Abstract
Background
Before the COVID-19 pandemic, telemedicine utilization was mostly used for postoperative visits only in neurosurgery. Shelter-in-place measures led the rapid expansion of telemedicine to address the needs of the neurosurgical patient population. Our goal is to determine the extent of adoption of telemedicine across tumor, vascular, spine, and function neurosurgery and utilization for new patient visits.
Methods
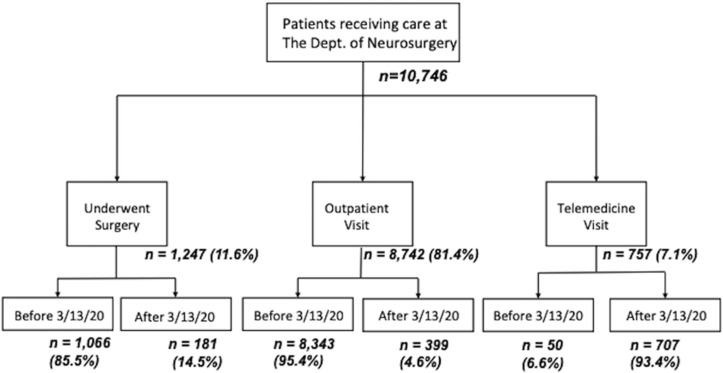
A single-center retrospective cohort study of patients who received neurosurgical care at a tertiary academic center from February to April 2020 was conducted. Patients evaluated from March to April 2019 were included for comparison. A total of 10,746 patients were included: 1247 patients underwent surgery, 8742 were seen in clinic via an in-person outpatient visit, and 757 were assessed via telemedicine during the study period.
Results
A 40-fold increase in the use of telemedicine was noted after the shelter-in-place measures were initiated with a significant increase in the mean number of patients evaluated via telemedicine per week across all divisions of neurosurgery (4.5 ± 0.9 to 180.4 ± 13.9, P < 0.001). The majority of telemedicine appointments were established patient visits (61.2%), but the proportion of new patient visits also significantly increased to an average of 8.2 ± 5.3 per week across all divisions.
Conclusions
Use of telemedicine drastically increased across all 4 divisions within neurosurgery with a significant increase in online-first encounters in order to meet the needs of our patients once the shelter-in-place measures were implemented. We provide a detailed account of the lessons learned and discuss the anticipated role of telemedicine in surgical practices once the shelter-in-place measures are lifted.
Key words: COVID-19, Neurosurgery, Telemedicine
Abbreviations and Acronyms: COVID-19, Coronavirus disease identified in 2019
Introduction
Telemedicine was implemented in the 1990s, but it has been slow to develop and only had modest increases through the previous decade. It was first adopted to cover rural Medicare beneficiaries in 1997 with its total expenditures for the first 5 years of coverage amounting to only $3 million dollars.1 This slow development has been mainly due to financial barriers, fear of losing the strong physician-patient relationship, and limitations of the physical examination.
The use of telehealth, however, has become more mainstream since the early 2010s in certain subspecialties. Our hospital initiated its telehealth program approximately 10 years ago by building a widespread neuroscience network that fueled widespread implementation within the rest of the institutional enterprise. This telehealth program initially became prevalent for inpatient care, particularly via robot evaluations for rapid stroke assessment and telerounds in neurointensive care units. However, the impact of telehealth on the outpatient practice had been more limited. There has been a paucity of data on telemedicine usage in neurosurgery, with the majority of the literature arising in the past 2 years.2, 3, 4, 5
The COVID-19 national emergency declared in the United States on March 13, 2020 dramatically changed the role of telemedicine in clinical care since shelter-in-place orders were issued throughout the country. In an effort to limit the patient and health care provider exposure, telemedicine has been an essential platform. As neurosurgical providers interact with patients in the operating room, intensive care unit, emergency department, and outpatient clinics each day, they place themselves and patients at an increased risk of exposure. There is a thus a widespread need for further implementation of telemedicine to reduce viral exposure. This manuscript shares the experience and lessons learned at a large tertiary care academic neurosurgery department required to maximally increase telemedicine use as a response to the COVID-19 pandemic.
