Highlights
-
•
CRP level is elevated in COVID-19 patients.
-
•
The present meta-analysis revealed significant association of CRP with poor prognosis of COVID-19 infection.
-
•
Role of CRP in COVID-19 infection remained contradictory.
Keywords: CRP, Meta-analysis, COVID-19, Biomarkers, Survivors, Non-survivors
Abstract
Background
The novel coronavirus disease 2019 (COVID-19) first broke out in Wuhan, China, spread over 227 countries and caused approximately 0.3 million death worldwide. Several biomolecules have been explored for possible biomarkers for prognosis outcome. Although increased C reactive protein (CRP) is associated with death due to COVID-19 infections, results from different populations remain inconsistent. For a conclusive result, the present meta-analysis was performed.
Methods
We conducted a literature search in PubMed and Scopus database for the association of CRP concentration with COVID-19 disease outcomes. A total of 16 eligible studies were enrolled in the present analysis comprising of 1896 survivors and 849 non-survivors cases. Concentrations of CRP were compared and analyzed by a meta-analysis.
Results
Egger’s regression analysis (intercept = 0.04, P = 0.98, 95%CI = −5.48 to 5.58) and funnel plot revealed an absence of publication bias in the included studies. Due to the presence of significant heterogeneity across the studies (Q = 252.03, Pheterogeneity = 0.000, I2 = 93.65) random model was used for the analysis of the present study. The results of the meta-analysis demonstrated a significant role of CRP in COVID-19 infection outcome (Standard difference in means = 1.371, P = 0.000).
Conclusions
Concentrations of CRP remained high in patients who died of COVID-19 infection and could be a promising biomarker for assessing disease lethality.
1. Introduction
The first case of Novel coronavirus disease 2019 (COVID-19) was detected in Wuhan, China, in late December, that broke out worldwide, affecting over 227 countries and caused approximately three lakhs deaths till date (https://www.worldometers.info/coronavirus/ accessed on 13/05/2020). The mortality rate remained 14.50% worldwide (https://www.worldometers.info/coronavirus/ accessed on 13/05/2020). World Health Organisation had declared COVID-19 as pandemic disease (http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic). As of today (13/05/2020), the United States of America contributed the highest number of infected cases and death due to COVID-19 in comparison to other populations (https://www.worldometers.info/coronavirus/ accessed on 13/05/2020). COVID-19 infection displays a wide range of clinical manifestations. A recent study [1] highlighted cough, sputum production, diarrhoea, nausea/vomiting, and shortness of breath as more frequent clinical phenotypes in critical/non-survived COVID-19 patients, and in contrast, fever and headache were less prevalent. Furthermore, the pathogenesis of the diseases is regulated by several host factors. Various biomolecules such as aspartate aminotransferase, creatinine, high-sensitive cardiac troponin, procalcitonin, lactate dehydrogenase, and D-dimer has been increased in COVID-19 critical patients in comparison to those with non-severe infected cases [1].
The upregulation of C reactive protein (CRP) has been reported during severe acute respiratory syndrome (SARS) outbreak in 2002 and associated with respiratory dysfunctions and death of the patients [2]. Based on these observations, various studies were carried out in COVID-19 patients hypothesizing CRP as one of the possible biomolecules linked with the death of the infected patients. However, the observations of the reports remained contradictory.
2. Materials and methods
2.1. Literature search strategy
Two authors, RKK and BRS searched various databases (Medline, ScienceDirect, and Scopus) to trace eligible studies for the present meta-analysis. The keywords used for the search were “COVID-19, coronavirus 2019, 2019-nCoV, SARS-CoV-2, CRP, C-reactive protein, survivors, non-survivors, death, (till 10th May 2020). The title and abstracts of the articles obtained were screened, and apposite papers were downloaded. Furthermore, various preprint servers (bioRxiv, medRxiv and SSRN) were also screened with the above-mentioned keywords.
2.2. Inclusion and exclusion criteria
Various inclusion and exclusion criteria were considered in the present investigation. Inclusion of a report in the current meta-analysis must have a) added analysis for death and survivors, b) plasma/serum CRP concentrations, c) data must be presented in mean ± standard deviation (S.D) or median (interquartile range). Exclusion of the articles was based on the following conditions: a) duplicate articles, b) research articles, including only survivors or death cases, c) lack of CRP concentrations data d) review article, summaries, or case report.
