Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has had a tremendous impact on the healthcare system. Owing to restrictions in elective surgery and social distancing guidelines, the training curriculum for neurosurgical trainees has been rapidly evolving. This evolution could have significant long-term effects on the training of neurosurgery residents. The objective of the present study was to assess the effects of COVID-19 on neurosurgical training programs and residents.
Methods
A survey consisting of 31 questions assessing changes to resident clinical and educational workload and their sentiment regarding how these changes might affect their careers was distributed electronically to neurosurgery residents in the United States and Canada.
Results
The survey respondents were from 29 states and Canada and were relatively evenly spread across all levels of residency. Nearly 82% reported that the inpatient and outpatient volumes had been either greatly (44.0%) or moderately (37.8%) reduced. Greater than 91% reported that their work responsibilities or access to the hospital had been reduced, with a significant reduction in work hours and a significant increase in resident didactics (P < 0.001). Senior residents expressed concern about their educational experience and their future career prospects as a result of the pandemic.
Conclusion
Universally, residents have experienced reduced work hours and a reduction in their operative case volumes. Programs have adapted by increasing didactic time and using electronic platforms. It is quite possible that this remarkable period will prompt a critical reappraisal of the pre–COVID-19 adequacy of educational content in our training programs and that the enhanced educational efforts driven by this pandemic could be lasting.
Key words: COVID-19, Education, Neurosurgery, Pandemic, Residency, Survey
Abbreviations and Acronyms: CNS, Congress of Neurological Surgeons; COVID-19, Coronavirus disease 2019
Introduction
In late December 2019, severe acute respiratory syndrome coronavirus 2 was initially detected in Wuhan, China, in a cluster of patients with pneumonia of an unknown source.1 The virus subsequently spread rapidly, placing significant strain on the healthcare system globally, with ripple effects that have reached nearly all aspects of life.2 The first case of coronavirus disease 2019 (COVID-19) in the United States was confirmed on January 20, 2020. On March 13, 2020, the American College of Surgeons recommended the cessation of elective surgery and triaging of the remaining cases according to the level of acuity.3, 4, 5 To help reduce the burden on the healthcare system during this pandemic, neurosurgery departments throughout the United States and Canada have reduced the number of elective surgeries, made changes to faculty and resident schedules, changed the structure of their inpatient and outpatient services, and reduced the number of larger group meetings.6, 7, 8, 9, 10 Although necessary, these changes could have had significant effects on the training of neurosurgery residents.
To better assess the effects of COVID-19 on neurosurgical training programs, we conducted a survey of all neurosurgical residents to determine how elements of their professional and personal lives have been affected during this pandemic. In the present report, we have demonstrated how the current phase of the COVID-19 pandemic has altered neurosurgical training.
Methods
Survey
The survey (Supplementary Appendix 1) was created using Qualtrics (Provo, Utah, USA). It was distributed electronically to program directors and coordinators in Accreditation Council for Graduate Medical Education–accredited and Royal College of Physicians and Surgeons of Canada–accredited neurosurgery residency programs across the United States and Canada. The survey included 31 questions, which were designed and vetted by us. Because of the rapid progression of the pandemic, the survey was not validated before distribution. The questions pertained to resident demographic data, year of training, location of training program, clinical volume and didactic changes during the pandemic, sentiments regarding the changes implemented, and how these changes have affected resident training and future career plans. The questions were designed to obtain the respondents’ general experience and reactions toward the pandemic. The responses were collected anonymously via the Qualtrics interface. Of an estimated 1300 active residents, 197 resident responses were collected from April 17, 2020 to April 30, 2020, for a response rate of 15%.11
Statistical Analysis
Statistical analysis was performed using SAS, version 9.4 (SAS Institute, Cary, North Carolina, USA). The categorical survey questions were summarized using counts and proportions. Continuous variables, such as training year and number of work hours per week, were grouped into categories for analysis. Highly affected states were defined as states with >10,000 cases of COVID-19. Less affected states were defined as those with ≤10,000 cases, as reported by the U.S. Centers for Disease Control and Prevention on May 2, 2020.12 Junior residents were defined as those in postgraduate years 1–4 and senior residents as those in postgraduate years 5–7. A χ2 test was used to compare the training year among the survey responders and to compare the responses between the junior and senior residents. The McNemar test was used to compare the number of hours per week that residents had worked before and after the start of the pandemic and the number of hours per week that didactic lectures were offered at the programs before and after the pandemic. For all tests, significance was set at a P < 0.05.