Methods
Patient Selection, Variables, and Outcomes
The study protocol was approved by the University Institutional Review Board. A retrospective analysis of patients who received care through the Department of Neurosurgery between February 1, 2020 through April 18, 2020 was performed. Patients treated the previous year between March 3, 2019 and April 20, 2019 were also included in the study for comparison. A total of 10,746 patients met the inclusion criteria. Of them, 1247 patients underwent surgery, 8742 were seen in clinic via an in-person meeting, and 757 were assessed via telemedicine during the study periods (Figure 1 ). These patients received care by 14 attending neurosurgeons, 1 interventional neurologist, 2 neurooncologists, and 4 nurse practitioners. Of the attending faculty, 6 were within the tumor division, 5 were from the vascular division (4 were dual-trained open and endovascular and 1 endovascular), 4 were from the spine division, and 2 were from the functional division. Data were collected on the number of telemedicine and in-person appointments for each of the 4 divisions within neurosurgery (vascular, spine, tumor, functional); the number of new patient visits; established patient visits; and postoperative visits. The COVID-19 national emergency was declared in the United States on March 13, 2020, which is used as the reference point in this study. Data analysis was conducted after removal of identifiable patient health information. The main endpoints of the study are the usage rate of telemedicine before and after the COVID-19 outbreak and the distribution of telemedicine use across the neurosurgical divisions.
Figure 1.
Patient selection flowchart.
Telemedicine Environment
Our department has used the Teladoc Health (Teladoc Health, Purchase, Harrison, New York, USA) and the VidyoConnect (Vidyo Health, Rochelle Park, New Jersey, USA) telemedicine platforms, which are integrated to the EPIC electronic health records (Epic Systems Corporation, Verona, Wisconsin, USA). Physicians established a telemedicine environment at home that consisted of the following setup: 1 device to remotely access the hospital Internet in order to use the Epic electronic health record and the telemedicine software and a second device to video conference with nursing staff. Nursing staff was also able to join the physician-patient encounter when necessary or videoconference with the patient independently before or after the physician. This setup thus enabled 360-degree communication between the neurosurgical team and the patient. Imaging was reviewed with patients using the share-screen functionality of the videoconferencing telemedicine software. Due to the rapid expansion of telemedicine, several technical issues were initially encountered: slow Internet connection speed, dropped calls, and video connection without audio. In those circumstances, the faculty and supporting staff combined other Health Insurance Portability and Accountability Act−compliant applications outside of the institution's bandwidth in order to carry out the telemedicine visit. Additionally, starting telemedicine visits earlier in the day (i.e., 5:30–6:00 a.m.) helped avoid network congestion noted later in the day.
Statistical Analysis
Data are presented as mean and standard deviation for continuous variables and as frequency for categorical variables. Analysis was performed using the unpaired t-test, chi-squared test, and Fisher exact test, as appropriate. The Shapiro-Wilk test was used to determine normality of variables; variables with a P value ≤ 0.05 were considered not normally distributed. The Mann-Whitney test was performed for continuous variables that did not conform to normal distribution. Not normally distributed variables were reported as medians if similar distribution was noted and mean ranks if differently distributed. Results are separated by department and visit type as appropriate. Analysis was carried out using the unpaired t-test, chi-squared test, and Fisher exact tests. P values of ≤0.05 were considered statistically significant. Statistical analysis was carried out with IBM SPSS (version 24.0, IBM Corp, Armonk, New York, USA).
