ABSTRACT
Background:
The COVID-19 pandemic has drastically changed healthcare systems and training around the world. The Training Committee of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition sought to understand how COVID-19 has affected pediatric gastroenterology fellowship training.
Methods:
A 21 question survey was distributed to all 77 pediatric gastroenterology fellowship program directors (PDs) in the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition program director database via email on April 7. Responses collected through April 19, 2020 were analyzed using descriptive statistics.
Results:
Fifty-one of 77 (66%) PDs from the United States, Canada, and Mexico responded to the survey. Forty-six of 51 (90%) PDs reported that they were under a “stay-at-home” order for a median of 4 weeks at the time of the survey. Two of the 51 (4%) programs had fellows participating in outpatient telehealth before COVID-19 and 39 of 51 (76%) at the time of the survey. Fellows stopped participating in outpatient clinics in 22 of 51 (43%) programs and endoscopy in 26 of 51 (52%) programs. Changes to inpatient care included reduced fellow staffing, limiting who entered patient rooms, and rounding remotely. Fellows in 3 New York programs were deployed to adult medicine units. Didactics were moved to virtual conferences in 47 of 51 (94%) programs, and fellows used various online resources. Clinical research and, disproportionately, bench research were restricted.
Conclusions:
This report provides early information of the impact of COVID-19 on pediatric fellowship training. Rapid adoption of telehealth and reduced clinical and research experiences were important changes. Survey information may spur communication and innovation to help educators adapt.
Keywords: COVID-19, fellowship, graduate medical education, telehealth
What Is Known/What Is New
What Is Known
The COVID-19 pandemic has drastically altered healthcare throughout the world.
Nonemergent outpatient care and procedures and laboratory and clinical research form the core of pediatric gastroenterology fellowship training, and have been restricted.
What Is New
This is an early report of the impact of COVID-19 on pediatric fellowship trainees, and it describes varying degrees of disruptions in clinical and scholarly activities.
Fellowship programs have rapidly transitioned to telehealth, virtual didactics, and other online learning resources.
The COVID-19 pandemic has drastically changed the behavior of individuals and communities around the world, including healthcare organizations. The typical operations of medical practices, hospitals, and academic health centers have been upended in response to the pandemic. In the United States, for example, government orders, Centers for Disease Control and Prevention and Surgeon General advice, and local practices have aimed to reduce contact with others, increase hospital capacity to care for surges of patients sickened by the virus, reduce risk of infection among healthcare providers and conserve limited personal protective equipment (PPE) (1–4). Nonemergent procedures and surgeries have been cancelled or postponed, clinic visits have been transitioned to telehealth, and inpatient hospital censuses have dropped in many areas, especially for children's hospitals (1). Although COVID-19-related research has skyrocketed, other research operations have been grounded or restricted (2,3). These pervasive changes have affected healthcare trainees through reduced typical clinical exposure, redeployment of trainees to new roles, reduced research activity, and alterations to in-person learning activities such as conferences and lectures (4,5). The Training Committee of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) sought to understand how COVID-19 has affected pediatric gastroenterology fellowship training in North America and to help these training programs share how they were managing changes in clinical work (including telehealth), teaching and learning, research activities, and endoscopy training.
