Supplemental Digital Content is available in the text.
Key Words: femoral anteversion, validity, mobile application, computed tomography, cerebral palsy
Abstract
Background:
Computed tomography (CT) provides benefits for 3-dimensional (3D) visualization of femur deformities. However, the potential adverse effects of radiation exposure have become a concern. Consequently, a biplanar imaging system EOS has been proposed to enable reconstruction of the 3D model of the femur. However, this system requires a calibrated apparatus, the cost of which is high, and the area occupied by it is substantial. The purpose of this study was to develop a mobile application that included a new method of 3D reconstruction of the femur from conventional radiographic images and to evaluate the validity and reliability of mobile the application when measuring femoral anteversion.
Methods:
The statistical shape model, graph-cut algorithm, and iterative Perspective-n-Point algorithm were utilized to develop the application. The anteroposterior and lateral images of a femur can be input using the embedded camera or by file transfer, and the touch interface aids accurate contouring of the femur. Regarding validation, the CT scans and conventional radiographic images of 36 patients with cerebral palsy were used. To evaluate concurrent validity, the femoral anteversion measurements on the images reconstructed from the mobile application were compared with those from the 3D CT images. Three clinicians assessed interobserver reliability.
Results:
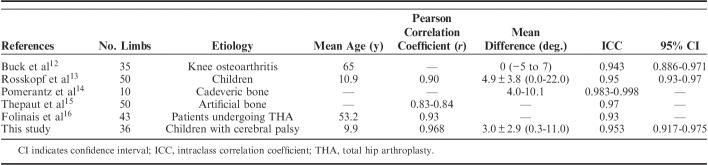
The mobile application, which reconstructs the 3D image from conventional radiographs, was successfully developed. Regarding concurrent validity, the correlation coefficient between femoral anteversion measured using 3D CT and the mobile application was 0.968 (P<0.001). In terms of interobserver reliability, the intraclass correlation coefficient among the 3 clinicians was 0.953.
Conclusions:
The measurement of femoral anteversion with the mobile application showed excellent concurrent validity and reliability in patients with cerebral palsy. The proposed mobile application can be used with conventional radiographs and does not require additional apparatus. It can be used as a convenient technique in hospitals that cannot afford a CT machine or an EOS system.
Level of Evidence:
Level III—diagnostic.
Cerebral palsy (CP) is a group of permanent developmental disorders caused by nonprogressive disturbances occurring in the immature brain of a developing fetus or infant.1 Increased femoral anteversion is a common deformity in patients with CP.2 It results in in-toeing gait, and femoral derotation osteotomy is commonly performed to treat this problem.3,4 Therefore, accurate measurement of femoral anteversion is essential for preoperative planning and good surgical outcomes.5
Femoral anteversion can be measured by physical examination, 2-dimensional (2D)/3-dimensional (3D) computed tomography (CT), magnetic resonance imaging, and the EOS system. Even though physical examination has proven to be a reliable and valid tool,6 imaging methods are still widely used as a compensatory tool because they have the merits of visualization and objectivity. Measurement using CT is an intuitive, reliable, and valid method,6 but the potential adverse effects of radiation have become an issue of concern, especially in the pediatric population, as children are more susceptible to the effects of radiation.7 Magnetic resonance imaging can be used as an alternative to CT,8 but it has several drawbacks including increased cost, time, possible motion artifacts, and the need for anesthesia in children. A low-dose biplanar x-ray technology (EOS; EOS Imaging, Paris, France) using 2 orthogonal radiographic images has been developed to reduce the radiation dose.9–11 Several studies have reported excellent concurrent validity of the EOS system for measuring femoral anteversion.12–16 However, this system requires another apparatus, the cost of which is high, and the area occupied by it is substantial. Therefore, purchasing an EOS system only for 3D reconstruction may not be appropriate in some hospitals or countries.
The use of mobile devices such as smartphones and tablets has become widespread. Moreover, the specifications of mobile devices can be improved and upgraded rapidly; they can, therefore, be considered comparable to the specifications of various medical devices.
