U/L), and creatine phosphokinase (131 U/L). X-ray and computed tomography (CT) of the chest showed bilateral ground glass opacities (GGOs). Abdominal CT demonstrated thickening of the ascending, transverse, descending, and sigmoid colon and rectum consistent with colitis (Figure 1). A nasal swab was positive for COVID-19 by real-time reverse transcriptase polymerase chain reaction (RT-PCR). We treated him in hospital with off-label hydroxychloroquine, 400 mg b.i.d. on day 1, followed by 400 mg q.d. for 4 days, and azithromycin 500 mg q.d. and zinc sulfate 220 mg q.d. for 5 days. Patient was admitted for total of 5 days followed by clinical improvement, and then, he was discharged with instruction about 2 weeks of home quarantine.
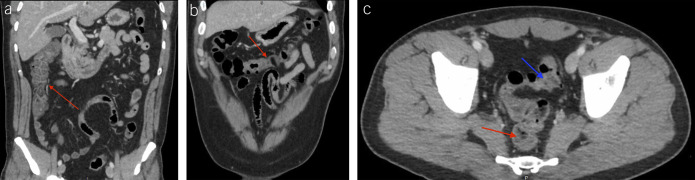
Figure 1.
Abdominal computed tomography showing thickening of the ascending (a, red arrow), transverse (b, red arrow), and left colon (c, blue arrow).
Case 2: A 55-year-old man with hypertension, hyperlipidemia, and diabetes presented with fever, cough, nausea, constipation, and abdominal pain for 7 days. He denied diarrhea, chest pain, dysuria, vomiting, travel, sick contacts, pets at home, or narcotic ingestion. His temperature was 102.5 °F, respiratory rate 18 breaths/min, oxygen saturation 92%, heart rate 101 beats/min, and blood pressure 125/72 mm Hg. He appeared in no distress, but he had diffuse rales bilaterally and tenderness of the right lower abdominal quadrant. He had a normal WBC, neutrophilia (82%), lymphopenia (18%), and elevated ALT (76 U/L), AST (70 U/L), CRP (63 mg/L), and LDH (369 U/L). Computed tomography of the chest showed bilateral GGOs. Abdominal CT showed colonic ileus and air in the bowel wall (Figure 2). A nasal swab was positive for COVID-19 by RT-PCR. He received the same drug therapy as case 1 for 2 days in hospital, and 3 days as an outpatient, recovered, and initiated 2 weeks of home quarantine.
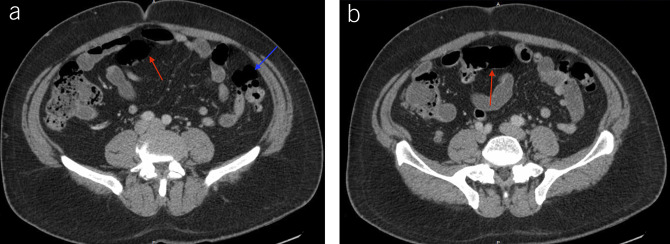
Figure 2.
Abdominal computed tomography showing colonic ileus with air fluid levels (a and b, red and blue arrows).
Case 3: A 74-year-old man with type 2 diabetes, hyperlipidemia, and benign prostatic hypertrophy presented with dry cough for 1 week and diffuse abdominal pain for 1 day. He denied chest pain, constipation, diarrhea, dysuria, previous surgeries, travel, trauma, or sick contacts. His temperature was 101 °F, respiratory rate 16 breaths/min, oxygen saturation 96%, heart rate 80 beats/min, and blood pressure 104/61 mm Hg. He appeared in no distress, but he had mild bilateral lower lobe rales and a nondistended, nontender abdomen. He had a normal WBC, lymphopenia (14.2%), neutrophilia (77%), monocytosis (11%), and elevated ALT (70 U/L), AST (59 U/L), CRP (156 mg/L), LDH (277 U/L), and d-dimer (562 ng/mL). Computed tomography of the chest showed bilateral GGOs and thickening of the proximal transverse colon (Figure 3). A nasopharyngeal swab was positive for COVID-19 RT-PCR. He received the same drug therapy as cases 1 and 2 during his hospitalization for 5 days and was quarantined at home after recovery.
