Abstract
Objectives
To develop a workflow algorithm for physicians and staff to decrease cross contamination and minimize exposure to Coronavirus Disease −19 (COVID-19) in pediatric otolaryngology at a community pediatric hospital.
Methods
PubMed and Google Scholar searches were carried out using the keywords. Pertinent clinical information related to pediatric otolaryngology was reviewed from journals, Texas Medical Board guidelines as well as institutional guidelines. Updated information from the Centers for Disease Control through social media was identified via Google search.
Study design
Safety measures and clinical work-flow protocols were developed to protect patients, families, and staff. Protocols included a rotation schedule for providers and ancillary staff, guidelines for in-clinic visits and alteration to surgical block and surgical case cadence to minimize exposure of providers and staff to COVID-19. Algorithms and guidelines were reviewed and revisions made at each phase of the pandemic related to in-clinic visits, telemedicine visits, and surgical cases.
Conclusion
In the era of the COVID-19 pandemic, otolaryngologists and pediatric otolaryngologists are amongst sub-specialties with an increased risk of exposure. It is imperative that a modification in clinical workflow is created to minimize the risk of exposure to providers and staff while continuing to provide care to patients.
Practice implications
The COVID-19 pandemic continues to evolve and change rapidly. The described guidelines and workflow algorithm serve as tools to help pediatric otolaryngologists protect themselves and their staff and patients during this global crisis.
Keywords: COVID-19, Otolaryngology, Physicians, Patient safety
1. Introduction/background
Coronavirus Disease-19 (COVID-19) is a novel disease impacting society with frequent treatment evolutions based on clinical experience. The Centers for Disease Control (CDC) has suggested person-person spread through direct close contact (within 6 feet). https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html. Recently, a paper published in the New England Journal of Medicine suggests that an aerosol form of transmission of the virus (SARS-CoV-2) causing COVID-19 is possible as the virus can remain viable and infectious in the aerosol form for several hours and on certain surfaces for days [1]. Otolaryngologists have been identified to be at increased risk of exposure to COVID-19 given the nature of our anatomical practice and aerosolized spread of the virus [2]. Pediatric otolaryngologists may be at an even greater risk when treating asymptomatic children who can be carriers of infection with high concentrations of the virus in the nasal and nasopharyngeal secretions [[3], [4], [5]].
Social distancing has been recommended by the CDC and various health agencies as one of the most important mitigation steps that can “flatten the curve” of disease burden of COVID-19 positive patients. https://www.politico.com/news/2020/04/01/jerome-adams-coronavirus-social-distancing-guidelines-158998. In the pediatric population, given the high rate of asymptomatic infection, it is imperative that providers follow strict safety guidelines [3,6]. Authors of a recent paper accepted by the Otolaryngology-Head and Neck Surgery propose that all asymptomatic children with unknown COVID-19 status should be presumed positive unless proven otherwise [7].
In the current paper, we outline our pediatric otolaryngology workflow algorithm that was formulated, approved and implemented in keeping with the above guidelines during the various phases of “evolution, peak and flattening” of the COVID-19 curve. The primary objective of the algorithm was to minimize exposure between staff and providers and between staff/providers and patients while continuing to care for patients.
2. Workflow algorithm/results (during COVID-19 peak and while stay-at-home orders and surgery restrictions were in place)
Based on heighten viral exposure concern and subsequent State mandate, we describe the organizational and clinical changes implemented to provide safer care to patients and limit exposure to staff and providers. We implemented a “rotation” protocol for providers and staff both for ambulatory and inpatient settings. We also made changes for evaluation of patients requiring emergent or urgent surgeries.
2.1. Organizational changes
-
1.
All patients and family members were screened (questionnaire, temperature screen) upon entering the hospital building.
-
2.
A second screening occurred when the patient checked in to the clinic.
-
3.
All visits when feasible were changed to telehealth (phone or video) visits.
-
4.