Therefore, the purpose of this study was to develop and validate a mobile application that can reconstruct a 3D model of the femur from conventional radiographic images, and does not need a calibrated apparatus such as EOS. In terms of validation, we focused on the measurements of femoral anteversion in this study.
METHODS
This study was approved by the institutional review board of our hospital (IRB no. B-1502/288-104). The need for informed consent was waived because the study only used the existing CT and radiographic images.
Development of the Mobile Application
Reconstruction of a 3D model from a few 2D images is arithmetically not possible. However, if we have prior knowledge of the 3D model, reconstruction is possible, that is, we can find the most appropriate 3D model that fits the 2D images. Such a 3D model is called a “statistical shape model (SSM).” The EOS system also adopts the concept of the SSM. In our mobile application, we used an SSM utilizing the femurs of 54 patients with CP.17
Theoretically, ≥2 calibrated images are needed to construct an accurate 3D model using SSM; that is, we should know the exact location of the cameras or sensors. A biplanar calibrated system such as EOS can be used to solve this problem. However, a conventional radiographic system can only take anteroposterior (AP) and lateral (LAT) images separately. The hardware does not support the calibration, that is, we do not know the exact location of a sensor. Recently, the iterative Perspective-n-Point algorithm, which solves the calibration and the reconstruction problems, has been proposed and utilized for the development of the mobile application. The calibration and reconstruction were optimized by minimizing the difference between the projected contour of the femur shape and the contour of the radiographic image (Video Supplement 1, Supplemental Digital Content 1, http://links.lww.com/BPO/A245).
To apply the above technology to a medical situation, the following factors should be considered. First, transferring images between incompatible devices is often inconvenient, even though the images can be stored digitally. Mobile devices usually have a high-resolution camera; therefore, the application was developed so that a user can easily input a printed film or a digital image displayed on a monitor screen by taking a photograph using an embedded camera. Second, because any automatic algorithms can cause errors, a way to correct the errors is required. Mobile devices usually have a high-performance touch interface; therefore, the application was developed to provide not only automatic contouring with a graph-cut algorithm but also an intuitive touch interface for modifying the contour of a radiograph and navigating the 3D view to verify the reconstruction result. Third, any apparatus other than the mobile device should not be needed, that is, the mobile application should be developed to self-contained. The 3D reconstruction and clinical measurements can be therefore obtained without requiring the use of additional devices or softwares.
Considering all the above factors, a mobile application was developed using the Unity 3D engine to support multiple platforms, such as iOS and Android.
Consensus Building of the Measurements
The validity and reliability studies were performed by 3 examiners (K.H.S., H.C.K., and M.I.K.), who were not involved in the development of the mobile application. They are all affiliated to different institutes, having 15, 8, and 7 years of orthopaedic experience, respectively.
After estimating the minimal sample size, the radiographic images of 36 patients were included for validation. The inclusion criteria were as follows: (1) consecutive patients with CP during the period between March 2003 and December 2017, and (2) who underwent torsional CT scan and AP and LAT radiographs of the femur with an interval of <1 month. The exclusion criteria were as follows: (1) inadequate coverage or quality of the radiographs, (2) fracture of the femur, and (3) patients having implants, such as plates and screws.
In our institute, CT scans were obtained using Mx8000-IDT (Philips Research, Eindhoven, The Netherlands) machine. AP and LAT radiographs of the femur were obtained using a UT 2000 x-ray machine (Philips Research) under the following conditions: source-to-image distance of ∼100 cm, 60 kVp, and 10 mAs.
A consensus-building session was held by all examiners before the measurements. The reconstruction process using the mobile application was as follows: (1) iPad fourth generation was used for the validation study, (2) the images of AP and LAT femur radiographs were obtained with an embedded camera, (3) the touch interface was used to aid in the contouring of the femur, and (4) after reconstruction, the femoral anteversion was measured using the embedded tool.
Femoral anteversion was defined as the angle between a line connecting the posterior margins of each femoral condyle and another line passing through the center of the femoral head and the midpoint of the femoral neck (Fig. 1).
FIGURE 1.