Figure 3.

Abdominal computed tomography showing thickening of the proximal transverse colon (red arrow).
Gastrointestinal manifestations of COVID-19 are less common than pulmonary disease (3). Gastrointestinal symptoms may be linked to binding of the SARS-CoV-2 virus to angiotensin-converting enzyme-2 receptors throughout the gut, leading to upregulation of this receptor and elevated transaminase levels (4). Like other viral gastrointestinal infections, COVID-19 may cause inflammation directly through cellular infection or indirectly by cytokines produced with inflammation. Therefore, the virus can be detected in stool (5). A common mucosal immune system response may underlie both pulmonary and gastrointestinal manifestations (6).
Although the most commonly reported digestive symptoms in COVID-19 disease are anorexia, diarrhea, and vomiting, constipation and abdominal pain can also occur. These symptoms may precede or be accompanied by fever, fatigue, myalgia, and respiratory symptoms (3). Han et al. (5) recently reported that patients with concurrent upper and lower digestive symptoms have a higher incidence of fever compared with patients with only upper or lower gastrointestinal symptoms. Patients with digestive symptoms had a longer period from symptom onset to hospital admission compared with patients without these symptoms (3,5), possibly due to mild symptoms or lack of awareness of gastrointestinal manifestations of COVID-19 disease. Gastrointestinal symptoms may occur early, as in our cases.
Lymphopenia, elevated transaminases, and impaired coagulation function occur in COVID-19 disease patients (3). As in our patients, severe cases are associated with neutrophilia and an elevated neutrophil-to-lymphocyte ratio (7). Serum AST and ALT are higher in patients with gastrointestinal symptoms compared with other patients (3).
Stool testing should be considered in patients presenting with gastrointestinal symptoms when a nasopharyngeal swab test is negative and COVID-19 disease is suspected (5). Endoscopy and colonoscopy generate aerosols, endangering medical staff, and should generally be limited to patients with life-threatening gastrointestinal bleeding or esophageal foreign-body obstruction (8).
Our patients manifested large bowel involvement in COVID-19 disease. They received off-label hydroxychloroquine, azithromycin, and zinc sulfate (9,10). Rigorous clinical trials of this treatment are lacking.
CONFLICTS OF INTEREST
Guarantor of the article: Yasar Sattar, MD.
Specific author contributions: The first 3 authors were involved in drafting the manuscript. All the authors were involved in reviewing the manuscript, editing and participated in submission.
Financial support: None to report.
Potential competing interests: None to report.
REFERENCES
- 1.Coronavirus COVID-19 global cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) (https://coronavirus.jhu.edu/map.html). Accessed March 23, 2020.
- 2.CDC. Cases in US. (https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html). 2020. Accessed March 23, 2020.
- 3.Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study. Am J Gastroenterol 2020;115(5):766–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan GW, Gao L, Wang JW, et al. Exploring the mechanism of liver enzyme abnormalities in patients with novel coronavirus-infected pneumonia. Zhonghua Gan Zang Bing Za Zhi 2020;28:E002. [Chinese] [DOI] [PubMed] [Google Scholar]
- 5.Han C, Duan C, Zhang S, et al. Digestive symptoms in COVD-19 patients with mild disease severity: Clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol 2020;115(6):801–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Budden KF, Gellatly SL, Wood DL, et al. Emerging pathogenic links between microbiota and the gut-lung axis. Nat Rev Microbiol 2017;15:55–63. [DOI] [PubMed] [Google Scholar]
- 7.Liu J, Liu Y, Xiang P, et al. Neutrophil-to-lymphocyte ratio predicts severe illness patients with 2019 novel coronavirus in the early stage. medRxiv 2020. 10.1101/2020.02.10.20021584. Accessed March 22, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tse F, Borgaonkar M, Leontiadis GI. COVID-19: Advice from the Canadian Association of Gastroenterology for Endoscopy Facilities, as of March 16, 2020. J Can Assoc Gastroenterol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gautret P, Lagier J-C, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020:105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 10.Fischer Walker C, Black RE. Zinc and the risk for infectious disease. Annu Rev Nutr 2004;24:255–75. [DOI] [PubMed] [Google Scholar]