Results
Work Hours and Case Volume
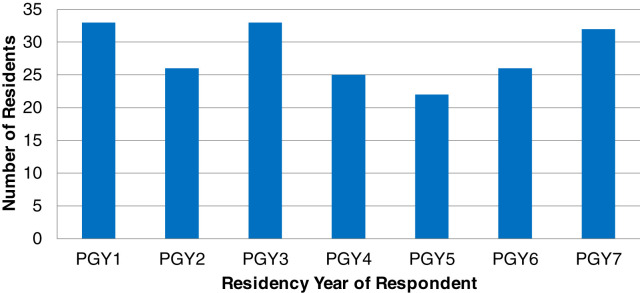
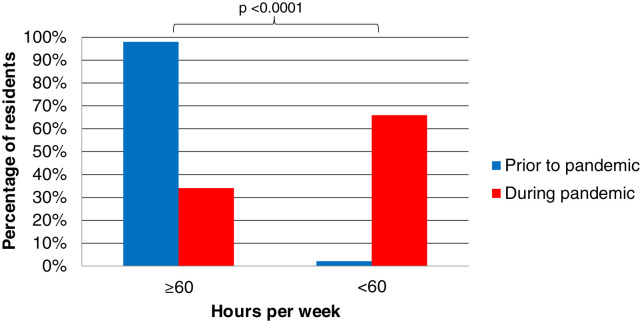
The survey respondents were from 29 states and Canada and were evenly spread across all residency levels (P = 0.619; Figure 1 ). Of the residents, 99% reported institutional limits on elective cases, with 99.5% reporting that the volume of operations performed at their institution had decreased. Nearly 82% reported that the inpatient and outpatient volumes had been either greatly (44.0%) or moderately (37.8%) reduced. More than 91% reported that their work responsibilities or access to the hospital had been reduced. Before the COVID-19 pandemic, 97.9% of the residents reported working at the hospital >60 hours per week. In contrast, during the pandemic, only 34% reported working >60 hours per week and 44.8% reported working <50 hours per week. The difference in the number of work hours was statistically significant (P < 0.0001; Figure 2 ).
Figure 1.
Graph showing the number of survey respondents stratified by residency year. The respondents were equally distributed across the residency years (P = 0.619). PGY, postgraduate year.
Figure 2.
Graph showing the resident work hours per week before and after the pandemic. Before the pandemic, 97.9% of residents were working >60 hours per week. During the pandemic, once elective cases had been stopped and distancing measures had been implemented, 66% were working <60 hours per week, a statistically significant difference (P < 0.0001).
