In France, as in most countries, strict strategies were implemented in cancer hospitals to reduce the spread of coronavirus (COVID-19), but to maintain as much as possible the capacity of oncology health services [1], [2]. These strategies included the reduction of elective services, an emphasis on remote visits, and the use of personal protective equipment [3], [4], [5], [6], [7]. International radiation therapy (RT) academic societies proposed to restrict the indications for treatment [8], to delay as long as possible the start of non-urgent treatments and to prefer hypofractionated regimens [9], [10], [11], [12], [13], [14], [15], [16]. To our knowledge, none of these recommendations anticipated how to handle the load of delayed treatments after the lockdown. However, the successful management of cancer treatments during lockdown undoubtedly correlates with the successful management of post-lockdown activity overload.
The Institut Curie has one of the largest RT departments in Europe. It is spread over three separate sites in the Paris area and has a total of eleven LINACs (six in Paris, four in Saint-Cloud and one in Orsay) and three treatment rooms for proton therapy in Orsay. In 2019, 5,860 patients were treated and the average number of treatment essions per month delivered was 8931, comprising 4183 sessions in Paris, 3303 in Saint-Cloud and 1445 in Orsay. In order to comply with the international recommendations mentioned above, several measures had to be applied in our department to protect both patients and operators from the risk of contamination. The challenges of post-crisis management following the COVID-19 pandemic therefore had to be anticipated. Here, we propose some key considerations to prepare for the post-lockdown period by presenting the guidelines adopted by the RT department of the Institut Curie.
During the French lockdown (in France from 17/03/20 to 11/05/20), priorities were established in order to limit the number of treatments. All indications for exclusive RT, whether or not combined with concomitant chemotherapy, were initiated without delay. These indications included not-yet-resected tumors (head and neck cancer, neurological cancer including glioblastoma, lung cancer, pediatric cancer, etc.), but excluded prostate cancer and metastatic tumours requiring local treatment, whatever the primary. Preoperative RT, stereotactic body RT, gynecological brachytherapy and proton therapy were provided throughout the lockdown without modifying the delay and the number of sessions (except for rectal cancer, i.e. 5 × 5 Gy). For breast cancer patients that had already begun RT and patients for whom irradiation (either for breast cancer or palliative treatment) was about to be started (planning in progress or completed but treatment not started), the number of sessions was adapted, giving priority to hypofractionation (workflow “adapt-COVID”) [17]. For patients whose treatment was not yet planned and whose start could be postponed for a few months, a new workflow called “break-COVID” was created and used to: (1) evaluate and identify the patients with delayed interventions during the crisis (delayed CT-scans, delayed treatment starts); (2) ensure the qualitative follow-up of delayed cases; (3) ensure the qualitative and quantitative follow-up of prescription changes; (4) resume treatment starts when the crisis is over by pushing forward the cases that were ready to start. The supplementary data 1 summarizes the fractionation and delay adjustments. It should be noted that specialized procedures such as isocentric lateral decubitus irradiation and Deep Inspiration Breath Hold for breast cancers, and brachytherapy for prostate cancers were suspended.
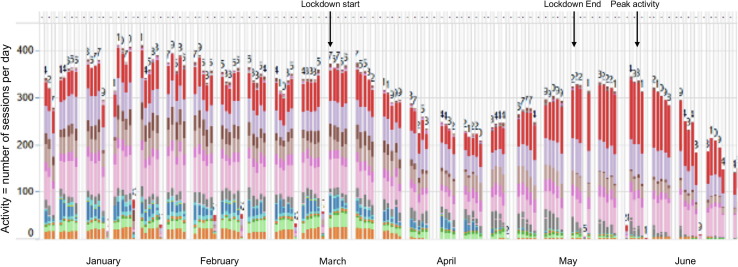
Similarly, the use of spirometry for respiratory gating in lung cancers was temporarily abandoned and replaced by 4D scanners in order to avoid handling high-risk components, such as breathing filters, to limit the risk of contamination as much as possible. Moreover, COVID+ patients were all treated on a dedicated machine, in prone position, using free-breathing VMAT technique and daily CBCT-based repositioning delivered on a Halcyon® (Varian®, PaloAlto, California). In this RT room, strict hygiene guidelines were established for all patients and operators. A dedicated circuit using a dedicated elevator and with arrows on the floor was set up in the RT department to avert contact between COVID+ and COVID− patients. We have used InSightive® software (Varian®) to provide a detailed analysis of all postponed treatments, and the projected evolution of the activity, i.e. the number of sessions per day in the RT department, during the periods before French lockdown, during lockdown, and following lockdown, respectively (Fig. 1 ).