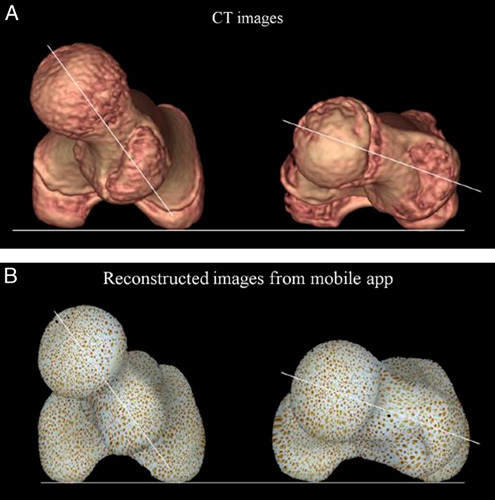
Measurement of femoral anteversion using 3D computed tomographic images (A) and using reconstructed images from the mobile application (B). Femoral anteversion was defined as the angle between a line connecting the posterior margins of each femoral condyle and another line passing through the center of the femoral head and the midpoint of the femoral neck.
Testing Concurrent Validity and Interobserver Reliability
After consensus-building, the 3 examiners had a 20-minute orientation and training for reconstruction with 5 femurs. Thereafter, 3 examiners independently reconstructed the femur from AP and LAT radiographs, which were randomly presented by a research assistant who did not participate in the current study.
To evaluate the concurrent validity, the femoral anteversion on the 3D CT image was measured by the 1st author with the use of the Picture Archiving and Communication System Software (PACS) (Infinitt Healthcare, Seoul, Korea). The correlation coefficient was calculated between the average of measurements by the 3 examiners using the mobile application and the measurements obtained using the 3D CT images.
The intraclass correlation coefficient (ICC) was used to assess interobserver reliability by the 3 examiners.
Statistical Analysis
Prior sample size estimation was performed to determine the minimum number of patients required for testing reliability. The minimum sample size for interobserver reliability was calculated as 36 hips by setting the ICC at a target value of 0.8 and the 95% confidence interval (CI) as 0.2 with a Bonett approximation.18 A single hip in each patient was selected by block randomization and included in the statistical analysis to achieve statistical independence.19
The Pearson correlation coefficients were used to determine the validity for measuring femoral anteversion using the mobile application. The Pearson correlation coefficient was characterized as poor (0.00 to 0.20), fair (0.21 to 0.40), moderate (0.41 to 0.60), good (0.61 to 0.80), or excellent (0.81 to 1.00).
ICCs and 95% CIs were used to summarize the interobserver reliability and were calculated with the use of a 2-way random effect model assuming a single measurement and absolute agreement. An ICC of 1 indicates perfect reliability and an ICC>0.8 indicates excellent reliability.20
Statistical analysis was conducted using the SPSS software for Windows (version 22.0; SPSS Inc., Chicago, IL), and null hypotheses of no difference were rejected if P-values <0.05.
RESULTS
The mobile application, which reconstructs the 3D image from conventional radiographs, was successfully developed. The AP and LAT radiographs of the entire femur for each patient are displayed on the monitor using a DICOM viewer. The user is required to take photographs of the displayed images using the capture function of the application. The application shows the captured images on the iPad screen, and the user is required to segment the contour of the femur from the images using the touch interface. After that, the application automatically calibrates the captured images because the AP and LAT radiographs are not orthogonal in the conventional radiographic system. The shape of the SSM is also optimized automatically. More specifically, the contours of the SSM in the AP and LAT views are virtually projected onto the captured images. Both calibration and shape optimization minimizes the difference between the projected contours and the contours segmented by the user. The reconstructed shape is the best estimate of all possible shapes that the SSM can generate in a sense that the projected contours are best aligned with the segmented contours. The reconstruction process for measuring femoral anteversion using this application takes <5 minutes (Video Supplement 2, Supplemental Digital Content 2, http://links.lww.com/BPO/A246).