Didactic Teaching and Research Activity
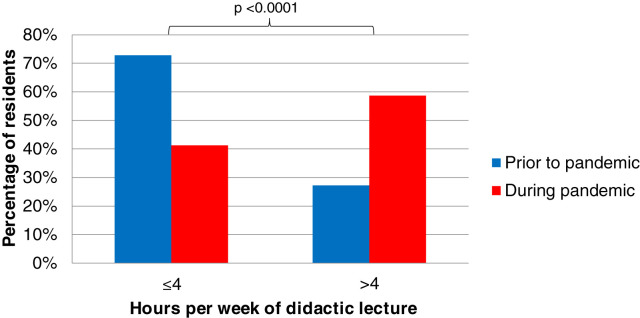
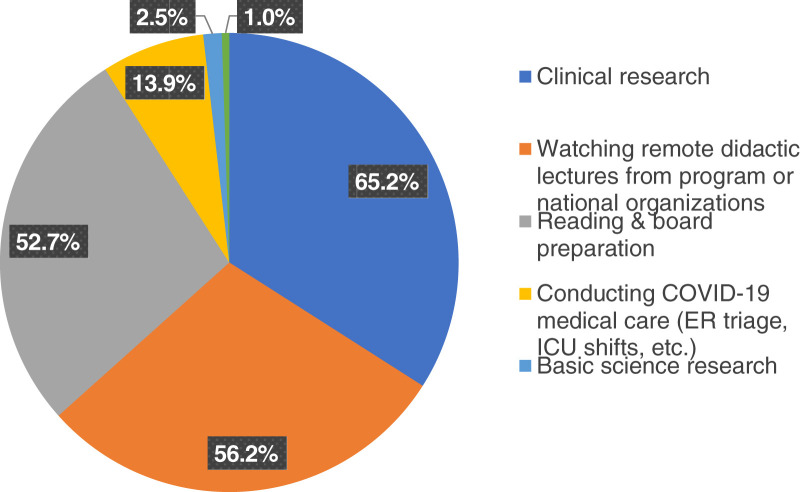
Many residency programs pivoted quickly to provide augmented didactic teaching to supplement the decline in hands-on training. Before the pandemic, only 27.2% of the residents responding to the survey reported spending >4 hours per week in formal didactic lectures through their program. This had increased significantly to 58.6% of residents spending >4 hours per week on didactics during the pandemic (P < 0.0001), with 19.4% spending >10 hours per week in didactic lectures of various forms (Figure 3 ). Nearly all residents surveyed (98.5%) reported that their program had converted to electronic platforms for their didactic lectures, with 71.9% of the programs making this change within 1 week of hospital restrictions taking effect. Most residents (79%) had been encouraged by their program to view the various complementary online didactic lectures that had begun to be offered during this time (e.g., Congress of Neurological Surgeons [CNS] Online Grand Rounds, CNS Virtual Visiting Professor, American Association of Neurologic Surgeons webinars, ad hoc national and international virtual conferences), with most (69.7%) viewing these an organized, monitored fashion. Most of the residents surveyed (64.6%) had a favorable response to the move to virtual didactics and only 10.8% reported negative responses. Furthermore, nearly one half of the respondents noted an increase in faculty engagement with resident education. The residents reported converting most of their time outside of neurosurgery clinical responsibilities into watching remote didactic lectures, conducting research, and preparing for board examinations. Also, nearly 14% of trainees reported spending at least a portion of that time providing COVID-19 medical care (Figure 4 ).
Figure 3.
Graph showing the weekly resident didactic lecture time before and after the pandemic. Before the pandemic, 72.8% of residents spent ≤4 hours per week in didactic lectures offered by their programs. During the pandemic, after the decline in elective cases and implementation of distancing measures, more than one half of the residents (58.7%) reported spending >4 hours per week in didactic lectures offered by their programs, a statistically significant difference (P < 0.0001).
Figure 4.
Pie chart showing where residents have been spending increased time during the coronavirus disease 2019 pandemic. These were not mutually exclusive categories (e.g., a respondent could have selected having spent increased time conducting clinical research and watching remote didactic lectures and spending time in the anatomy laboratory).
Direct Involvement in COVID-19 Medical Care
Approximately three fourths of residents reported being engaged by their program in formulating COVID-19 response plans and just more than one third of the respondents (35.1%) had been asked to provide non–neurosurgical care to patients with COVID-19. Residents in highly affected states were more likely than residents from less affected states to be asked to assist in the medical care of patients with COVID-19 (40.2% vs. 20.3%, respectively; P = 0.008). Overall, most residents (nearly 70%) reported they would be comfortable providing critical care or medical services to patients with COVID-19, with 57.9% having received extra training in this regard. Approximately 17% of respondents reported that their program had been negatively affected by their need to self-quarantine—or by a coresident needing to do so—after being exposed to or contracting COVID-19.