Results
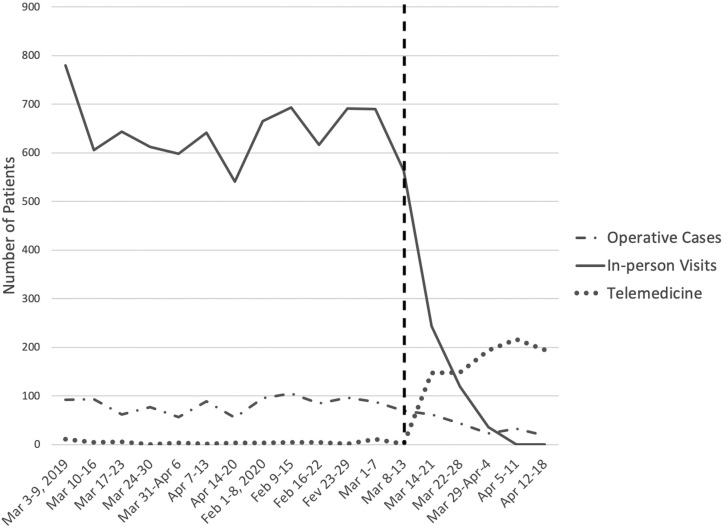
A total of 10,746 patients were included in this study: 1247 (11.6%) patients underwent surgery, 8742 (81.4%) were seen in clinic via an in-person meeting, and 757 (7.1%) had a telemedicine appointment. The mean number of patients who had surgery, an in-person clinic appointment, or a telemedicine visit during this study period is displayed in Figure 2 .
Figure 2.
Weekly average number of operative cases, in-person clinic and telemedicine visits, and before and after the shelter-in-place order was placed.
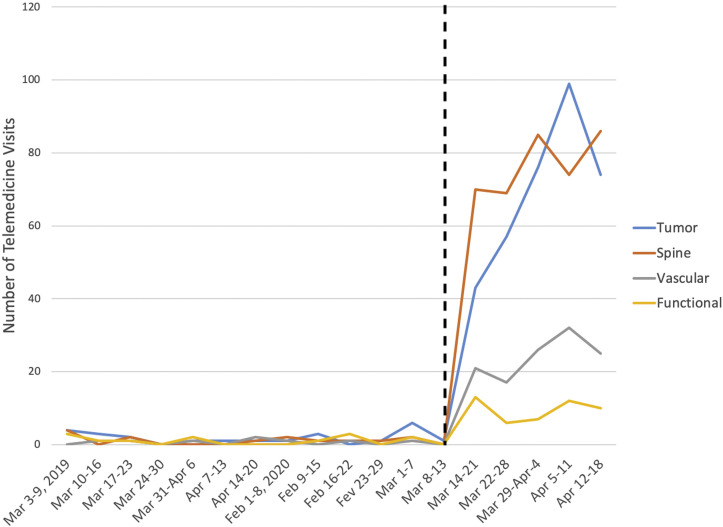
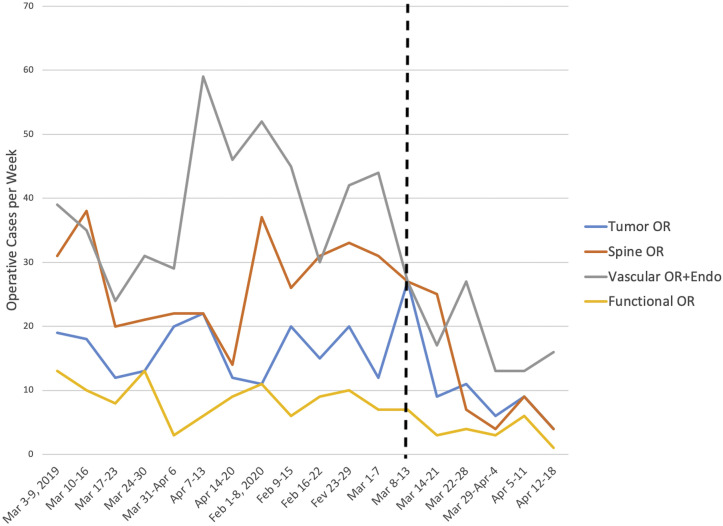
The number of operative cases per week decreased significantly after the shelter-in-place measures were implemented from 91.5 ± 14.5 to 38.7 ± 10.5 (P < 0.001). In-person clinic visits also decreased dramatically from 641.8 ± 63.2 to 79.8 ± 103.9 (P < 0.001) as represented in Table 1 and Figure 2 . The breakdown of visits by division is displayed in Table 2 and Figure 3 . During the same study period, the number of telemedicine visits increased from 4.5 ± 0.9 before March 13, 2020 to 180.4 ± 13.9 after March 13, 2020 (P < 0.001). A statistically significant increase in the number of telemedicine visits was seen in all 4 divisions (Table 3 ), while a statistically significant decrease was noted in the number of operative cases per week in all 4 divisions (Figure 4 ).