2.3. Data extraction
Two authors BRS and AP extracted data such as authors' details, years of publication, population, number of COVID-19 infected subjects, death and survivors, CRP concentrations in mean ± S.D. or median (interquartile range), significance value. Details are shown in Table 1 .
Table 1.
Details of studies enrolled in the meta-analysis.
| Authors, y | Digital Object Identifier/ PMID | Country | Number of COVID-19 patients | Survivors |
Non-survivors |
P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number | CRP (mg/L) mean ± S.D./ median (IQR) | Mean ± S.D. | Number | CRP (mg/L) mean ± SD/median (IQR) | Mean ± S.D. | |||||
| Chen Tao et al. 2020 [9] | https://doi.org//10.1136/bmj.m1091 | China | 274 | 161 | 26.2 (8.7–55.2) | 30.03 ± 34.78 | 113 | 113 (69.1–168.4) | 116.83 ± 74.56 | <0.001 |
| Deng Yan et al. 2020 [4] | https://doi.org//10.1097/CM9.0000000000000824 | China | 225 | 116 | 3.22 (1.04–21.8) | 8.68 ± 15.58 | 109 | 109.25 (35–170.28) | 104.84 ± 101.63 | <0.001 |
| He Wenjuan et al. 2020 [10] | https://doi.org//10.1038/s41375-020-0836-7 | China | 13 | 5 | 121 (37–144) | 100.66 ± 107.60 | 8 | 68 (64–115) | 82.33 ± 45.56 | NS |
| Li Jingwen et al. 2020 (Preprint) [11] | https://doi.org//10.2139/ssrn.3546043 | China | 161 | 96 | 8.48 (0.13–310.10) | 106.23 ± 233.30 | 65 | 81.2 (8.4–284.4) | 124.66 ± 209.25 | 0.00 |
| Luo Xiaomin et al.2020 (Preprint) [12] | https://doi.org//10.1101/2020.03.21.20040360 | China | 298 | 214 | 9.65 (5–37.9) | 17.51 ± 24.55 | 84 | 100 (60.7–179.4) | 113.36 ± 89.53 | 0.000 |
| Ruan Qiurong et al. 2020 [13] | https://doi.org//10.1007/s00134-020-06028-z | China | 150 | 82 | 34.1 ± 54.5 | – | 68 | 126.6 ± 106.3 | – | <0.001 |
| Tomlins Jennifer et al. 2020 [14] | https://doi.org//10.1016/j.jinf.2020.04.020 | UK | 95 | 72$ | 36 (14–67) | 39 ± 40.09 | 20 | 77 (53–124) | 84.66 ± 56.64 | 0.001 |
| Tu Wen-Jun et al. 2020 [15] | https://doi.org//10.1007/s00134-020-06023-4 | China | 174 | 149 | 22 (6–45) | 24.33 ± 29.19 | 25 | 118 (22–184) | 108 ± 127.35 | <0.001 |
| Wang Kun et al. 2020a[16] | https://doi.org//10.1093/cid/ciaa538 | China | 296 | 277 | 11.4 (2.2–27.9) | 13.83 ± 19.17 | 19 | 88.6 (59.7–118.0) | 88.76 ± 43.49 | <0.001 |
| Wang Kun et al. 2020b[16] | https://doi.org//10.1093/cid/ciaa538 | China | 44 | 30 | 39.9 (11.9–68.1) | 39.96 ± 43.74 | 14 | 98.0 (85.5–117.8 | 83.86 ± 14.33 | <0.001 |
| Wang Lang et al. 2020 [17] | https://doi.org//10.1016/j.jinf.2020.03.019 | China | 339 | 274 | 44.2 (13.5–82.2) | 13.83 ± 19.15 | 65 | 102.0 (58.9–187.4) | 116.1 ± 97.42 | <0.001 |
| Wang Yang et al. 2020 [18] | https://doi.org//10.1164/rccm.202003-0736LE | China | 344 | 211 | 28 (6–67) | 33.66 ± 45.53 | 133 | 101 (61–153) | 105 ± 68.95 | <0.001 |
| Wu Chaomin et al. 2020 [19] | https://doi.org//10.1001/jamainternmed.2020.0994 | China | 84 | 40 | 69.20 (26.60–120.80) | 72.2 ± 72.43 | 44 | 90.85 (44.55 - >160) | 98.43 ± 88.56 | NS |