Overall Effect on Resident Sentiment
Most respondents (68.2%) reported that working as a physician during the pandemic had not had negative effects on their home or family lives, although 31.6% reported that it had negatively affected their interpersonal relationships (Table 1 ). Although 55.4% of trainees had had to alter vacation or elective schedules because of the COVID-19 outbreak, 88.7% responded that they did not believe they had been unfairly burdened by alterations to their work schedule or responsibilities. Roughly one third (33.7%) of the respondents were concerned that the epidemic would negatively affect their overall residency education and another one third (32.7%) were convinced that the course of their education would be unaltered. The remaining one third (33.7%) were unsure of the long-term effects the epidemic would have on their education. However, when categorized by residency status, the senior residents were more likely than were the junior residents to report that their cumulative residency experience had been negatively influenced by the pandemic (43.8% vs. 26.7%, respectively; P = 0.028). Only 8.2% of the residents were concerned that the restrictions resulting from the COVID-19 pandemic would limit their overall case numbers required by the Accreditation Council for Graduate Medical Education. However, 26.5% were concerned that these would limit their ability to obtain the employment or fellowship of their choice. Senior residents reported that the pandemic might (22.5%) or definitely (18.8%) would affect their chances of obtaining a fellowship or position of their choice. Among the junior residents, 15.5% reported that it might and 0.9% that it definitely would affect their future opportunities. This difference was statistically significant (P < 0.001). Overall, 74% of residents were unchanged in their perception of neurosurgery as a career, 13.8% were more favorable about their career, and 12.3% were less favorable. Although the difference was not statistically significant, a trend was found for residents from highly affected states having a more favorable perception of a career in medicine compared with those from less affected states (18.1% vs. 5.1%, respectively; P = 0.058).
Table 1.
Resident Sentiment Surrounding the Pandemic
| Survey Question | Resident Level∗ |
Parametric P Value† | |
|---|---|---|---|
| Junior (n = 117) | Senior (n = 80) | ||
| Q25. Do you feel that working as a physician during the COVID pandemic has negatively impacted your interpersonal relationships with family and friends? | 0.142 | ||
| Yes | 32 (27.59) | 30 (37.5) | |
| No | 84 (72.41) | 50 (62.5) | |
| Q26. Do you feel you have unfairly been required to continue or adapt your clinical duties in the face of the pandemic? | 0.639 | ||
| Yes | 12 (10.34) | 10 (12.5) | |
| No | 104 (89.66) | 70 (87.5) | |
| Q28. I feel that the COVID pandemic will negatively impact the cumulative experience of my residency training. | 0.028 | ||
| True | 31 (26.72) | 35 (43.75) | |
| False | 39 (33.62) | 25 (31.25) | |
| Unsure | 46 (39.66) | 20 (25) | |
| Q29. I am concerned that I will not meet the required ACGME case numbers by the end of my training due to the restrictions during the COVID pandemic. | 0.190 | ||
| True | 7 (6.03) | 9 (11.25) | |
| False | 109 (93.97) | 71 (88.75) | |
| Q30. Do you feel that the COVID pandemic will ultimately affect your chances of getting the fellowship/job of your choice? | <0.001 | ||
| Yes | 1 (0.86) | 15 (18.75) | |
| No | 97 (83.62) | 47 (58.75) | |
| Maybe | 18 (15.52) | 18 (22.5) | |
| Q31. How is your overall perception of a career in medicine impacted by the COVID pandemic? | 0.106 | ||
| More favorable | 19 (16.38) | 8 (10) | |
| Less favorable | 10 (8.62) | 14 (17.5) | |
| Unchanged | 87 (75) | 58 (72.5) | |
Data presented as n (%).
Q, question; COVID, coronavirus disease 2019; ACGME, Accreditation Council for Graduate Medical Education.
Junior resident level included postgraduate years 1–4; senior resident level included postgradudate years 5–7.
Calculated using the χ2 test.