All community specialty care centers were closed. Any patient at these facilities deemed urgent were seen at one central location.
-
5.
All meetings, conferences, and urgent provider training sessions were altered to virtual meetings.
-
6.
Online training was available to learn and reinforce the correct way of wearing and discarding personal protective equipment (PPE).
-
7.
In compliance with state issued executive order, all non-essential, non-life-threatening surgeries were postponed until restrictions were lifted.
2.2. Clinical changes
-
a
Reorganization of Providers
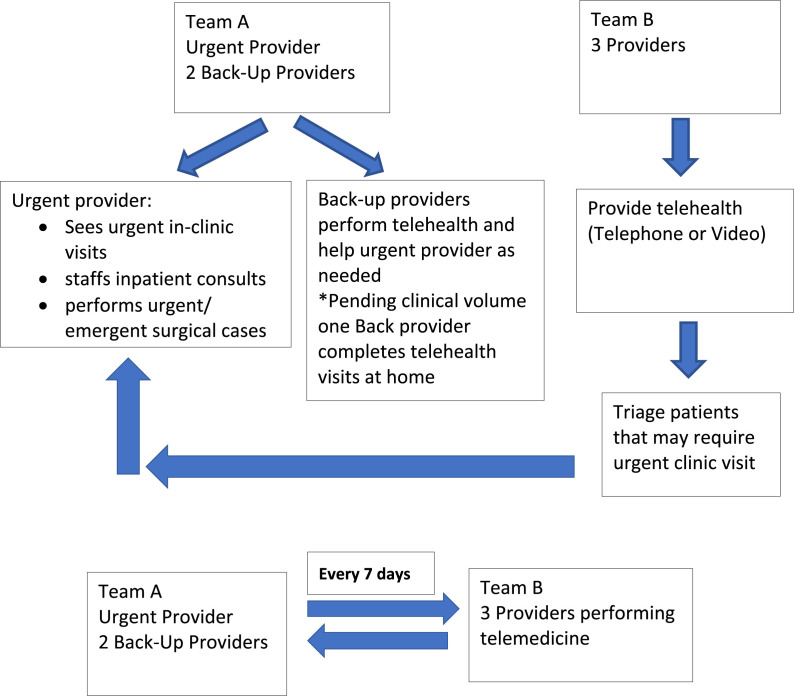
All the providers at the community hospitals were divided into two teams, Team A and Team B. Each team had 2-3 providers per team. Team A was designated as the “Urgent” team and Team B was the “Home” Team. Each team served a one-week rotation prior to altering roles.
Team A consisted of the following:
-
a
1 Urgent Provider: This provider was on call for an entire week. The responsibilities of this provider included evaluation of urgent/emergent patients both in outpatient and inpatient setting as well as performing any urgent/emergent surgeries.
-
b
1–2 Back-Up Providers: The urgent provider was supported by 1–2 back-up providers depending on clinical volume. The back-up providers had scheduled telehealth visits and were available to provide agssistance to the urgent care provider as needed. For instance, if the urgent care provider was in the Operating Room (OR) performing emergent/add on cases, the back-up provider saw urgent patients in the clinic so that patients in clinic were attended to in a timely fashion. To limit potential viral exposure, the majority of the time, the urgent provider was the primary physician performing direct patient care.
2.2.1. Team B
The Home team provided telehealth medicine to patients. This team was the ‘off site’ team for a period of one week. The providers on Team B, through their telehealth encounters identified patients that required an urgent clinical follow up visit. Urgent clinical visit examples included prolonged draining ear unresponsive to otic antibiotic drops, nasal/ear foreign bodies, auricular hematomas, Acute Otitis Media (AOM) unresponsive to intramuscular (IM) and oral antibiotic management and various abscesses. Any provider from Team B was able to add such a patient to Team A's urgent provider's schedule thereby ensuring that only the urgent provider was in direct patient contact.
