Abstract
Although residential environment might be an important predictor of depression among older adults, systematic reviews point to a lack of longitudinal investigations, and the generalizability of the findings is limited to a few countries. We used longitudinal data collected between 2012 and 2017 in 3 surveys including 15 European countries and the United States and comprising 32,531 adults aged 50 years or older. The risk of depression according to perceived neighborhood disorder and lack of social cohesion was estimated using 2-stage individual-participant-data meta-analysis; country-specific parameters were analyzed by meta-regression. We conducted additional analyses on retired individuals. Neighborhood disorder (odds ratio (OR) = 1.25) and lack of social cohesion (OR = 1.76) were significantly associated with depression in the fully adjusted models. In retirement, the risk of depression was even higher (neighborhood disorder: OR = 1.35; lack of social cohesion: OR = 1.93). Heterogeneity across countries was low and was significantly reduced by the addition of country-level data on income inequality and population density. Perceived neighborhood problems increased the overall risk of depression among adults aged 50 years or older. Policies, especially in countries with stronger links between neighborhood and depression, should focus on improving the physical environment and supporting social ties in communities, which can reduce depression and contribute to healthy aging.
Keywords: cohort studies, depression, mental health, meta-analysis, multicenter studies, residence characteristics
Abbreviations
- CES-D
Center for Epidemiologic Studies Depression
- CI
confidence interval
- ELSA
English Longitudinal Study of Ageing
- HRS
Health and Retirement Study
- IPD
individual participant data
- OR
odds ratio
- SHARE
Survey of Health, Ageing and Retirement in Europe
Depression is one of the leading causes of disability worldwide, affecting 1 out of 5 individuals during their lifetime (1), and it is associated with a large economic burden (2). Approximately 13.5% of people over the age of 50 years suffer from clinically relevant depressive symptoms (3), and this percentage rises dramatically among the oldest old (age ≥80 years) (4). Because of global aging, the number of people older than 65 years is expected to grow almost 3-fold by 2050 (5), which will significantly increase the disease burden related to depression. These processes present a range of challenges for social, economic, and health-care systems and require age-specific adaptations to support healthy aging (6).
In aging individuals, psychosocial and health-related determinants become more prominent risk factors for the incidence (7) and recurrence (8) of depression. Because of increasing morbidity, functional decline, and life-course transitions (e.g., retirement), older people tend to spend more time in their local area, which affects the pathways through which physical and social characteristics influence their social and psychological well-being (6, 9). Exposure to adverse neighborhood conditions, such as vandalism, crime, littering, and heavy traffic, have been found to increase the risk of depression through direct and indirect pathways (10, 11), while social cohesion or social capital buffers individual distress and weakens the risk of depression (12, 13).
Although there is a growing body of literature on neighborhoods and mental health, relatively few studies have assessed the longitudinal associations for this age group (9), and evidence is based on a low number of (mainly Anglo-Saxon) economies, limiting the generalizability of the findings. Examining the evidence of possible neighborhood effects in different settings will provide further insights into the public health significance of the residential environment. In addition, the inclusion of several countries enables the consideration of between-country heterogeneity in neighborhood effects. Although previous studies have shown that the prevalence of depression (14) and its association with social inequality (15) differs by welfare regime (i.e., typology indicating how states manage their economies and provide social protection and income transfers; originally introduced by Esping-Andersen (16)), there is no evidence of differential neighborhood effects. Moreover, because micro- and meso-level social and environmental factors (e.g., population density, green space, air pollution) have been previously associated with mental health and also interact with each other (9), it is feasible that they will modify neighborhood effects on mental health between countries. An understanding of how country-level social, environmental, or welfare-state differences influence the link between neighborhood and mental health can help in prioritizing public health policies and interventions at the national level.
Our primary aims in this individual-participant-data (IPD) meta-analysis were the following. First, we examined the longitudinal associations (2 years) of perceived neighborhood disorder and social cohesion with depressive symptoms among adults aged 50 years or older, estimating the risk in a wide range of European and North American countries. Second, using meta-regression, we explored effect modification by type of welfare regime and other macro-level social or environmental indicators in the country-specific neighborhood effects. In a secondary analysis, we investigated the robustness of our findings for retired individuals, a subgroup for whom we assumed that there would be stronger associations than in the general sample, since this group tends to spend more time in a residential environment.