METHODS
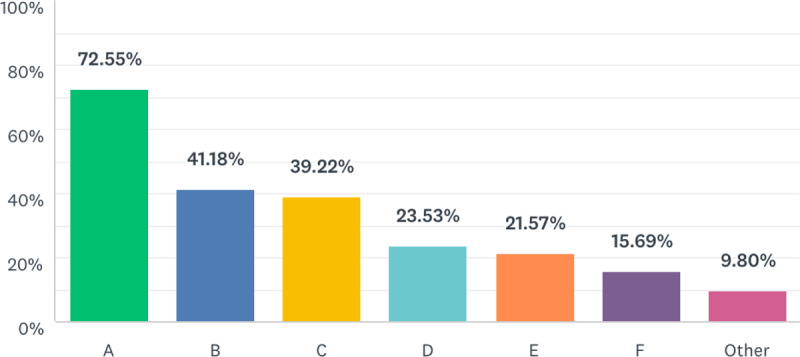
A survey was developed by leaders of the NASPGHAN Training Committee and distributed to committee members for feedback regarding comprehension and solicitation of new, pertinent questions. After iterative editing and committee approval, committee leaders distributed a weblink to complete the survey in SurveyMonkey (San Mateo, CA) via email on April 7, 2020 to all 77 program directors (PDs) in the NASPGHAN program director database (Table 1). One reminder was sent on April 13, 2020. Responses were collected through April 19, 2020. Respondents were directed to answer questions related to pediatric gastroenterology fellows and not to subspecialized advanced training fellows (transplant hepatology, neurogastroenterology, interventional endoscopy, etc). Descriptive statistics were used to analyze responses using Excel (Microsoft, Redmond, WA) and SurveyMonkey software. Free text answers were abstracted and quoted directly or grouped in themes by the authors. Information about programs that did not respond was collected from the NASPGHAN PD database.
TABLE 1.
Fellowship program characteristics
RESULTS
Fifty-one of 77 (66%) PDs responded to the survey, including PDs from Canada, Mexico, and all regions of the United States. Forty-two programs (82%) had 6 or fewer fellows across all 3 years, and half were associated with freestanding children's hospitals (Table 1). A large majority of PDs, 46 of 51 (90%), reported their area was under a “stay-at-home” order, with median duration of 4 weeks at the time of their response.
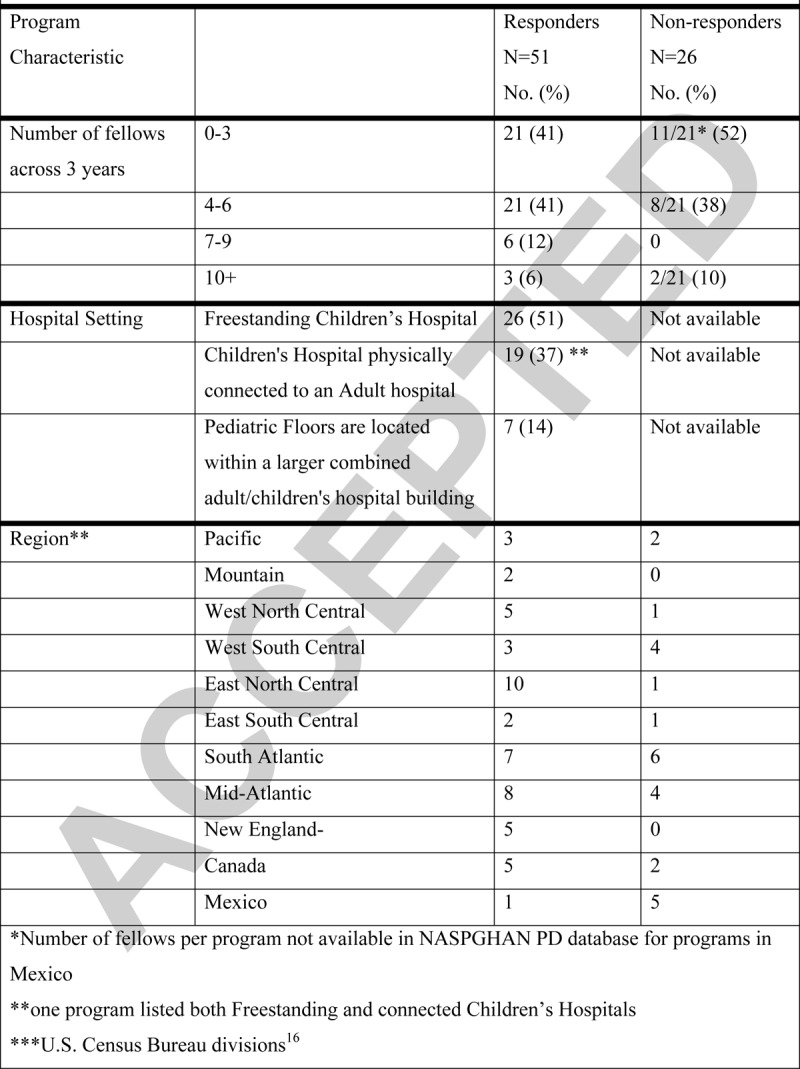
PDs were asked about fellows’ utilization of telehealth for outpatients before the COVID-19 pandemic. Forty-nine (98%) programs indicated they did not use telehealth in the pre-COVID-19 era. In the COVID-19 era, 39 (76%) of programs reported having fellows use telehealth. Of the programs that were engaging fellows in telehealth, 33 estimated the number of telehealth visits per week per fellow, with a median of 5 visits (range 1–25). There was a variety of ways that faculty managed telehealth visits with fellows (Fig. 1). Some individual programs reported multiple methods. Counting programs who only indicated the fellow and attending were in the same room, 14 of 51 (27%) were conducting visits with the attending present for the entire telehealth call. For 22 of 51 (43%) programs, fellows had stopped seeing patients in clinic. Fifteen of these 21 (68%) programs had fellows participating in telehealth, and 7 programs’ fellows were not seeing outpatients in clinic or via telehealth. The remaining 29 programs had continued having fellows see outpatients in-person, and comments indicated these patients were selected, urgent patient visits, resulting in fewer visits for fellows. Eight of the 29 (28%) programs with fellows still seeing outpatients in clinic estimated fellows were seeing 1 to 2 patients per fellow per week, and 29 programs (31%) reported fellows seeing 3 to 6 patients in-person in clinic per week. Twenty-four of 29 programs (83%) with fellows attending in-person clinics were also including fellows in telehealth.
FIGURE 1.
How fellows operate telehealth visits with their faculty preceptors. A, Fellow and attending in the same room, doing the telehealth visit from the same computer. B, Fellow and attending on separate computers, attending on video call for the entire visit. C, Fellow conducts the majority of the telehealth visit alone. BEFORE the call is completed, attending joins VIDEO CALL. D, Fellow conducts the majority of the telehealth visit alone. BEFORE the call is completed, fellow calls the attending on the PHONE. E, Fellow conducts the entire telehealth visit alone. AFTER completing the call, fellow calls the attending on the PHONE. F, Not applicable—fellows are not participating in telehealth.
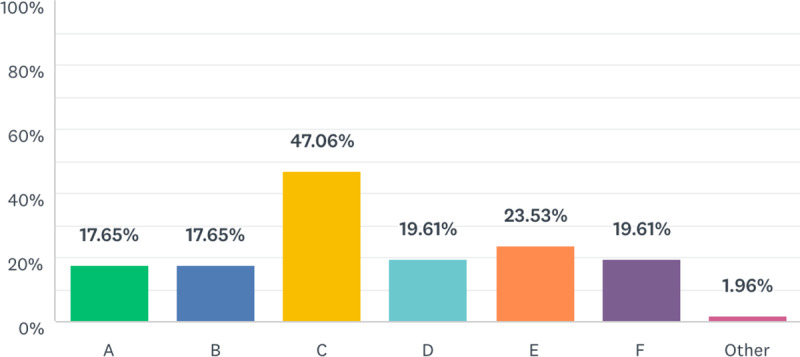
When asked about fellows working on the inpatient hospital service, 26 of 51 (51%) programs had reduced the number of on-site fellows seeing inpatients as follows, including 14 of 51 (27%) cutting the number by 50% or more. Eight (16%) of programs reported no significant changes in how fellows were engaging in inpatient rounds and consults, but for most programs, fellows were limiting in-person contact in various ways (Fig. 2). In 26 (52%) programs, fellows were not participating in endoscopy procedures.
FIGURE 2.
Changes to inpatient rounds and consults. A, The number of staff and trainees allowed in patient rooms for examinations have been reduced. B, Fellows are not going into patient rooms unless deemed important/necessary. C, Some/all of patient/family conversations with inpatient teams are now done remotely. Examinations are still being performed in person. D, Inpatient consult discussions with the patient/family and consulting teams are done remotely by video or phone call. Examinations are performed in person. E, Fellows are going into most patient rooms with the attending. F, No significant changes (other than personal protective equipment [PPE] requirements).