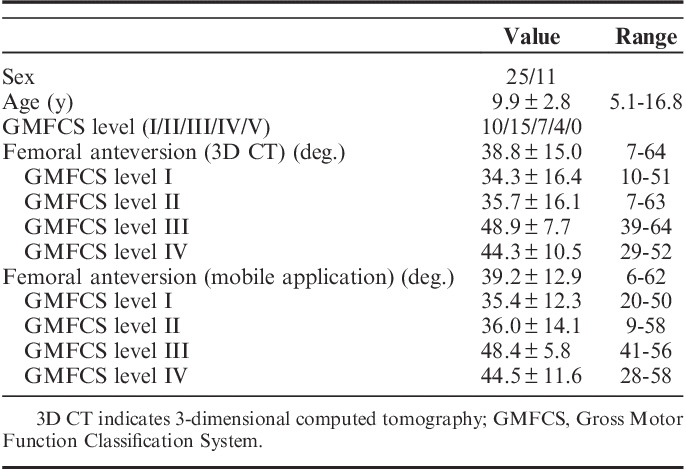
The images of the hips of 36 patients (36 hips including 18 right hips and 18 left hips) with CP were included in the validation study (Table 1).
TABLE 1.
Patients’ Demographics and Summary of Measurement
The correlation coefficient between femoral anteversion measured using 3D CT and mobile application was 0.968 (P<0.001) (Fig. 2). The Bland-Altman plot of the femoral anteversion measurement using 3D CT and the mobile application is shown in Figure 3. The mean angle difference between the 2 methods was 3.0±2.9 degrees (range, 0.3 to 11.0 degrees). The difference between the 2 methods was >5 degrees in 5 hips and >10 degrees in 1 hip.
FIGURE 2.
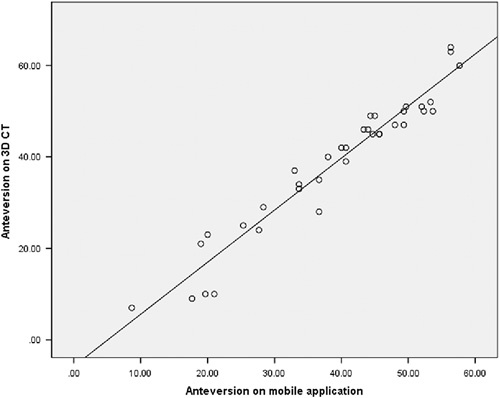
Scatter plot illustrating the relationship between femoral anteversion as measured on 3D computed tomographic (CT) images and that measured using the reconstructed images from the mobile application.
FIGURE 3.
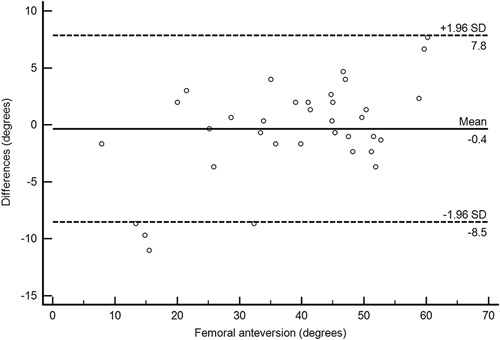
Bland-Altman plots of the femoral anteversion measurements using 3D computed tomography and the mobile application.
Measuring femoral anteversion using the mobile application showed excellent interobserver reliabilities (ICC, 0.953; 95% CI, 0.917-0.975).
DISCUSSION
The newly developed mobile application can reconstruct 3D images of the femur from conventional radiographs. It showed excellent convergent validity and interobserver reliability.
This study has some limitations. First, the validity of the application in this study is confined to the measurements of femoral anteversion. The SSM uses the principal component analysis or singular value decomposition. Consequently, it has inherent limitations in reconstructing femur shapes of different kinds. That is, it can cover only the variance of the principal component or shape deformities such as torsion, bowing, or bending. In other words, it is difficult to reconstruct the various fracture patterns using the SSM. Therefore, to validate the other uses of this application, further validation with a specific purpose will be needed. However, this is not only true for this application but also all other apparatus using the SSM such as EOS. Second, the iPad fourth generation was used for the validation study. However, the application can be used in a variety of smartphones and tablets. This can lead to difference in measurements due to the disparity in reliability and validity among different devices. Third, the application only covers the femur. The 3D reconstruction of the tibia and spine need to be developed in future studies.