Once the urgent provider completed his/her one-week rotation, this provider was not involved in direct patient care for a minimum period of a week. If the urgent provider became symptomatic or was exposed to a COVID-19 positive patient, this role was switched to one of the back-up providers from the same team. The urgent provider was quarantined for a period of 2 weeks followed by an additional two weeks of telemedicine, limiting direct patient care for 4 weeks.
The above workflow has been outlined in Fig. 1 .
-
bReorganization of Staff
-
1Registered Nurses (RN): Each week we designated a “clinical” RN who helped the urgent provider as needed. The remaining RN's assisted with phone triage and converting patient visits to telemedicine visits. The roles of the nurses also changed weekly similar to the providers.
-
2Medical Assistant (MA): Each week we designated a “clinical” MA that along with the assigned nurse helped the Urgent Provider as needed. The other MA's worked remotely to help with scheduling and consenting of telehealth visits. The MA's also rotated weekly.
-
1
Fig. 1.
Algorithm for physician rotation and responsibilities.
2.3. Surgery schedule changes
Per State executive order all elective surgeries were postponed during this period. Providers called scheduled patients and discussed alternative treatment options (when feasible) while awaiting restrictions to be lifted. Surgery schedulers maintained a surgical case cancellation list to aid with rescheduling procedures based on the initial surgery date and clinical patient concern. Urgent surgery was defined as a case that could be postponed until the patient was medically stable, but should generally be done within 2 days, and an emergency surgery was defined as one that must be performed without delay; the patient has no choice other than immediate surgery if permanent disability or death is to be avoided.
The Texas Medical Board (TMB) updated online guidance on the scheduling of elective surgeries and procedures during the COVID-19 disaster. These are shown in Table 1 . These guidelines were followed when scheduling urgent/emergent surgeries. Institutional policies and guidelines from American Academy of Otolaryngology-Head and Neck Surgery were also followed to make decision regarding urgent/emergent surgeries. In keeping with these guidelines, every urgent or emergent case (when feasible) was reviewed by the surgical lead team and Chief of Otolaryngology for authenticity and validity of “URGENT” nature of the surgery. To minimize exposure risk, only the urgent provider performed these surgeries. In addition, the following protocol was followed for COVID-19 testing for urgent/emergent cases.
-
1.
COVID-19 test was performed 2–3 days prior to all scheduled urgent surgical cases. The timing of the pre-op COVID-19 testing was governed by hospital policy. The rationale behind testing 2–3 days prior to scheduled surgery, was to provide adequate time for tests to be resulted and also decrease exposure risk to the virus between testing and surgery date.
-
2.
All emergent surgical cases, such as tonsil bleeds and airway foreign body, were tested for COVID-19 in the emergency department (ED) or OR without delaying timing of surgery.
-
3.
While performing any nasal, sinus and or throat related surgery, the provider and anesthesiologist along with the staff wore N95 mask with a face shield along with universal personal protective equipment (PPE).
-
4.
COVID-19 test was performed for all patients admitted to the intensive care unit (ICU)
Table 1.
Texas Medical Board Guidelines (TMB) to help Surgeons determine urgent/emergent surgical cases.
| TMB rules allow providers to use their judgment in determining whether a surgery or procedure will prevent serious adverse medical consequences or death |
| If you normally could or would wait a few weeks to provide the surgery or procedure being considered for a specific patient based on the patient's unique circumstances, then that might help you decide what to do |
| If you normally could not or would not wait a few weeks to provide the surgery or procedure being considered for a specific patient based on the patient's unique circumstances, then that might help you decide what to do |
| If you do proceed with a surgery or procedure during this time, then be sure to clearly document why you made that decision |
| Referencing legitimate literature and guidelines, such as the CDC, CMS, or specialty guidelines will be very helpful; |
2.4. Reorganization of clinical work-flow
Our pre-COVID-19 clinical space included 6 exam rooms and 3 procedure rooms separated by two hallways. To increase safety, social distancing and prevent cross contamination we designated one area as the “urgent” clinical area and assigned one exam room and one procedure room for the urgent provider to see patients and perform clinical procedures. The “urgent” space was separated from the other clinic rooms by a clean hallway. The “clean area” was used to perform telehealth visits with appropriate social distancing. To help work through unforeseen factors we implemented daily huddles and weekly virtual meetings to obtain feedback and make adjustments as needed.