Table 1.
Number of Operative Cases and In-Person Outpatient Visits per Week for the Department of Neurosurgery Before and After Shelter-in-Place Measures
| Before March 13, 2020 | After March 13, 2020 | P Value | |
|---|---|---|---|
| Operative cases: | 91.5 ± 14.5 | 38.2 ± 13.1 | <0.001 |
| Tumor | 17.0 ± 4.9 | 7.8 ± 2.8 | 0.001 |
| Spine | 27.2 ± 7.1 | 9.8 ± 8.8 | <0.001 |
| Vascular | 38.7 ± 10.5 | 17.2 ± 4.8 | 0.001 |
| Functional | 8.6±2.9 | 3.4 ± 1.8 | 0.002 |
| In-person clinic visits: | 641.8 ± 63.2 | 79.8 ± 103.9 | <0.001 |
| Tumor | 169.9 ± 37.2 | 18.8 ± 22.9 | <0.001 |
| Spine | 337.2 ± 51.3 | 40.0 ± 56.1 | <0.001 |
| Vascular | 83.8 ± 21.9 | 15.4 ± 18.6 | <0.001 |
| Functional | 50.9 ± 14.0 | 5.6 ± 8.2 | <0.001 |
Table 2.
Number of In-Person Visits per Week by Division Before and After Shelter-in-Place Measures
| Before March 13, 2020 | After March 13, 2020 | P Value | |
|---|---|---|---|
| Tumor: | |||
| EPV | 85.1 ± 21.4 | 2.6 ± 3.7 | <0.001 |
| NPV | 35.9 ± 32.8 | 1.4 ± 2.2 | 0.035 |
| Postoperative | 51.5 ± 20.6 | 13.8 ± 15.7 | 0.002 |
| Spine: | |||
| EPV | 136.6 ± 24.2 | 3.4 ± 7.1 | <0.001 |
| NPV | 62.2 ± 11.1 | 1.6 ± 3.1 | <0.001 |
| Postoperative | 122.4 ± 27.8 | 34.2 ± 44.9 | <0.001 |
| Vascular: | |||
| EPV | 29.7 ± 8.3 | 1.0 ± 2.2 | <0.001 |
| NPV | 15.8 ± 9.2 | 0.6 ± 1.3 | <0.001 |
| Postoperative | 35.2 ± 12.8 | 13.8 ± 16.0 | 0.009 |
| Functional: | |||
| EPV | 16.0 ± 12.1 | 0.0 ± 0.0 | <0.001 |
| NPV | 6.2 ± 5.7 | 0.0 ± 0.0 | 0.029 |
| Postoperative | 17.0 ± 8.5 | 0.0 ± 0.0 | 0.002 |
EPV, established patient visit; NPV, new patient visit.