METHODS
Data sources
Data were drawn from 3 representative longitudinal panel surveys of aging adults: the English Longitudinal Study of Ageing (ELSA) (17), the Health and Retirement Study (HRS) (18), and the Survey of Health, Ageing and Retirement in Europe (SHARE) (19). All of the studies have comparable designs and contain information on noninstitutionalized community-dwelling adults aged 50 years or over (51 years for HRS (18)), as well as details on their partners, irrespective of their age. Participants are followed up approximately every 2 years, with regular refreshment samples being added to compensate for attrition bias and to balance the age structure. The initial HRS cohort was recruited in the United States in 1992 (20) and served as an exemplar for subsequent aging studies. ELSA, with a representative sample for England, was set up in 2002 (17). The first wave of SHARE was conducted in 2004/2005, and the most recent wave was conducted in 2015; it includes 17 European countries and Israel (19). ELSA, HRS, and SHARE data are harmonized, allowing cross-national comparisons.
Our analytical sample comprised individuals who provided valid measurements of depression at 2 consecutive study waves and answered at least 1 question on perceived neighborhood characteristics at the baseline wave. We excluded participants if they had depression at baseline, were living in a nursing home, were younger than 50 years, moved to a new residential address between baseline and follow-up, or had missing values for baseline covariates. Because data on the neighborhood were not usually collected in all waves, we used the most recently available sweeps in compliance with our criteria: for ELSA, wave 7 (2014/2015) and wave 8 (2016/2017); for SHARE, wave 5 (2013) and wave 6 (2015). In the HRS, since 2006 approximately 50% of the sample has been selected for an enhanced face-to-face interview, while the other half is interviewed via telephone; the survey mode alternates in each wave. Neighborhood perception is part of the psychosocial questionnaire, which is administered after the face-to-face interviews, once every 4 years for the same person (18). Therefore, in order to have information for the entire HRS sample, we extracted exposure data from 2 consecutive waves (wave 11 in 2012 and wave 12 in 2014) and linked them with matching follow-ups (wave 12 in 2014 and wave 13 in 2016). The rates of attrition between baseline and follow-up were 16% for ELSA, 12% and 16% for the 2 HRS subsamples, and 15% (Switzerland) to 32% (Luxemburg) in SHARE.
Neighborhood
For the measures of perceived neighborhood disorder and lack of social cohesion, we used 4 similarly operationalized items asking participants about the “local area, that is, everywhere within a 20-minute walk or about a mile [kilometer in SHARE] of your home.” Neighborhoods were assessed in ELSA and HRS on a 7-point bipolar scale in the self-completion part of the questionnaire, while SHARE applied a 4-point Likert scale in the interview denoting agreement or disagreement with the opposing statement. A priori, we assigned 2 items to the neighborhood disorder domain, capturing information on 1) vandalism and crime/graffiti and 2) the cleanliness of the area. Lack of social cohesion included items on 1) feeling part of the area and 2) receiving help if in trouble. Principal components analysis did not confirm the 2-component structure but indicated 1 underlying score, which provided satisfying internal consistency (Cronbach’s α = 0.57–0.82). In order to make neighborhood variables comparable across studies, we first dichotomized scores for all items (SHARE: 0–1 vs. 2–3; ELSA and HRS: 0–3 vs. 4–6) to obtain similar response patterns between cohorts. Scales were computed by calculating the average value of the respective items, which ranged between 0 and 1, with higher numbers indicating more problems and less cohesion in the residential area.
Depression
Depressive symptoms were assessed with 2 self-report symptom scales: the Center for Epidemiologic Studies Depression (CES-D) Scale (21) and the EURO-D Scale (22). The CES-D was implemented in ELSA and HRS, and the EURO-D was implemented in SHARE. The original CES-D Scale, containing 20 items, was developed to detect depressive symptomatology in the general population during the week preceding the interview (21). In ELSA and HRS, a short version of the CES-D was used, with 8 items asking respondents whether (in the past week) they had felt depressed, felt that everything was an effort, had restless sleep, were happy, were lonely, enjoyed life, felt sad, or could not get going. The EURO-D Scale consists of 12 items measuring the presence of depression, pessimism, wishing for death, guilt, sleep, interest, irritability, appetite, fatigue, concentration, enjoyment, and tearfulness in the last month (22). Both scales have high internal consistency and test-retest reliability, provide a valid measurement of depression, and show high correlation within the same population (22, 23). Binary answers, indicating the presence or absence of depressive symptoms, were summed, with increasing scores indicating higher levels of depressive symptoms. For approximation of a clinically significant level of depressive symptoms, a cutoff score of ≥3 was applied for CES-D (23) and a cutoff score of ≥4 was applied for the EURO-D (22, 23); these thresholds were also used in a recent comparative study (24).