Call schedules were changed in 21 of 51 (41%) programs, with comments about adjusting duties for fellows who were pregnant, had other health conditions, had childcare needs, or had spouses working emergency department or intensive care unit shifts. Some PDs noted they adjusted call schedules to allow fellows 2 weeks without call duties following a period of service, modified backup call schedules, or had fellows staying at home take call to allow rest for fellows on service. Three of six New York City-area programs reported that some of their fellows were redeployed to adult medicine teams, and 2 of the remaining 3 commented “expected any day now” and “awaiting redeployment.”
Of the 50 PDs who responded to a question regarding changes in education resources, 47 of 50 (92%) had started using online audio/video virtual conference platforms for meetings or lectures, 26 of 50 (52%) reported offering readings and 6 of 50 (12%) were using prerecorded lectures. PDs reported using the following educational resources: NASPGHAN curricular resources and videos, American Academy of Pediatrics PREP GI, the NASPGHAN Bowel Sounds podcast, American College of Gastroenterology Online activities, Journal of Pediatric Gastroenterology and Nutrition CME activities, Abbott lectures, Crohn Disease Exclusion Diet modules, and the NASPGHAN Nutrition University (N2U) Nutrition curriculum.
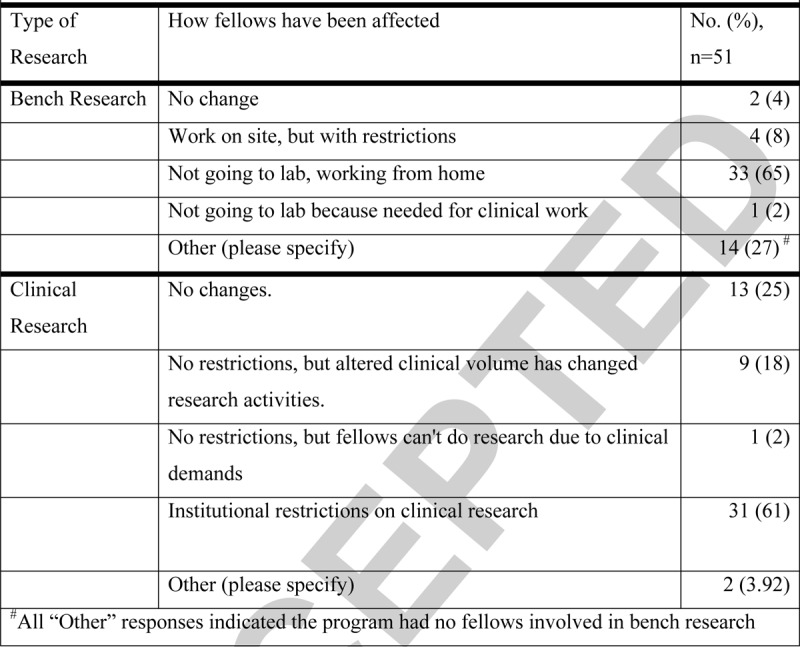
Regarding bench laboratory research, 14 of 51 (27%) programs reported they had no fellows involved in bench research. Of the remaining 37, 33 (89%) programs reported their fellows were not going to the laboratory and were working from home (Table 2). For programs with fellows involved in clinical research, 25% of programs reported no changes, and 31 of 51 (61%) programs reported their institution had placed restrictions on clinical research (Table 2).
TABLE 2.
Impact of COVID-19 on bench and clinical research activities of fellows
PDs were asked to share changes they felt were critical to their COVID response. Responses were varied but reflected prior survey responses related to reduced interpersonal and patient exposure, institution of telemedicine, and adapting conferences and personal check-ins to virtual meetings (Supplemental Digital Content, Table:).
PDs also were asked what they were most interested to learn from other programs regarding COVID fellowship changes (Supplemental Digital Content, Table:). Themes that emerged included ensuring fellows’ readiness for independent care and credentialing, safety and missed opportunities regarding endoscopy, implementation of telemedicine, and addressing fellow wellness.