CT measurement of lower-limb torsional alignment has been well validated and is widely used as a current reference standard.6,21 However, population irradiation from medical sources has been rising quite substantially and CT scans are largely responsible for this increase.7,22,23 A low-dose biplanar x-ray technology (EOS; EOS Imaging) was developed for 3D reconstruction of the lower extremity and spine. Several studies have demonstrated that the EOS system showed excellent concurrent validity and reliability for femoral anteversion and tibial torsion measurements12–16 (Table 2). However, the EOS system is not appropriate for use in some hospitals and countries because of its high cost, requirement for another apparatus, and space constraints.
TABLE 2.
Previous Study Regarding Validity and Reliability of EOS System for Measuring Femoral Anteversion
The radiation dose from the EOS imaging system has been reported to be much less than that from the CT scan. Folinais et al16 showed that the mean radiation dose from the EOS system was 0.18 mGy for the AP view and 0.45 mGy for the LAT view, and that from CT scan was 8.4 to 15.6 mGy. Delin et al24 found that the EOS system provided lower-limb torsional alignment at a radiation dose reduced 4 to 30 times from that of 16-slice CT scan. In addition, Deschenes et al25 showed that full-spine EOS imaging delivered 6 to 9 times less radiation dose than conventional radiography. However, Faria et al11 showed that the health benefits from radiation dose reduction with the use of the EOS system was unremarkable in terms of cost-effectiveness.
The mobile application newly developed in this study has some advantages over the EOS system. First, the application only requires mobile devices and conventional radiographs to visualize a 3D image of the femur. However, the validity and reliability of this method are comparable to those of EOS. Second, the accuracy of the 3D reconstruction with the SSM depends on the subjects used therein. The range of femoral anteversion is limited in the SSM as it uses only typical or healthy subjects. However, the mobile application was developed from an SSM using 54 CP patients who showed substantial variation in femoral anteversion and coxa valga.17 The mobile application, therefore, could cover anteversion from 6 to 62 degrees in this study. Third, to the best of our knowledge, there has been no study investigating the validity and reliability of the EOS system in CP patients with severe deformity of the proximal femur. Fourth, the use of the EOS system requires patients to stand still for 10 seconds.16 Most patients with Gross Motor Function Classification System level IV to V and some with Gross Motor Function Classification System level III are therefore not suitable candidates for EOS imaging. However, our application needs only the AP and LAT radiograph with patient in any position.
In conclusion, the measurement of femoral anteversion with the mobile application showed excellent validity and reliability in patients with CP. Furthermore, the newly developed mobile application can be easily used with conventional radiographic equipment, and incorporated into existing clinical protocols. Therefore, anyone with a smartphone or tablet can reconstruct the 3D femur shapes in their hospitals without any additional apparatus. We believe that the newly developed mobile application in this study is an appropriate technology for assessing femoral anteversion. In the future, we expect to expand the application for use in 3D reconstruction of the tibia and spine.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.pedorthopaedics.com.
Footnotes
K.H.S. and K.Y. contributed equally.
M.S.P. and J.L. are co-corresponding authors.
Supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (No.NRF-2017R1A2B4007412), the Ministry of SMEs and Startups (grant no. S2566948) and the SNUBH Research Fund (grant no. 13-2017-005).
The authors declare no conflicts of interest.