Baseline covariates
We adjusted for several sociodemographic and health-related confounders measured at baseline that were relevant to the neighborhood-depression association (10, 12, 25, 26). In addition to sex (male, female), age (because of a nonlinear relationship with depression, this variable was categorized as 50–59, 60–69, 70–79, and ≥80 years), and immigration (born in the country of interview or not), we included 3 indicators of socioeconomic status: educational attainment, total equalized household net wealth, and economic activity. For education, we used the International Standard Classification of Education classification (27) from the harmonized data sets and grouped the highest educational attainment into 3 categories: primary (levels 0 and 1), secondary (levels 2–4), and tertiary (levels 5 and 6). Household nonpension net wealth included financial, physical, and housing wealth after all debt had been subtracted. We calculated an equalized measure by dividing the household sum by the square root of benefiting members (28) and categorized it into country-specific tertiles (low, medium, or high wealth). Economic activity described whether the respondent was working (employed, self-employed), retired, or out of the labor force (homemaker, unemployed, permanently sick or disabled). We included information on partnership (married or cohabiting vs. neither) and on current smoking (yes, no). A binary variable described whether the respondent reported at least 2 out of 7 physician-diagnosed chronic diseases or conditions (arthritis, cancer, cardiovascular disease, diabetes, high blood pressure, lung disease, and stroke). Finally, a measure of functional limitations indicated whether the respondent had at least 1 disability affecting Activities of Daily Living or Instrumental Activities of Daily Living (29).
Figure 2.
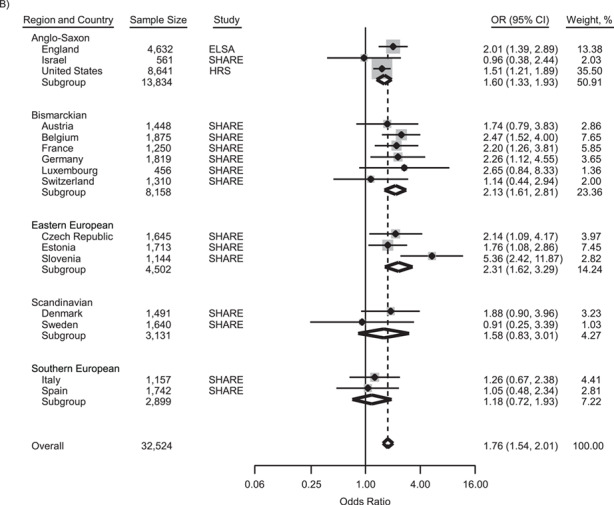
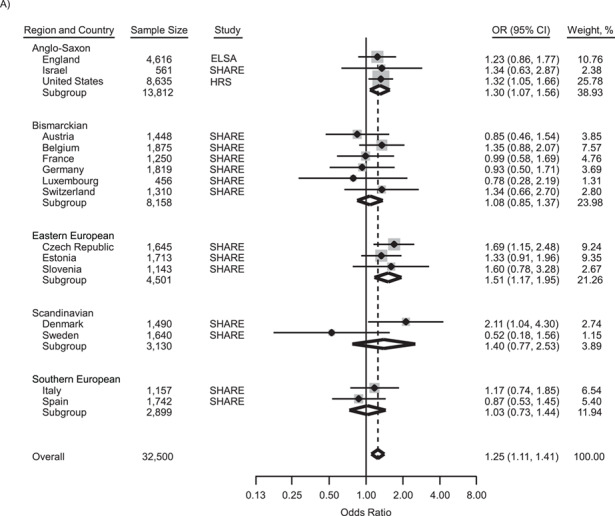
Country-specific and pooled associations of A) perceived neighborhood disorder and B) perceived lack of social cohesion with depression among adults aged 50 years or older in 16 high-income countries, 2012–2017. Results were adjusted for age, sex, country of birth, education, wealth, economic activity, partnership status, current smoking, chronic diseases or conditions, and functional limitations. Countries are grouped by type of welfare regime. The size of each gray square is proportional to the relative weight of the sample in the meta-analysis; diamonds represent the pooled estimates. Odds ratios (ORs) greater than 1 indicate increased risk of depression, while ORs less than 1 indicate decreased risk. The overall I2 values were 0.0% (P = 0.53) for perceived neighborhood disorder and 23.7% (P = 0.19) for perceived lack of social cohesion. Bars, 95% confidence intervals (CIs). ELSA, English Longitudinal Study of Ageing; HRS, Health and Retirement Study; SHARE, Survey of Health, Ageing and Retirement in Europe.