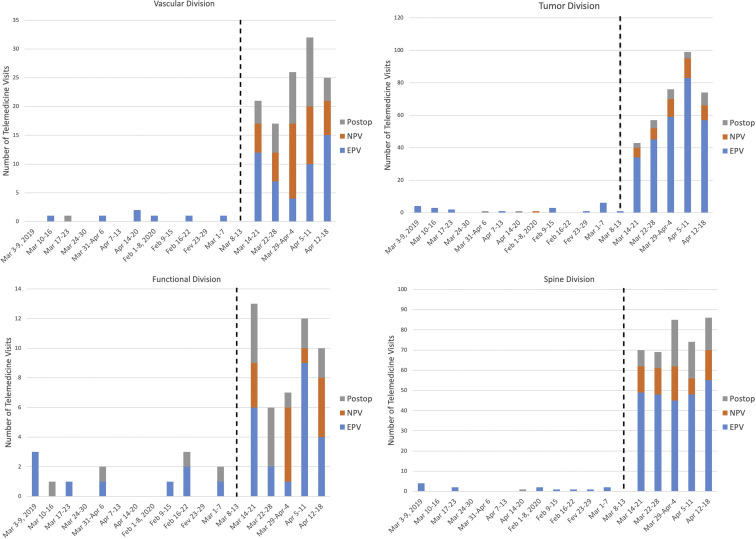
Figure 3.
Average number of weekly telemedicine visits for the spine, tumor, vascular, and functional divisions before and after the COVID-19 national emergency.
Table 3.
Number of Telemedicine Visits per Week by Division Before and After Shelter-in-Place Measures
| Before March 13, 2020 | After March 13, 2020 | P Value | |
|---|---|---|---|
| Total telemedicine (±SEM) | 4.5 ± 0.9 | 180.4 ± 13.9 | <0.001 |
| Tumor | 1.8 ± 0.5 | 69.8 ± 9.5 | 0.002 |
| Spine | 1.1 ± 0.3 | 76.8 ± 3.7 | <0.001 |
| Vascular | 0.6 ± 0.2 | 24.2 ± 2.5 | 0.001 |
| Functional | 1.0 ± 0.3 | 9.6 ± 1.4 | 0.003 |
| Telemedicine tumor visits (±SEM) | |||
| EPV | 1.6 ± 0.5 | 55.6 ± 8.2 | 0.003 |
| NPV | 0.1 ± 0.1 | 9 ± 1.1 | 0.001 |
| Postoperative | 0.2 ± 0.1 | 5.2 ± 0.9 | 0.004 |
| Telemedicine spine visits (±SEM) | |||
| EPV | 1.0 ± 0.3 | 49.0 ± 1.6 | <0.001 |
| NPV | 0.0 | 13.2 ± 1.5 | 0.001 |
| Postoperative | 0.1 ± 0.1 | 14.6 ± 2.9 | 0.008 |
| Telemedicine vascular visits (±SEM) | |||
| EPV | 0.7 ± 0.2 | 9.6 ± 1.9 | 0.009 |
| NPV | 0.0 | 7.8 ± 1.6 | 0.008 |
| Postoperative | 0.1 ± 0.1 | 7.8 ± 1.6 | 0.013 |
| Telemedicine functional visits (±SEM) | |||
| EPV | 0.7 ± 0.3 | 4.4 ± 1.4 | 0.06 |
| NPV | 0.0 | 2.6 ± 0.9 | 0.049 |
| Postoperative | 0.3 ± 0.1 | 2.6 ± 0.6 | 0.017 |
SEM, standard error of mean; EPV, established patient visit; NPV, new patient visit.
Figure 4.
Average number of weekly operative cases for the spine, tumor, vascular, and functional divisions before and after the COVID-19 national emergency.
There were no new patient visits performed via telemedicine before the shelter-in-place measures, but the number rose significantly across all 4 divisions to an average of 8.2 ± 2.1 per week after March 13 (P < 0.05). The proportion of patients who underwent a new patient, established, or postoperative follow-up visit in each of the divisions is displayed in Table 3 and Figure 5 .
Figure 5.
Proportion of established, new, and postoperative patient visits before and after the COVID-19 national emergency.