3. Workflow algorithm/results (during plateau phase of COVID-19 and easing of surgery restrictions and stay-at-home orders)
3.1. Organizational changes
Patients and caregivers were screened similar to that outlined in 1a above.
Providers were screened using infrared thermal scanner to provide contact-less screening.
Patients and families were provided masks upon entering the hospital and it was mandated that they wear these masks at all times within the hospital.
Only one caretaker was permitted to enter the hospital with the patient. The caretaker was also screened for symptoms.
All families, patients, and hospital staff were expected to adhere to social distancing. Only 4 people were allowed in the elevators at any given time, A hospital employee was assigned to aid with elevator traffic.
The entire hospital (including inpatient, outpatient, and surgical areas) had visual signs and posters at various locations reminding patients and families to wear masks, wash hands and maintain social distancing.
The community ambulatory centers re-opened slowly. The initiative was to see those patients in clinic that could not have been treated through telemedicine visits. For instance: ear pain, ear or nasal foreign bodies, persistent ear drainage, and tongue-tied infants with difficulty feeding.
3.2. Clinical changes
Providers continued with team A and B rotation during this time.
When a provider from Team A was on call, the back-up provider was assigned half a day to see patients in clinic. The back-up provider continued to perform telemedicine visits on the other days. During this “slow ramp” up phase, limited clinical templates were opened to provide in-clinic patient care. The strategic “slow ramp up” clincial phase continued to provide quality and safety measures to limit exposure including: clinical template modification (decreasing the amount of patients per clinical session), alteration of clinical flow of patients to limit potential exposure and reinforce social distancing, provider and staff training during transition of telemedicine technology, and changing OR workflow to include COVID-19 testing for all surgical patients.
After a physician performed an aerosol generating procedure (AGP) such as flexible laryngoscopy or deep nasal suctioning, to limit staff exposure, the provider placed the laryngoscope in a biohazard bag. The procedure room was then closed, a sign was put outside the door to indicate that the room was closed due to use for an AGP and the timer on the door set for 1 h. After 1 h, the staff entered the room for disinfection of the room and to carry the scope back to sterile processing while wearing appropriate PPE.
Telemedicine technology was upgraded to allow for a larger number of patients to be on a protected server at any given time. These visits were also integrated with the patient's electronic medical records which made the telemedicine process easier and faster for patients and providers.
Provider schedules were reviewed daily by the staff to ensure that a patient was correctly scheduled either for a telemedicine or an in-clinic visit with the appropriate provider.