Fig. 1.
Title: Projected evolution of the activity in the RT department from January to June 2020 (excluding stereotactic irradiation and brachytherapy). Caption: Location details: Red and purple: breast irradiation in dorsal decubitus position, dark brown: breast irradiation in isocentric lateral decubitus position, light brown: head and neck and brain, magenta: lung, pink: pelvis (including prostate).
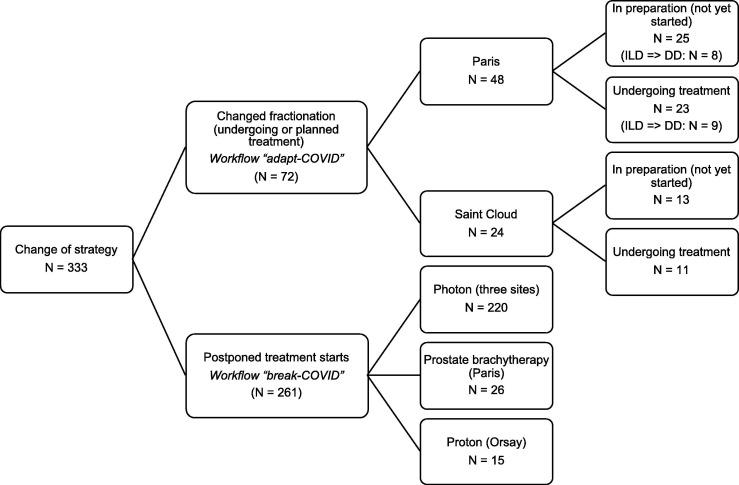
Therefore, the treatment strategy was changed for 333 patients (Fig. 2 ). The most affected locations were breast (N = 155) and prostate cancers (N = 66, including 26 permanent implants) (supplementary data 2). In order to optimally reschedule the 261 postponed treatments, priorities were established. The few patients with non-resected tumors (such as head and neck) who required confinement during the lockdown (e.g., severe COVID-19 infection) were reprogrammed to be first. The very few patients with postponed stereotactic irradiation were second. Then, in order: (1) hormone-receptor-negative breast cancer (and therefore with no treatment since surgery); (2) hormone-receptor-positive breast cancer (exceptionally treated with hormone therapy [HT] since surgery); (3) non-operated prostate cancer with no indication for HT; (4) operated prostate cancer with no indication for HT; (5) non-operated prostate cancer treated with HT; (6) and operated prostate cancer treated with HT. Patients with brain metastases not responding to corticosteroids and symptomatic patients remained a priority. Insightive® software provided a precise projection of the kinetics of postponed treatments, allowing us to anticipate a significant increase in the flow of patients requiring treatment in the department at the time of peak activity expected at the end of May and beginning of June 2020. Since May 11th 2020, we chose to prioritize shortening the delay to the start of RT for all patients treated post-lockdown while maintaining hypofractionated internationally validated schemes during the following months. The purpose of this 2-step procedure is to remain vigilant should there be consecutive waves of contamination.
Fig. 2.
Title: Flow-chart summarizing the management changes occurring during lockdown. Caption: ILD: isocentric lateral decubitus irradiation, DD: dorsal decubitus irradiation, ILD = > DD: Re-planning ILD treatment in DD.
Finally, we highlighted some of the key issues in anticipating the end of COVID-19 crisis in a high-volume department of RT in a French comprehensive cancer center, and analyzed the use of certain techniques that could be continued outside the epidemic context, such as hypofractionation, and obtaining real-time data monitoring using data visualization tools.
Conflict of interest statement
None to declare.
Funding statement
None to declare.