Discussion
The COVID-19 pandemic has resulted in many challenges unparalleled in modern society. Hospitals have placed restrictions on elective cases, clinic visits, visitors, and time spent in the institution and, in many cases, have asked faculty and trainees alike to provide care in areas that are not their primary specialty. It only stands to reason that limited personal contact could affect our educational system, including medical education, with more downstream consequences than in other areas. The effects on the surgical and nonsurgical education and psyche of trainees is unknown. Specialties throughout medicine, especially surgical specialties, have needed to develop innovative solutions to continue the education of their trainees during the pandemic.13 Numerous individual studies and reports have described departmental and resident experiences and sentiment from throughout the medical community during this pandemic.7, 8, 9 , 14 , 15 Several recent media articles have been reported detailing residents’ responses to the pandemic.16 , 17 These accounts have largely detailed the negative effects that the pandemic has had on resident education and home life, suggesting that trainees have been unjustly required to bear much of the risk in caring for patients with COVID-19, with little reward. Through our survey, we sought to elucidate the true effects of the COVID-19 pandemic on neurosurgical residency education and the residents themselves. We found that the effects were experienced universally by nearly all neurosurgical trainees. Despite the significant reductions in operative cases and work hours, residency programs swiftly and nearly universally transitioned educational activities to electronic platforms, which have been favorably adopted by most residents. The significant increase in didactic lectures and opportunities has been a momentous effort by many programs and national organizations and is consistent with reports from individual programs about the changes made to didactics during the pandemic.9 , 10 , 13 , 14 This increase likely will supplement resident training and mitigate some of the loss that has occurred from the complete cessation of clinical activity.
These increases in didactic lectures have by and large been accomplished through remote platforms offered either locally by the individual institutions or nationally by both individual institutions and national organizations (i.e., virtual visiting professor, grand rounds). The response to these opportunities has been largely favorable among the neurosurgical trainees, with 64.6% of the respondents to our survey reporting a favorable opinion. Most residents were unsure whether their programs were planning to continue using virtual platforms after the pandemic. However, their continuation is certainly an area of consideration for the training curriculum. The effort put forth by organized neurosurgery and individual programs has been immense, with many programs converting to remote electronic didactic lectures within 1 week of the implementation of the reductions in surgical volume and social distancing measures. These efforts have resulted in didactic opportunities that otherwise would not have been available to trainees and has enriched the learning environments for neurosurgical education as a whole. In our experience, this has also fostered collaboration between geographically separated programs and has allowed our residents to broaden their horizons with experts in the field without ever having to leave their home. This could provide a model for the future of neurosurgical education and should definitely serve as a model for similar crises in the future.
The sentiment of those residents who responded to the survey toward the pandemic appears to be one of an eagerness and willingness to help. Our survey found that ~75% of trainees had been involved in helping to formulate a plan for their involvement in the care of patients with COVID-19 and that nearly 60% had received extra training should such a need arise. Although they were prepared, most neurosurgery residents (64.9%) had not been approached about providing non–neurosurgical care to patients with COVID-19. Training programs have performed excellently in preparing their residents for these circumstances. Several of the other reported accounts of residents’ reaction to COVID-19 have expressed some frustration that residents were bearing the burden of care and had been forced to compromise their education.16 , 17 However, in our survey, 88.7% of residents did not believe that the changes to their work or academic schedule or changes to their work responsibilities were unfair. Also, 87.6% of the respondents had reported that their perception of their career in medicine was either unchanged or had actually improved during the COVID-19 pandemic. Senior residents were 15 times more likely to express concern about their educational experience and their future career prospects as a result of the pandemic (Table 1). This finding suggests that senior residents might be experiencing the effects of the decreased operating time and reduced ability for in-person interviews more than their junior counterparts. This might require more acute attention from faculty with respect to preparing our senior residents for moving on to their fellowship or ultimate employment.
Although our results represent the views of a cohort of U.S. neurosurgical residents who were broadly representative in both geographic location and level of experience, the present study had a number of limitations. As with any survey, the opportunity existed for a response bias. Our selected population was not random, and it is quite possible that the residents most affected by the pandemic had not responded because of their increased responsibilities working on the front lines caring for patients with COVID-19. The overall sample size was relatively small, given that an estimated 1300 neurosurgical residents are currently in training in the United States and Canada.11 We acknowledge this as a shortcoming of our study. Given the demands resulting from the COVID-19 pandemic and additional burden of coordination efforts, we acknowledge that survey participation was not likely to be one of many priorities on the list of a program director or resident, which likely contributed to the low response rate of 15%, limiting the generalizability of the results. Also, with the rapid progression of the pandemic, we did not have the opportunity to validate the survey as a psychometric analysis tool. Therefore, the results should be interpreted as more descriptive findings.