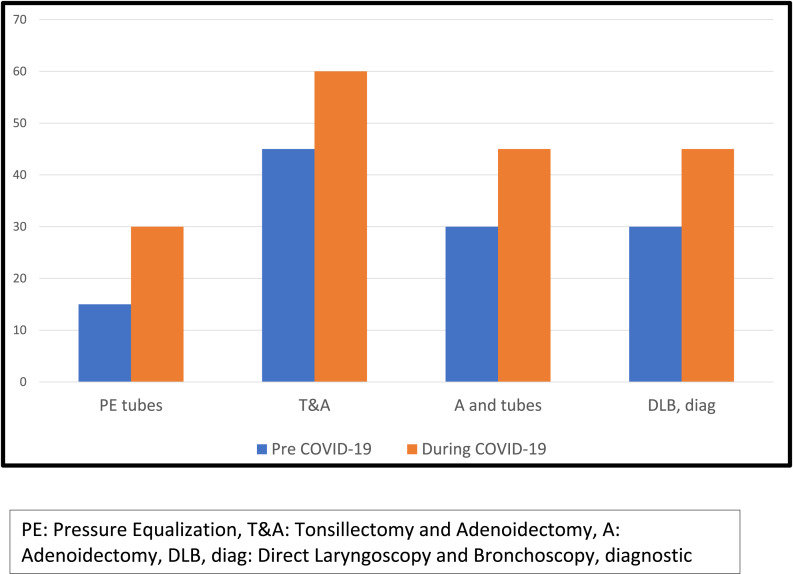
3.3. Surgical schedule changes
Upon alteration of state mandate lifting surgery restrictions for elective procedures new patient safety measures were implemented. All patients continued to be tested for COVID-19 prior to surgery. In addition, hospital policy was altered to allow only one caretaker to be present for the procedure. Upon entering the hospital surgical patients also went through the screening process and asked to wear a mask. Patients were restricted to preoperative rooms and not allowed in the common play area. The OR template was changed to optimize OR utilization and also accommodate social distancing guidelines specifically for the check-in and waiting areas. Social distancing was optimized by increasing the turn-over time between procedures. Fig. 2 compares surgical turnover times prior COVID-19 to those during COVID-19.
Fig. 2.
Comparison of turnover times between surgeries before and during COVID-19
PE: Pressure Equalization, T&A: Tonsillectomy and Adenoidectomy, A: Adenoidectomy, DLB, diag: Direct Laryngoscopy and Bronchoscopy, diagnostic.
Initial priority was given to the patients in which surgery was postponed during the COVID-19 surgical restriction. Providers called their patients to determine patient's interest in pursuing elective surgeries and answer their queries. As patients were contacted it was noted some were still hesitant with rescheduling surgery and elected to be contacted at a future time.
4. Workflow algorithm/results (current and future)
4.1. Organizational changes
Patients, families, providers and staff continue to be screened. There is ongoing limitation on the number of caregivers that can be physically present with the patient at any given time (restricted to one adult caretaker >18).
Plexiglass frames have been installed at outpatient and surgical check-in and check-out locations to provide additional barrier between staff and patients/families.
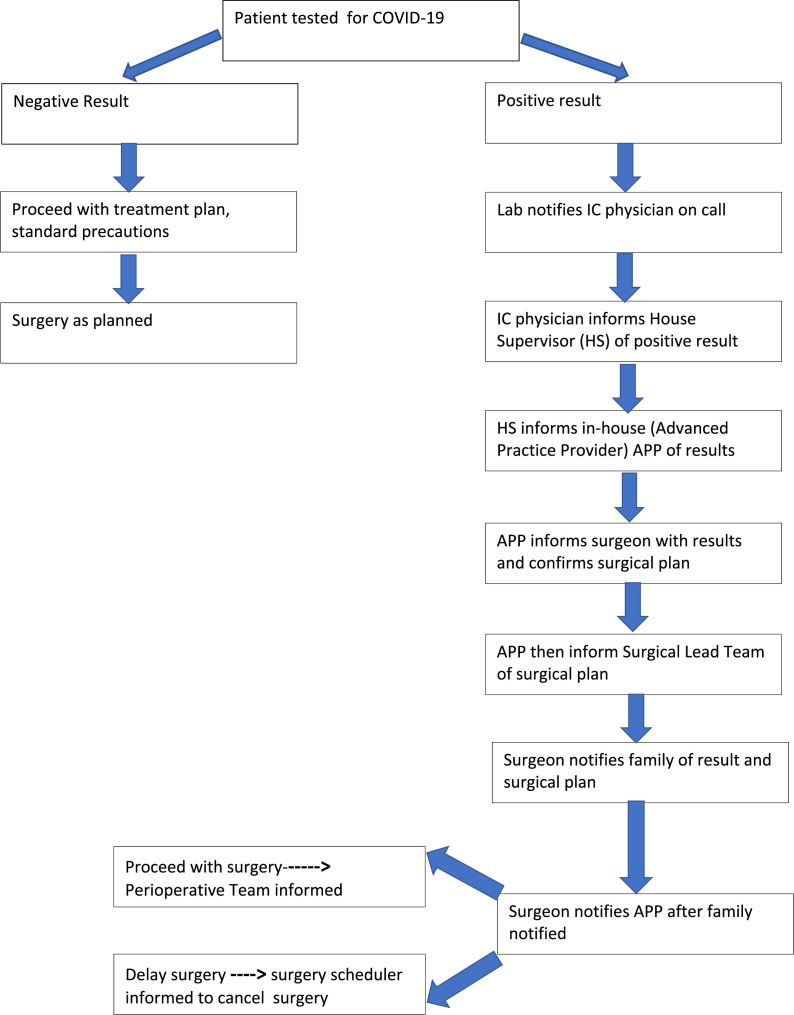