| Yan Yongli et al. 2020 ^ [20] | https://doi.org//10.1136/bmjdrc-2020-001343 | China | 48 | 9 | 13 (1–48) | 20.66 ± 41.10 | 39 | 97.2 (64.4–191.0) | 117.53 ± 97.43 | <0.001 |
| Zangrillo Alberto et al. 2020#[21] |
|
Italy | 73 | 56 | 180.3 (110.2–255.5) | 182 ± 110.56 | 17 | 256.4 (144.2–375.4) | 258.66 ± 186.89 | NS |
| Zhang Jingping et al. 2020 [22] | https://doi.org//10.1007/s10389-020-01291-2 | China | 19 | 11 | 86.9 (47.9–120.5) | 85.1 ± 61.58 | 8 | 166.15 (82.3–129.4) | 125.95 ± 42.08 | NS |
| Zhang Jun et al. 2020 [23] | https://doi.org//10.1016/j.jcv.2020.104392 | China | 111 | 93 | 7.93 (3.14–22.50) | 11.19 ± 14.57 | 18 | 79.52 (61.25–102.98) | 81.25 ± 33.57 | <0.001 |
NOTE: mean ± S.D. was calculated by Wan’s method, $CRP was not measured in three samples, ^ with diabetes patients, # mg/dl, a training cohort, b validation cohort.
2.4. Statistical analysis
The meta-analysis was performed by comprehensive meta-analysis V3.1 software (Biostat). Begg’s funnel plot and Eggers linear regression analysis were employed to test publication bias. CRP data was available in the median (interquartile range) format in most of the included reports, and those were converted into mean ± standard deviation according to an earlier report [3]. Association of CRP concentrations with COVID-19 disease prognosis was analyzed, and the combined standard difference in means and P-values were calculated. The Q test and I2 statistics evaluated heterogeneity among included reports. Based on the results of heterogeneity statistics, random (heterogeneous), or fixed model (non-heterogenous) were deployed for analysis. Furthermore, a sensitivity analysis was performed to test the robustness of the meta-analysis.
3. Results and discussion
A total of 122 and 153 articles were obtained after searching PubMed and Scopus, respectively. After screening the titles, abstracts, and full text based on inclusion and exclusion criterias, 14 articles, including data of 15 different cohorts were enrolled for the present analysis. Further, we found two articles related to our searched norms from preprint servers. Baseline data from all eligible publications were extracted and presented in Table 1. CRP data in median (interquartile range) were converted into the required format of CMA V3.1 software (mean ± S.D and sample number)[3].
Both Egger’s regression analysis (intercept = 0.04, 95% confidence interval = -5.48 to 5.58 and P = 0.98) and Begg’s funnel plot (Supplementary Fig.-1) revealed absence of publication bias in the studied reports. Further, significance heterogeneity across enrolled studies was observed (Q = 252.03, Pheterogeneity = 0.000, I2 = 93.65), suggesting a random model as an appropriate model for testing of association between CRP concentrations and mortality from COVID-19 infection.