Discussion
The COVID-19 pandemic has tremendously impacted all clinical specialties over the span of a few weeks. The use of telehealth at our hospital in the past decade facilitated the transition to telemedicine for managing established patients and accepting new patients during the COVID-19 outbreak. Despite any prior barriers regarding the applicability of telemedicine to neurosurgical patients, our findings demonstrate widespread adoption of this technology through the 4 neurosurgery divisions.
Developing a solid foundation for a telemedicine practice before the current pandemic was instrumental in adjusting to the national emergency. Our experience with telestroke has led to faster diagnosis of stroke, more frequent administration of t-PA, and improved long-term outcomes.6, 7, 8 Importantly, the telestroke program also laid the foundation for effective and efficient use of telemedicine in general at our university. As each state established lockdown measures, health care systems had to urgently transition to telemedicine to minimize exposure. The prior use and training of telemedicine at our hospital allowed for a seamless transition to virtual office visits in order to maintain social distancing.
The rapid expansion of a telemedicine practice is not an easy feat; success is contingent on a strong telemedicine infrastructure. Complex telecommunication requirements and availability of high-speed broadband access are necessary to enable use of telemedicine for daily work.9 Our prior history of telemedicine use had prepared our institution to adapt to the COVID national emergency and promptly switch to the new means of delivering health care across the hospital system nearly overnight. Issues with bandwidth and Internet connection speed were encountered at first as the use of telemedicine was rapidly increased across the enterprise. On the basis of this experience, we learned that investing in such infrastructure and training is only 1 important factor necessary to rapidly expand the application of the telemedicine platform. It is equally important to estimate the number of new telemedicine users and encounters to sufficiently expand the bandwidth to support the increased use of the platform. We also found that telemedicine allowed our staff to not only provide seamless care to established and postoperative patients but also address new patients who may otherwise avoid seeking care for their health problems in fear of contracting COVID-19.
The Centers for Medicare & Medicaid Services implemented the 1135 Waiver on March 6, 2020, which expanded the coverage of telehealth services by Medicare. Under this waiver, telehealth visits are covered even outside of designated rural areas and reimbursed similarly to the equivalent in-person visits for the duration of the COVID-19 national emergency. This further enables continuity of care for patients. The neurosurgery department changed all outpatient office visits to telehealth visits within a 1-week timeframe. This was done for all staff including physicians, nurse practitioners, administrators, nurses, and scribes across all divisions. Although we have developed an effective use of the telemedicine platform, the reimbursement by Medicare and private insurances once the pandemic resolves will be instrumental in determining the sustainability of telemedicine.
The COVID pandemic also highlighted some limitations of telemedicine that we need to take into consideration. While there are a number of companies in this space, there is a lack of telemedicine technology that is specific to the needs of the neurosurgical patient population and captures the nuances of the neurologic examination. This has created a tremendous opportunity for the application of artificial intelligence to telemedicine in order to improve our diagnostic and follow-up capabilities. Furthermore, as neurosurgical practices increasingly use telemedicine, the reimbursement models will need to be updated in order to incentivize the efficient and safe application of this technology.10 , 11 Before the 1135 Waiver, telemedicine was mostly used for follow-up care; however, our findings suggest increasing acceptance of online new-patient visits by both patients and physicians. Lastly, as telemedicine allows for coverage of larger catchment areas, licensing across states remains an outstanding issue.
Understanding the benefits and challenges of telemedicine during this crisis will be useful in order to better incorporate telemedicine into neurosurgery once the pandemic has resolved. Our findings demonstrate that it is feasible to maintain a high volume of outpatient practice via telemedicine and appropriately triage which patients need to be seen in person. The benefits of telemedicine for patients are numerous: it allows patients to avoid missing work, avoids inconveniencing a family member if needed for assistance, and avoids a potentially long commute with associated costs. Telemedicine not only improves clinic efficiency and patient satisfaction but also optimizes the surgeon's schedule. Surgeons can spread out their telemedicine visits throughout the week including early morning and evening. This strategy could allow the surgeon to expand the number of operative days or free up additional time for academic pursuits. Also, this would likely help improve patient satisfaction by offering office hours before or after the average workday. Telemedicine is not likely to diminish the quality of physician-patient encounters; instead, it may enhance the relationship by making health care delivery more efficient and convenient.