A new drive-through initiative for COVID-19 testing was implemented for family convenience. Parental feedback regarding this initiative has been positive and drive through testing has helped our community hospital to increase the number of tests performed on a daily basis. As testing has increased, we have found more asymptomatic patients testing positive for COVID-19, though overall positive rate has been in the range of 2.1–2.4%. A new algorithm is in place to manage asymptomatic patients that test positive for COVID-19 prior to surgery (Fig. 3 ). If a patient tests positive for COVID-19 unless the surgeon deems the procedure urgent/emergent, the procedure will be delayed and retesting will occur to ensure the patient is negative before undergoing surgical procedure and other procedures including non-emergent radiographic testing or polysomnography (PSG).
Fig. 3.
Covid-19 positive results notification process-Surgery.
The institution has advanced COVID-19 testing capabilities by implementing rapid COVID-19 testing (results available ≤4 h). Due to current limitation of number of rapid testing kits available, guidelines were developed to identify indications for rapid testing. Current indications include emergent procedures (such as stable airway foreign bodies), add on cases such as abscess drainage, and for out of state patients requiring surgery at our hospital.
The specialty surgery centers continue to increase the number of sessions for each provider. The plan is to have at least one ENT provider in each of the satellite clinics daily.
Clinical ramp up has also influenced by other services including audiology and the sleep lab. Secondary to social distancing concerns, audiology schedules were opened at a slower pace initially accommodating ENT add on patients, hearing aid patients, and acute hearing loss patients. Audiology ramp up will include slowly increasing the number of regular scheduled appointments.
The sleep lab also initially postponed all elective PSG's. As restrictions were lifted all patients being scheduled for a PSG also required COVID-19 testing prior to the study. In attempt to decrease repeat patient testing, when feasible COVID-19 testing, PSG and potential surgical intervention (contingent on study results), were coordinated within a 3-day period of time.
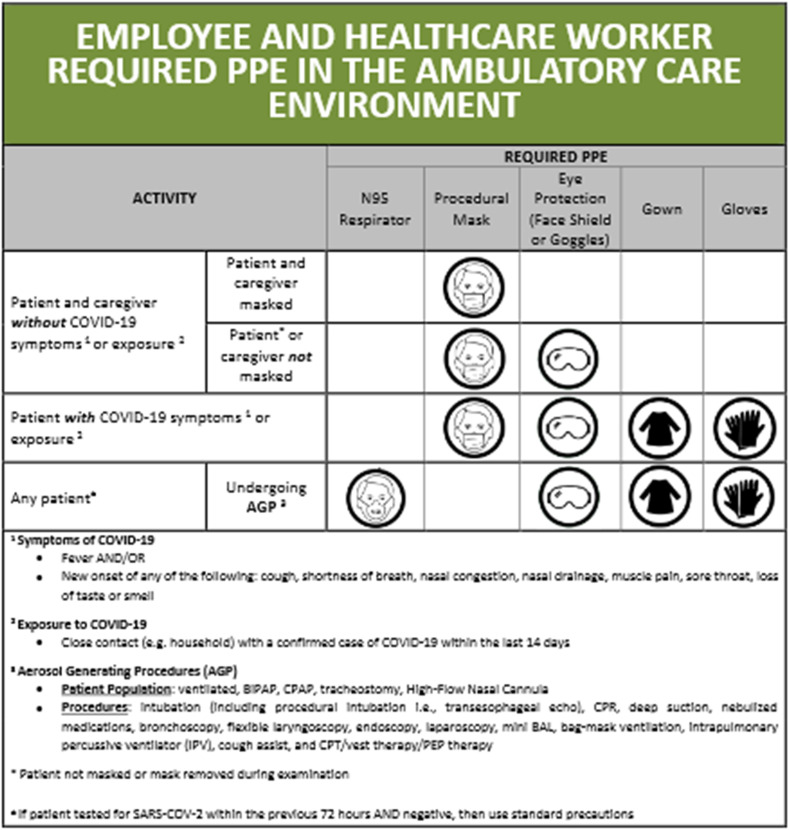
4.2. Clinical changes
Social distancing guidelines continue to be followed. PPE guidelines (Fig. 4 ) remain in place.