DISCUSSION
PDs who responded to this survey represent all regions of the United States and include some programs in Canada and Mexico. Although there may be relatively lower representation of programs from South Atlantic and West South Central regions and Mexico, the sizes of fellowships were similar between programs who responded and those who did not respond. The impact of COVID-19 on fellowship training is pervasive, but to varying degrees regarding clinical duties, including call, inpatient service, and outpatient visits, and research activity. Restrictions regarding in-person clinical work were nearly universal, and new models and methods have been used for engaging fellows in inpatient work with less physical contact with patients and colleagues including outpatient encounters using telehealth and learning using virtual conferences and online resources. Research activity in bench-based and clinical research has been restricted for most programs. Although PDs from all regions of the United States, Canada, and Mexico reported changes due to COVID-19, the timing of the virus's impact may depend on location and population. Only New York programs reported redeploying fellows to other clinical areas, but some other programs in Philadelphia, Baltimore, and Montreal indicated they had plans in place or were preparing for it at the time of their response. The duration of the need for these responsive changes and future adaptations is unknown, and this survey of pediatric gastroenterology PDs echo questions that have been raised by educators in other specialties (6).
The Accreditation Council of Graduate Medical Education(ACGME) has issued some guidance to the US programs, although recommendations for reducing clinical encounters or increasing the ability of trainees to work in new ways have not been firmly established (4,7). The accreditation body has not changed work-hour restrictions and has reiterated calls for adequate supervision, training, and provisions for safety in the work environment. They also have recommended continued didactic training using Web-based remote conferencing, which our survey respondents are doing (4).
The ACGME accelerated its implementation of telemedicine guidance to make them effective from March 18. Under these requirements, residents and fellows are permitted to use telemedicine under direct supervision where the “supervising physician and/or patient is not physically present with the resident and the supervising physician is concurrently monitoring patient care through appropriate telecommunication technology (4).” A clarification statement was, however, posted on March 20, stating “We want to be clear that those residents and fellows who are capable of providing this service (telemedicine) with indirect supervision available or immediately available are covered under the indirect supervision requirements(8).” The post also reminds readers that graded supervision from direct to indirect is at the discretion of programs for typical care, and indicates that decisions for implementing supervision of telehealth should be made at the program level. PD respondents to our survey reported rapid but variable implementation of telehealth. Only 14 of 51 (27%) programs indicated the attending was present by video the whole time, and 12 programs, nearly 1 quarter of programs, reported the attending did not staff the patient encounter until after the call was completed suggesting that no current clear path exists for attendings staffing fellows during telehealth.
The Center for Medicare and Medicaid Services has added an interim rule during this public health emergency that allows payment for services provided by teaching physicians as long as they are present during the key portions of the service, using interactive telecommunications technology. Center for Medicare and Medicaid Services defines interactive telecommunication as requiring real-time, 2-way, audio and video telecommunication (5). This rule includes supervision of telehealth visits conducted by a resident (or fellow). Implementation of telehealth supervision practices is informed by the ACGME, by hospital and university guidance, and by payors, and PDs should familiarize themselves with relevant policies.
Rapid and wide uptake of telehealth may present new opportunities for appropriate clinical care and training applicable to existing telehealth practices. Teaching through apprenticeship and role modeling is the foundation of graduate medical education, and telehealth should be no exception. Berg et al (9), recently published a “Playbook” for rapid implementation of telehealth during the pandemic, including best practices adapted from American Academy of Pediatrics and American Medical Association and specific applications in pediatric gastroenterology.
The ACGME also has recognized the reduced clinical volume and potential for trainees not achieving recommended numbers of cases or procedures and has left decisions about determining whether a graduating resident/fellow is “prepared for unsupervised practice to PDs with consideration of the program's Clinical Competency Committee” (4). PDs for Pediatric Subspecialty Fellowships received a letter on April 13, 2020 from the American Board of Pediatrics with corollary guidance for PDs as they submit Verification of Clinical Competence forms for graduating fellows (10). That letter does specifically recommend additional clinical experiences for nonfinal year trainees to make up for lost opportunities in the COVID era.