Conclusion
The COVID-19 pandemic has taught us many lessons about telemedicine. Our early adoption of telemedicine before the pandemic allowed for a rapid transition across all divisions within neurosurgery. We also learned that medical centers need to estimate the surge in telemedicine use and increase Internet bandwidth in advance. Understanding insurance reimbursement will help in the optimal incorporation of telemedicine into each practice after the pandemic resolves. Finally, there is clear need to further develop the telemedicine technology in an effort to fully address the needs of the neurosurgical patient population.
CRediT authorship contribution statement
Nikolaos Mouchtouris: Writing - original draft, Writing - review & editing, Formal analysis. Pascal Lavergne: Writing - review & editing, Methodology. Thiago S. Montenegro: Investigation, Data curation. Glenn Gonzalez: Investigation, Data curation. Michael Baldassari: Writing - review & editing, Formal analysis. Ashwini Sharan: Resources, Supervision. Pascal Jabbour: Resources, Supervision. James Harrop: Project administration, Visualization. Robert Rosenwasser: Validation, Resources, Conceptualization, Supervision, Writing - review & editing.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Data
References
- 1.Neufeld J.D., Doarn C.R. Telemedicine spending by Medicare: a snapshot from 2012. Telemed J E Health. 2015;21:686–693. doi: 10.1089/tmj.2014.0185. [DOI] [PubMed] [Google Scholar]
- 2.Chhabra H.S., Sharma S., Verma S. Smartphone app in self-management of chronic low back pain: a randomized controlled trial. Eur Spine J. 2018;27:2862–2874. doi: 10.1007/s00586-018-5788-5. [DOI] [PubMed] [Google Scholar]
- 3.Cottrell M.A., O’Leary S.P., Swete-Kelly P. Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskelet Sci Pract. 2018;38:99–105. doi: 10.1016/j.msksp.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Goz V., Spiker W.R., Brodke D. Mobile messaging and smartphone apps for patient communication and engagement in spine surgery. Ann Transl Med. 2019;7:S163. doi: 10.21037/atm.2019.08.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Linden S.D., Sitskoorn M.M., Rutten G.-J.M., Gehring K. Feasibility of the evidence-based cognitive telerehabilitation program Remind for patients with primary brain tumors. J Neurooncol. 2018;137:523–532. doi: 10.1007/s11060-017-2738-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chalouhi N., Dressler J.A., Kunkel E.S.I. Intravenous tissue plasminogen activator administration in community hospitals facilitated by telestroke service. Neurosurgery. 2013;73:662–667. doi: 10.1227/NEU.0000000000000073. [DOI] [PubMed] [Google Scholar]
- 7.Mouchtouris N., Al Saiegh F., Fitchett E. Revascularization and functional outcomes after mechanical thrombectomy: an update to key metrics. http://www.ncbi.nlm.nih.gov/pubmed/31518981 [e-pub ahead of print]. J Neurosurg. Available at: [DOI] [PubMed]
- 8.Zanaty M., Chalouhi N., Starke R.M. Epidemiology of a large telestroke cohort in the Delaware valley. Clin Neurol Neurosurg. 2014;125:143–147. doi: 10.1016/j.clineuro.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Wilcock A.D., Rose S., Busch A.B. Association between broadband Internet availability and telemedicine use. JAMA Intern Med. 2019;179:1580–1582. doi: 10.1001/jamainternmed.2019.2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grossman S.N., Han S.C., Balcer L.J. Rapid implementation of virtual neurology in response to the COVID-19 pandemic. https://doi.org/10.1212/WNL.0000000000009677 [e-pub ahead of print]. Neurology. [DOI] [PubMed]
- 11.Scott Kruse C., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.