Footnotes
The Editors of the Journal, the Publisher and the European Society for Radiotherapy and Oncology (ESTRO) cannot take responsibility for the statements or opinions expressed by the authors of these articles. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. For more information see the editorial “Radiotherapy & Oncology during the COVID-19 pandemic”, Vol. 146, 2020.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.radonc.2020.05.043.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.You B, Ravaud A, Canivet A, Ganem G, Giraud P, Guimbaud R, et al. The official French guidelines to protect patients with cancer against SARS-CoV-2 infection. Lancet Oncol 2020;0. https://doi.org/10.1016/S1470-2045(20)30204-7. [DOI] [PMC free article] [PubMed]
- 2.Ferguson NM, Laydon D, Nedjati-Gilani G, Imai N, Ainslie K, Baguelin M, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID- 19 mortality and healthcare demand 2020:20. [DOI] [PMC free article] [PubMed]
- 3.Filippi A.R., Russi E., Magrini S.M., Corvò R. Covid-19 outbreak in northern Italy: first practical indications for radiotherapy departments. Int J Radiat Oncol. 2020 doi: 10.1016/j.ijrobp.2020.03.007. S0360301620309305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krengli M., Ferrara E., Mastroleo F., Brambilla M., Ricardi U. Running a Radiation Oncology Department at the time of coronavirus: an Italian experience. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.003. S2452109420300543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ngoi N., Lim J., Ow S., Jen W.Y., Lee M., Teo W. A segregated-team model to maintain cancer care during the COVID-19 outbreak at an academic center in Singapore. Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.03.306. S0923753420364103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Y.-L., Hsu F.-M., Tsai C.J., Chia-Hsien Cheng J. Efforts to reduce the impacts of COVID-19 outbreak on Radiation Oncology in Taiwan. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.005. S2452109420300567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Combs S.E., Belka C., Niyazi M., Corradini S., Pigorsch S., Wilkens J. First statement on preparation for the COVID-19 pandemic in large German Speaking University-based radiation oncology departments. Radiat Oncol. 2020;15:74. doi: 10.1186/s13014-020-01527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Achard V., Tsoutsou P., Zilli T. Radiotherapy in the time of the Coronavirus pandemic: when less is better. Int J Radiat Oncol. 2020: doi: 10.1016/j.ijrobp.2020.03.008. [DOI] [Google Scholar]
- 9.Coles C.E., Aristei C., Bliss J., Boersma L., Brunt A.M., Chatterjee S. International guidelines on radiation therapy for breast cancer during the COVID-19 pandemic. Clin Oncol. 2020;32:279–281. doi: 10.1016/j.clon.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guckenberger M., Belka C., Bezjak A., Bradley J., Daly M.E., DeRuysscher D. Practice recommendations for lung cancer radiotherapy during the COVID-19 pandemic: an ESTRO-ASTRO consensus statement. Radiother Oncol. 2020;146:223–229. doi: 10.1016/j.radonc.2020.04.001. S0167814020301821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curigliano G., Cardoso M.J., Poortmans P., Gentilini O., Pravettoni G., Mazzocco K. Recommendations for triage, prioritization and treatment of breast cancer patients during the COVID-19 pandemic. Breast. 2020 doi: 10.1016/j.breast.2020.04.006. S096097762030093X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simcock R., Thomas T.V., Estes C., Filippi A.R., Katz M.S., Pereira I.J. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68. doi: 10.1016/j.ctro.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marijnen C.A.M., Peters F.P., Rödel C., Bujko K., Haustermans K., Fokas E. International expert consensus statement regarding radiotherapy treatment options for rectal cancer during the COVID 19 pandemic. Radiother Oncol. 2020;148:213–215. doi: 10.1016/j.radonc.2020.03.039. S0167814020301730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yahalom J., Dabaja B.S., Ricardi U., Ng A., Mikhaeel N.G., Vogelius I.R. ILROG emergency guidelines for radiation therapy of hematological malignancies during the COVID-19 pandemic. Blood. 2020 doi: 10.1182/blood.2020006028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomson D.J., Palma D., Guckenberger M., Balermpas P., Beitler J.J., Blanchard P. Practice recommendations for risk-adapted head and neck cancer radiotherapy during the COVID-19 pandemic: an ASTRO-ESTRO consensus statement. Int J Radiat Oncol. 2020 doi: 10.1016/j.ijrobp.2020.04.016. S0360301620310348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zaorsky N.G., Yu J.B., McBride S.M., Dess R.T., Jackson W.C., Mahal B.A. Prostate cancer radiation therapy recommendations in response to COVID-19. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.010. S2452109420300610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loap P., Kirova Y., Takanen S., Créhange G., Fourquet A. Breast radiation therapy during COVID-19 outbreak: practical advice. Cancer Radiother J Soc Francaise Radiother Oncol. 2020 doi: 10.1016/j.canrad.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.