REFERENCES
- 1.Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005;47:571–576. [DOI] [PubMed] [Google Scholar]
- 2.Robin J, Graham HK, Selber P, et al. Proximal femoral geometry in cerebral palsy: a population-based cross-sectional study. J Bone Joint Surg Br. 2008;90:1372–1379. [DOI] [PubMed] [Google Scholar]
- 3.Wren TA, Rethlefsen S, Kay RM. Prevalence of specific gait abnormalities in children with cerebral palsy: influence of cerebral palsy subtype, age, and previous surgery. J Pediatr Orthop. 2005;25:79–83. [DOI] [PubMed] [Google Scholar]
- 4.Dreher T, Wolf S, Braatz F, et al. Internal rotation gait in spastic diplegia—critical considerations for the femoral derotation osteotomy. Gait Posture. 2007;26:25–31. [DOI] [PubMed] [Google Scholar]
- 5.Sung KH, Kwon SS, Chung CY, et al. Long-term outcomes over 10 years after femoral derotation osteotomy in ambulatory children with cerebral palsy. Gait Posture. 2018;64:119–125. [DOI] [PubMed] [Google Scholar]
- 6.Chung CY, Lee KM, Park MS, et al. Validity and reliability of measuring femoral anteversion and neck-shaft angle in patients with cerebral palsy. J Bone Joint Surg Am. 2010;92:1195–1205. [DOI] [PubMed] [Google Scholar]
- 7.Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. [DOI] [PubMed] [Google Scholar]
- 8.Schneider B, Laubenberger J, Jemlich S, et al. Measurement of femoral antetorsion and tibial torsion by magnetic resonance imaging. Br J Radiol. 1997;70:575–579. [DOI] [PubMed] [Google Scholar]
- 9.Dubousset J, Charpak G, Dorion I, et al. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med. 2005;189:287–297; discussion 297–300. [PubMed] [Google Scholar]
- 10.Chaibi Y, Cresson T, Aubert B, et al. Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Engin. 2012;15:457–466. [DOI] [PubMed] [Google Scholar]
- 11.Faria R, McKenna C, Wade R, et al. The EOS 2D/3D X-ray imaging system: a cost-effectiveness analysis quantifying the health benefits from reduced radiation exposure. Eur J Radiol. 2013;82:e342–e349. [DOI] [PubMed] [Google Scholar]
- 12.Buck FM, Guggenberger R, Koch PP, et al. Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements. AJR Am J Roentgenol. 2012;199:W607–W612. [DOI] [PubMed] [Google Scholar]
- 13.Rosskopf AB, Ramseier LE, Sutter R, et al. Femoral and tibial torsion measurement in children and adolescents: comparison of 3D models based on low-dose biplanar radiography and low-dose CT. AJR Am J Roentgenol. 2014;202:W285–W291. [DOI] [PubMed] [Google Scholar]
- 14.Pomerantz ML, Glaser D, Doan J, et al. Three-dimensional biplanar radiography as a new means of accessing femoral version: a comparitive study of EOS three-dimensional radiography versus computed tomography. Skeletal Radiol. 2015;44:255–260. [DOI] [PubMed] [Google Scholar]
- 15.Thepaut M, Brochard S, Leboucher J, et al. Measuring physiological and pathological femoral anteversion using a biplanar low-dose X-ray system: validity, reliability, and discriminative ability in cerebral palsy. Skeletal Radiol. 2016;45:243–250. [DOI] [PubMed] [Google Scholar]
- 16.Folinais D, Thelen P, Delin C, et al. Measuring femoral and rotational alignment: EOS system versus computed tomography. Orthop Traumatol Surg Res. 2013;99:509–516. [DOI] [PubMed] [Google Scholar]
- 17.Park N, Lee J, Sung KH, et al. Design and validation of automated femoral bone morphology measurements in cerebral palsy. J Digit Imaging. 2014;27:262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21:1331–1335. [DOI] [PubMed] [Google Scholar]
- 19.Park MS, Kim SJ, Chung CY, et al. Statistical consideration for bilateral cases in orthopaedic research. J Bone Joint Surg Am. 2010;92:1732–1737. [DOI] [PubMed] [Google Scholar]
- 20.Lee KM, Lee J, Chung CY, et al. Pitfalls and important issues in testing reliability using intraclass correlation coefficients in orthopaedic research. Clin Orthop Surg. 2012;4:149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abel MF, Sutherland DH, Wenger DR, et al. Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop. 1994;14:48–53. [DOI] [PubMed] [Google Scholar]
- 22.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361:849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mettler FA, Jr, Bhargavan M, Faulkner K, et al. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources—1950-2007. Radiology. 2009;253:520–531. [DOI] [PubMed] [Google Scholar]
- 24.Delin C, Silvera S, Bassinet C, et al. Ionizing radiation doses during lower limb torsion and anteversion measurements by EOS stereoradiography and computed tomography. Eur J Radiol. 2014;83:371–377. [DOI] [PubMed] [Google Scholar]
- 25.Deschenes S, Charron G, Beaudoin G, et al. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976). 2010;35:989–994. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.pedorthopaedics.com.