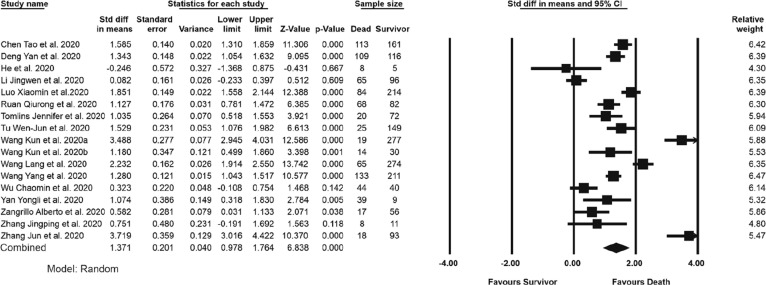
The result of the meta-analysis is shown in Fig. 1 . Patients, who died of COVID-19 infections, displayed significantly higher CRP concentrations compared to the survivors (P = 0.000, the standard difference in means = 1.371). Sensitivity analysis by the exclusion of a study each time demonstrated a significant association of CRP with mortality, further strengthen the observation of the present analysis (Supplementary Fig.-2). CRP is an acute-phase protein responsible for the clearance of pathogens through the complement system and enhanced phagocytosis. The most common complications in non-survivors COVID-19 infected patients include acute respiratory distress syndrome, acute cardiac injury, acute kidney injury, shock, disseminated intravascular coagulation, and a significant alterations in CRP level have been observed in these subjects [4]. A positive correlation between CRP concentrations with the lung lesion in COVID-19 infected patients has been demonstrated [2]. Furthermore, the induction of acute kidney damage [5] and the extent of the cardiac injury [6] has been directly linked with the CRP concentrations. Possibly for clearance of viral infections, immune system responded more vigorously by producing various immune molecules and production of CRP [7] beyond threshold limit may lead to dysfunction of various organ system in COVID-19 infected patients. Production of CRP is controlled by genetic makeup of the subject [8] and it would be interesting to investigate candidate genetic approach in different populations to obtain firm conclusion. The results of the present analysis and earlier observations altogether highlighted the importance of CRP as a possible biomarker for mortality by COVID-19 infection. However, more studies are required in different populations to validate the findings of the present report.
Fig. 1.
Forest plot of the association between C-reactive protein and survival status of COVID-19 infected patients. Data from earlier published articles were analyzed in Comprehensive meta-analysis software.
CRediT authorship contribution statement
Bikash R. Sahu: Investigation, Formal analysis. Raj Kishor Kampa: Investigation, Formal analysis. Archana Padhi: Writing - original draft. Aditya K. Panda: Conceptualization, Supervision, Formal analysis, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
AKP is supported by the DST-INSPIRE Faculty Grant from the Department of Science and Technology, Government of India, New Delhi, Grant id: IFA12/LSBM-46.
References
- 1.Zheng Z., Peng F., Xu B., Zhao J., Liu H., Peng J., Li Q., Jiang C., Zhou Y., Liu S., Ye C., Zhang P., Xing Y., Guo H., Tang W. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020 doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang L. C-reactive protein levels in the early stage of COVID-19. Medecine et maladies infectieuses. 2020 doi: 10.1016/j.medmal.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Method. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deng Y., Liu W., Liu K., Fang Y.-Y., Shang J., Zhou L., Wang K., Leng F., Wei S., Chen L., Liu H.-G. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin. Med. J. (Engl.) 2020 doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Y. Tang, X.R. Huang, J. Lv, A.C. Chung, Y. Zhang, J.Z. Chen, A.J. Szalai, A. Xu, H.Y. Lan, C-reactive protein promotes acute kidney injury by impairing G1/S-dependent tubular epithelium cell regeneration, Clinical science (London, England : 1979) 126(9) (2014) 645-59. [DOI] [PubMed]
- 6.Orn S., Manhenke C., Ueland T., Damas J.K., Mollnes T.E., Edvardsen T., Aukrust P., Dickstein K. C-reactive protein, infarct size, microvascular obstruction, and left-ventricular remodelling following acute myocardial infarction. Eur. Heart J. 2009;30(10):1180–1186. doi: 10.1093/eurheartj/ehp070. [DOI] [PubMed] [Google Scholar]
- 7.Salonen E.-M., Vaheri A. C-reactive protein in acute viral infections. J. Med. Virol. 1981;8(3):161–167. doi: 10.1002/jmv.1890080302. [DOI] [PubMed] [Google Scholar]
- 8.Brull D.J., Serrano N., Zito F., Jones L., Montgomery H.E., Rumley A., Sharma P., Lowe G.D., World M.J., Humphries S.E., Hingorani A.D. Human CRP gene polymorphism influences CRP levels: implications for the prediction and pathogenesis of coronary heart disease. Arterioscler. Thromb. Vasc. Biol. 2003;23(11):2063–2069. doi: 10.1161/01.ATV.0000084640.21712.9C. [DOI] [PubMed] [Google Scholar]
- 9.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., Ma K., Xu D., Yu H., Wang H., Wang T., Guo W., Chen J., Ding C., Zhang X., Huang J., Han M., Li S., Luo X., Zhao J., Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ (Clinical research ed.) 2020;368 doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He W., Chen L., Chen L., Yuan G., Fang Y., Chen W., Wu D., Liang B., Lu X., Ma Y., Li L., Wang H., Chen Z., Li Q., Gale R.P. COVID-19 in persons with haematological cancers. Leukemia. 2020:1–9. doi: 10.1038/s41375-020-0836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.J. Li, L. Xi, L. Huilin, F. Fang, L. Xuefei, Z. Dandan, S. Yu, L. Fengming, L. Na, Z. Qing, F. Xi, H. Shaoping, L. Zhicheng, X. Nian, Clinical Characteristics of Deceased Patients Infected with SARS-CoV-2 in Wuhan, China, SSRN (2020).