We were pleased to find that our own department’s experience was similar to that of other North American programs. This has, by and large, been a positive adaptation. Although emergent and urgent cases have continued, elective cases were halted at our institution in early April. We pivoted within days of this case hold to a daily virtual 2-hour didactic schedule that included a departmental journal club, webinars from the CNS, attending and resident subspecialty didactics, facilitated use of surgical videos, attending-driven mock oral board cases, ad hoc national virtual conferences (e.g., multi-institutional Virtual Global Spine Conference), and kept our standard weekly grand rounds and monthly morbidity and mortality conferences. Furthermore, many faculty have met virtually with residents and fellows to discuss ongoing and newly developed research projects and initiatives. In our discussions with residents, regardless of level, the additional didactics have been received only positively, and we plan to layer in several elements of this curriculum to our weekly schedule even as elective cases resume. Furthermore, our residents have not openly expressed concern for their clinical training or future careers during the pandemic. We hope this is a reflection of the enhanced clinical didactic and academic training introduced to offset some the inevitable loss of training time in the operating room. It is likely that a number of novel educational changes will result from this pandemic. Electronic learning, which had not been broadly deployed in neurosurgical education before the pandemic, can expand the reach of our educational efforts in both space and time.18 Residents on other services outside the hospital or on vacation would still be able to participate in educational activities or even watch these again on their own time via recordings. This unique situation has led many programs to explore the greater use of video and virtual reality in resident training, which will provide yet another opportunity for learning outside of the operating room. The effort to train neurosurgical residents in critical care remains strong, with most of our respondents reporting that they were comfortable providing critical care and medical services to patients with COVID-19 if required.
Conclusion
The educational effects resulting from the COVID-19 pandemic have been nearly universally experienced across neurosurgical residency programs. Nearly all residents have experienced reduced work hours and reductions in their operative case volumes. Programs have been effective, however, in increasing didactic time through use of electronic platforms, which have been favorably received by residents. Ultimately, the respondents to our survey did not report that they were unfairly bearing the burden of care for patients with COVID-19 or neurosurgical patients on their services. Most were not concerned that the changes would have long-term negative effects on their overall education or future career prospects. Undoubtedly, some of the changes that programs have made because of COVID-19 will be useful adjuncts that will continue into the future. Although we do not know how long the changes brought about by COVID-19 will last, it is encouraging that neurosurgery has been able to quickly adapt educational programs to fit the needs of our resident trainees. Future efforts will undoubtedly work to quantify both the educational effects of the virus and the success our interventions have had in mitigating these effects.
CRediT authorship contribution statement
Panayiotis E. Pelargos: Investigation, Data curation, Writing - original draft. Arpan Chakraborty: Writing - original draft. Yan D. Zhao: Validation, Formal analysis, Visualization. Zachary A. Smith: Writing - original draft. Ian F. Dunn: Writing - review & editing. Andrew M. Bauer: Conceptualization, Methodology, Investigation, Data curation, Writing - original draft.
Acknowledgments
The authors acknowledge Camille K. Milton, BS, for her assistance during the present study. Also, the authors appreciate and acknowledge the willing participation of the survey respondents nationally in this difficult time.
Footnotes
Conflict of interest statement: The statistical analysis was partially supported by the National Institutes of Health, National Institute of General Medical Sciences (grant 1 U54GM104938; principal investigator, Judith James).
Supplementary digital content available online.