Fig. 4.
Personal Protective Equipment (PPE) guidelines currently in place.
To allow a conservative clinical ramp up period, overall primary institutional initiative was to maintain 50% of patient visits as telemedicine visits. Three main phases of clinical ramp up were developed to alter pre-COVID-19 clinical volume to aid with social distancing. The developed phases allowed progression from only seeing urgent patients in clinic to increasing routine clinical sessions. The goal is to ramp up clinical sessions to have at least 2 providers in clinic daily (pre COVID-19 era, there were 3 providers daily) and to also incorporate limited clinical sessions for Advanced Practice Provider (APP's).
5. Surgical schedule changes
OR blocked time has now been diverted back to pre-COVID-19 state. There is an institution wide effort to utilize OR time optimally and an email is sent out weekly for any “first come first serve” time that is available. The OR cadence remains similar to that outlined in Fig. 3 (during COVID-19) to help everyone follow social distancing and to ensure that the post-operative care unit (PACU) is not overwhelmed while recovering patients. Testing for COVID-19 prior to surgery and PPE guidelines remain in place.
6. Conclusion
We describe a workflow algorithm implemented at a community pediatric hospital setting during the various phases of the COVID-19 pandemic to prevent cross contamination of provider/staff while providing safe patient care. This pandemic has been unprecedented and has impacted different geographic areas in a diverse manner. As these geographic areas transition through the different phases of COVID-19, our algorithm may serve as a tool to help other institutions implement safe and effective workflow changes at each transitional phase. Patient and provider/staff safety should remain central in all decision makings.
Contributor Information
Shraddha Siddharth Mukerji, Email: sxmukerj@texaschildrens.org.
Yi-Chun (Carol) Liu, Email: yxliu2@texaschildrens.org.
Mary Frances Musso, Email: mxmusso@texaschildrens.org.
References
- 1.Van Doremalen N., Lloyd-Smith J.O., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, Mar 13 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vukkadala N., Qian Z.J., Holsinger F.C., Patel Z.M., Rosenthal E. COVID-19 and the otolaryngologist - preliminary evidence-based review. Laryngoscope. 2020 Mar 26 doi: 10.1002/lary.28672. [DOI] [PubMed] [Google Scholar]
- 3.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., Tong S. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 Mar 16 [Google Scholar]
- 4.Chan J.Y.K., Wong E.W.Y., Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemic: an experience in Hong Kong. JAMA Otolaryngol. Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0488. [DOI] [PubMed] [Google Scholar]
- 5.Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qiu H., Wu J., Hong L., Luo Y., Song Q., Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30198-5. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bann D.V., Patel V.A., Saadi R.A. Best practice recommendations for pediatric otolaryngology during the COVID-19 pandemic. Otolaryngol. Head Neck Surg. 2020 doi: 10.1177/0194599820921393. [DOI] [PubMed] [Google Scholar]