- 12.X. Luo, W. Zhou, X. Yan, T. Guo, B. Wang, H. Xia, L. Ye, J. Xiong, Z. Jiang, Y. Liu, B. Zhang, W. Yang, Prognostic value of C-reactive protein in patients with COVID-19, medRxiv (2020) 2020.03.21.20040360. [DOI] [PMC free article] [PubMed]
- 13.Ruan Q., Yang K., Wang W., Jiang L., Song J. Correction to: Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020:1–4. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomlins J., Hamilton F., Gunning S., Sheehy C., Moran E., MacGowan A. Clinical features of 95 sequential hospitalised patients with novel coronavirus 2019 disease (COVID-19), the first UK cohort. J. Infect. 2020 doi: 10.1016/j.jinf.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tu W.J., Cao J., Yu L., Hu X., Liu Q. Clinicolaboratory study of 25 fatal cases of COVID-19 in Wuhan. Intensive Care Med. 2020:1–4. doi: 10.1007/s00134-020-06023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang K., Zuo P., Liu Y., Zhang M., Zhao X., Xie S., Zhang H., Chen X., Liu C. Clinical and laboratory predictors of in-hospital mortality in patients with COVID- 19: a cohort study in Wuhan, China. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 2020 doi: 10.1093/cid/ciaa538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang L., He W., Yu X., Hu D., Bao M., Liu H., Zhou J., Jiang H. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J. Infect. 2020;80(6):639–645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y., Lu X., Li Y., Chen H., Chen T., Su N., Huang F., Zhou J., Zhang B., Yan F., Wang J. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am. J. Respir. Crit. Care Med. 2020;201(11):1430–1434. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C., Zhang Y., Song J., Wang S., Chao Y., Yang Z., Xu J., Zhou X., Chen D., Xiong W., Xu L., Zhou F., Jiang J., Bai C., Zheng J., Song Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 Pneumonia in Wuhan, China. JAMA Internal Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yan Y., Yang Y., Wang F., Ren H., Zhang S., Shi X., Yu X., Dong K. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res. Care. 2020;8(1) doi: 10.1136/bmjdrc-2020-001343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zangrillo A., Beretta L., Scandroglio A.M., Monti G., Fominskiy E., Colombo S., Morselli F., Belletti A., Silvani P., Crivellari M., Monaco F., Azzolini M.L., Reineke R., Nardelli P., Sartorelli M., Votta C.D., Ruggeri A., Ciceri F., De Cobelli F., Tresoldi M., Dagna L., Rovere-Querini P., Serpa Neto A., Bellomo R., Landoni G. Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit. Care Resusci.: J. Australasian Acad. Crit. Care Med. 2020 doi: 10.1016/S1441-2772(23)00387-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.J. Zhang, P. Liu, M. Wang, J. Wang, J. Chen, W. Yuan, M. Li, Z. Xie, W. Dong, H. Li, Y. Zhao, L. Wan, T. Chu, L. Wang, H. Zhang, T. Tao, J. Ma, The clinical data from 19 critically ill patients with coronavirus disease 2019: a single-centered, retrospective, observational study, Zeitschrift fur Gesundheitswissenschaften = Journal of public health (2020) 1-4. [DOI] [PMC free article] [PubMed]
- 23.Zhang J., Yu M., Tong S., Liu L.Y., Tang L.V. Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China. J. Clin. Virol.: Off. Publ. Pan Am. Soc. Clin. Virol. 2020;127 doi: 10.1016/j.jcv.2020.104392. [DOI] [PMC free article] [PubMed] [Google Scholar]