Our study indicates pediatric gastroenterology fellows’ research activities have been curtailed, with a disproportionate 89% of those involved in bench research not coming to the laboratory compared with 64% of programs reporting restrictions for fellows involved in clinical research. Whether scaling back research for fellows will translate into delayed progress is yet unknown, but it does raise concerns about lost opportunities to generate the research that could allow timely completion of manuscripts or grants that drive early academic career development and which are needed as evidence of scholarly activity for graduation and board certification. Potential ways to keep research active during the COVID-19 pandemic include redesigning studies to be less labor intensive, having the ability for open communication regarding research progress, prioritization of necessary outcomes, considering alternative methods for collecting data, and working remotely to work on outcomes data (11,12). For some fellows, reduced clinical workload and stalled research projects may present opportunities for alternative scholarly activities such as curriculum development, retrospective studies, and reviews that do not require presence in a laboratory or clinical encounters. Although some allowances for altered clinical training have been addressed by the ACGME and American Board of Pediatrics, the impact on scholarly activity requirements has not been addressed in detail. The American Board of Medical Specialties signed on to a statement of the Coalition for Physician Accountability recognizing the “extreme disruption” to student, resident, and fellow training, licensing, and credentialing and will provide guidance for how to manage that impact (13).
Regulatory guidance that recognizes the disruption, reinforces the importance of learner safety and supervision, and underscores competency-based assessment is welcome. However, regulations only go so far to inform educators in the day-to-day adjustments to teaching and learning in our specialty, especially in the setting of the current COVID-19 pandemic. Residents and fellows are crucial in many settings, especially for busy inpatient services. Adjusting staffing of inpatient service and on-call duties was a theme in our survey responses with consideration of limiting contact with patients and each other, personal health risks, childcare obligations, and the potential for trainees to become ill or enter quarantine due to suspected exposure. Some respondents mentioned addressing fellow wellness and morale, and the emotional toll on trainees merits attention (6,14). Our survey is meant to inform and spur communication among pediatric gastroenterology fellowship directors, and others, so we can learn from each other.
About half of the programs in our study reported that fellows were no longer participating in endoscopy in the COVID-19 era. This is a tremendous loss of learning opportunities for skills that are integral to our subspecialty. Adapting to the needs to protect learners and coworkers and to conserve PPE likely drives this change, and careful consideration is needed to readdress these concerns as assessments of risk and PPE supply change in the coming weeks and months. To maximize educational value, fellows can still be involved in the decision-making surrounding timing and type of procedures performed as well as interpretation of findings for actual cases. In addition, programs with endoscopy simulators can encourage fellows to practice their endoscopy skills, assuming they can sanitize equipment and comply with social distancing guidance. Training in video capsule endoscopy or pH-impedance studies also can be considered, if fellows have access to software with synchronous or asynchronous feedback from experienced supervisors. Curating and generating other educational activities related to endoscopy may be taken up by programs, or perhaps through collaborative work of relevant NASPGHAN committees, including ours. For programs more severely impacted, with prolonged and pervasive disruption of face-to-face clinical and endoscopy training, the threat to their capacity to train fellows to acceptable competency is chilling and may require special consideration to support those programs.
This report provides early information of the impact of COVID-19 on the training of pediatric fellows. Although the COVID-19 era has altered patient care and reduced opportunities for learning procedural skills, development of other competencies can continue. There is value in many online interactive and self-directed learning activities that help our fellows build knowledge including those listed by the PDs in our survey. Multicenter or NASPGHAN-facilitated efforts to offer online educational activities in addition to those already available (15) may help ease the burden on individual programs and educators. There also is value in engaging fellows in divisional and institutional responses to COVID-19, encouraging reflection and self-care, and practicing telehealth to foster development of competencies in professionalism, systems-based practice, and adapted interpersonal and communication skills. How long COVID-19 will affect our typical training environment and practices remains unknown, but with resourcefulness, collaboration, innovation, and grace, we are able to adapt and to carry on preparing our fellows for independent practice.