Appendix
Thirty-one–question survey distributed electronically to all U.S. and Canada neurosurgery residents.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.-J., Ni Z.-Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Surgeons COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/triage Available at:
- 4.American College of Surgeons COVID-19: Recommendations for Management of Elective Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/elective-surgery Available at:
- 5.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: adaptation under fire: two Harvard neurosurgical services during the COVID-19 pandemic. https://doi.org/10.1093/neuros/nyaa146 [e-pub ahead of print]. Neurosurgery. accessed May 24, 2020. [DOI] [PMC free article] [PubMed]
- 7.Eichberg D.G., Shah A.H., Luther E.M. Letter: academic neurosurgery department response to COVID-19 pandemic: the University of Miami/Jackson Memorial Hospital model. https://doi.org/10.1093/neuros/nyaa118 [e-pub ahead of print]. Neurosurgery. accessed May 24, 2020. [DOI] [PMC free article] [PubMed]
- 8.Choi B.D. Editorial: a neurosurgery resident’s response to COVID-19: anything but routine. https://doi.org/10.3171/2020.4.jns201028 [e-pub ahead of print]. J Neurosurg. accessed May 24, 2020. [DOI] [PMC free article] [PubMed]
- 9.Carter B.S., Chiocca E.A. Editorial: COVID-19 and academic neurosurgery. https://doi.org/10.3171/2020.4.jns201013 [e-pub ahead of print]. J Neurosurg. accessed May 24, 2020. [DOI] [PMC free article] [PubMed]
- 10.Bambakidis N.C., Tomei K.L. Editorial: impact of COVID-19 on neurosurgery resident training and education. https://doi.org/10.3171/2020.3.jns20965 [e-pub ahead of print]. J Neurosurg. accessed May 24, 2020. [DOI] [PMC free article] [PubMed]
- 11.Statement of the American Association of Neurological Surgeons, American Board of Neurological Surgery, Congress of Neurological Surgeons, and Society of Neurological Surgeons before the Institute of Medicine on the Subject of Ensuring an Adequate Neurosurgical Workforce for the 21st Century. https://www.aans.org/pdf/Legislative/Neurosurgery%20IOM%20GME%20Paper%2012%2019%2012.pdf Available at:
- 12.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): cases in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html?fbclid=IwAR2YGdSiJ1zk6mktakCLsCqjU-tEq9XsvLMK2fGG0vmHPIsAdMgl8C13cOU Available at:
- 13.Chick R.C., Clifton G.T., Peace K.M. Using technology to maintain the education of residents during the COVID-19 pandemic. https://doi.org/10.1016/j.jsurg.2020.03.018 [e-pub ahead of print]. J Surg Educ. accessed May 24, 2020. [DOI] [PMC free article] [PubMed]
- 14.Schwartz A.M., Wilson J.M., Boden S.D., Moore T.J., Bradbury T.L., Fletcher N.D. Managing resident workforce and education during the COVID-19 pandemic: evolving strategies and lessons learned. JBJS Open Access. 2020;5:e0045. doi: 10.2106/JBJS.OA.20.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weber L. A Neurosurgeon Takes New Role to Care for Coronavirus Patients and Families. https://www.wsj.com/articles/a-neurosurgeon-takes-new-role-to-care-for-coronavirus-patients-and-families-11587979801 Available at:
- 16.Corley J. Doctors in Training Are Dying, and We Are Letting Them Down. https://www.forbes.com/sites/jacquelyncorley/2020/04/05/doctors-in-training-are-dying-and-we-are-letting-them-down/#a335c896cdcf Available at:
- 17.Safdar K., Palazzolo J., Adamy J., Ramachandran S. Young Doctors Struggle to Treat Coronavirus Patients: “We Are Horrified and Scared”. https://www.wsj.com/articles/young-doctors-struggle-to-treat-coronavirus-patients-we-are-horrified-and-scared-11588171553 The Wall Street Journal. Available at:
- 18.Tomlinson S.B., Hendricks B.K., Cohen-Gadol A.A. Editorial: innovations in neurosurgical education during the COVID-19 pandemic: is it time to reexamine our neurosurgical training models? https://doi.org/10.3171/2020.4.jns201012 [e-pub ahead of print]. J Neurosurg. accessed May 24, 2020. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Thirty-one–question survey distributed electronically to all U.S. and Canada neurosurgery residents.