Supplementary Material
Footnotes
Disclaimer: Dr. Cade M. Nylund is employed by the United Stated Air Force. The views expressed in this article do not reflect the official policy of the US Air Force, Department of Defense or the US government.
The authors report no conflicts of interest.
Contributor Information
Collaborators: NASPGHAN Training Committee COVID-19 Survey Working Group
REFERENCES
- 1. Sternberg S. usnews.com. US News & World Report. https://www.usnews.com/news/health-news/articles/2020-04-10/coronavirus-is-causing-a-reshuffling-of-pediatric-care. Published April 10, 2020. Accessed April 17, 2020. [Google Scholar]
- 2. Servick K, Cho A, Guglielmi G et al. Updated: labs go quiet as researchers brace for long-term coronavirus disruptions. Science Magazine Web site. https://www.sciencemag.org/news/2020/03/updated-labs-go-quiet-researchers-brace-long-term-coronavirus-disruptions#. Published March 16, 2020. Accessed April 17, 2020. [Google Scholar]
- 3. Coronavirus Disease 2019 (COVID-19): Information for NIH Applicants and Recipients of NIH Funding. National Institutes of Health Web site. https://grants.nih.gov/policy/natural-disasters/corona-virus.htm. Published March 10, 2020. Accessed April 16, 2020. [Google Scholar]
- 4. Nasca T. ACGME Response to the Coronavirus-COVID-19. Letters to the Community. Accreditation Council for Graduate Medical Education Web site. https://www.acgme.org/Newsroom/Newsroom-Details/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19. Letter posted March 18, 2020. Accessed April 15, 2020. [Google Scholar]
- 5. Centers for Medicare and Medicaid Services. Medicare and Medicaid Programs; Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency. Centers for Medicare and Medicaid Web site. https://www.cms.gov/files/document/covid-final-ifc.pdf. Published March 24, 2020. Accessed April 19, 2020. [Google Scholar]
- 6.Anderson ML, Turbow S, Willgerodt MA, et al. Education in a crisis: the opportunity of our lives. J Hosp Med 2020; 15:287–291. [DOI] [PubMed] [Google Scholar]
- 7.Potts JR., 3rd Residency and fellowship program accreditation: effects of the novel coronavirus (COVID-19) pandemic. J Am Coll Sur 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ACGME Response to COVID-19: Clarification regarding Telemedicine and ACGME Surveys. ACGME Blog. https://www.acgme.org/Newsroom/Blog/Details/ArticleID/10125/ACGME-Response-to-COVID-19-Clarification-regarding-Telemedicine-and-ACGME-Surveys. Published March 20, 2020. Accessed April 20, 2020. [Google Scholar]
- 9.Berg EA, Picoraro JA, Miller SD, et al. COVID-19: a guide to rapid implementation of telehealth services: a playbook for the pediatric gastroenterologist. J Pediatr Gastroenterol Nutr [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Woods SK. Pediatric Subspecialty Fellowship Program Directors and Coordinators of Gastroenterology. E-mail communication April 13, 2020. [Google Scholar]
- 11.Gewin V. Safely conducting essential research in the face of COVID-19. Nature 2020; 580:549–550. [DOI] [PubMed] [Google Scholar]
- 12.McDermott MM, Newman AB. Preserving clinical trial integrity during the coronavirus pandemic. JAMA [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 13. Safeguard the Public, Protect our Health Care Workforce during the COVID-19 Pandemic. American Board of Medical Specialties Web site. https://www.abms.org/news-events/safeguard-the-public-protect-our-health-care-workforce-during-the-covid-19-pandemic/. Published April 9, 2020. Accessed April 19, 2020. [Google Scholar]
- 14.Gallagher TH, Schleyer AM. “We Signed Up for This!” - Student and Trainee Responses to the Covid-19 Pandemic. New Engl J Med XXX; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 15. Curricular Resources. North American Society for Pediatric Gastroenterology Hepatology and Nutrition Web site. https://naspghan.org/training-career-development/for-fellowship-directors/curricular-resources/. Published 2019. Accessed April 27, 2020. [Google Scholar]
- 16. US Census Bureau Regions and Divisions. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed April 19, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