Country-level indicators
Countries were grouped into 5 types of welfare regimes based on an expanded classification (15) of Ferrera’s typology (30), which is considered a state-of-the-art typology and is often used in cross-national surveys (15). The 1) Scandinavian welfare regimes (Denmark, Sweden) are described as having universal coverage and generous social transfers; the 2) Bismarckian regimes (Austria, Belgium, France, Germany, Luxembourg, Switzerland) have earnings-related benefits administered by the employer and familialism; the 3) Anglo-Saxon regimes (England, Israel, United States) have minimum welfare provisions and a strong emphasis on the market (15); the 4) Southern European regimes (Italy, Spain) are characterized as “rudimentary,” with services ranging from generous to limited and with high reliance on the family (15, 30); and the 5) Eastern European regimes consist of postcommunist countries (Czech Republic, Estonia, Slovenia) which have experienced shifts towards marketization from more universalist communist welfare states (15).
Macro-level social and environmental indicators were extracted from the World Bank Database (31) for the closest year of data collection (see Web Table 1, available at https://academic.oup.com/aje): gross domestic product at purchasing power parity per capita (in current international dollars), Gini index of income inequality (32), population density (number of people per km2), urbanization rate (percentage of the population that is urban), forest coverage (percentage of land area), and annual mean air pollution level (particulate matter less than or equal to 2.5 μm in diameter, measured in μg/m3). Before including these variables in the models, we standardized all external raw data. Correlations between indicators are shown in Web Table 2.
Statistical analysis
We conducted a 2-stage IPD meta-analysis to estimate the overall associations between perceived neighborhood characteristics and depression (33). First, we fitted separate logistic regression models for each country, including perceived neighborhood characteristics as a continuous independent variable, to obtain odds ratios for depression with 95% confidence intervals. Second, we derived effect estimates and their variance and pooled them using meta-analysis. Heterogeneity between countries was quantified with the I2 statistic, indicating the percentage of variance explained by individual countries (34). Because the heterogeneity was low (I2 < 25%), we fitted fixed-effects models with inverse variance pooling, assuming a single underlying true association across countries (33). We present results from 2 sets of models: The first set of models controlled for age and sex, and the second set adjusted for all confounders (age, sex, country of birth, education, wealth, economic activity, partnership status, current smoking, chronic diseases or conditions, and functional limitations). Prior to the main analyses, we tested the linearity assumption by imputing neighborhood variables in categorical form into the models, which was confirmed by the stepwise increasing gradients. Interaction models did not reveal significantly different neighborhood associations among male and female participants; therefore, no sex-stratified results were prepared.
Although heterogeneity was relatively low, we still examined whether between-country variation in the risk estimates might be explained by sample (sample size, percentage of female participants) or country (e.g., welfare regime, Gini index, air pollution) characteristics. We first retained log odds and their standard errors from the fully adjusted logistic models and then performed univariable random-effects meta-regression. Models were fitted by the restricted maximum likelihood method and corrected with the Hartung-Knapp variance estimator.
Because multicenter studies can be analyzed in various ways (35), in the sensitivity analyses we derived risk estimates pooled by 1) 2-stage IPD with random-effects models and estimated with 2) 1-stage IPD with random intercepts (multilevel logistic models) and 3) 1-stage IPD with fixed country effects (logistic models). Although we expected only small differences (33), we report results from the 2-stage IPD meta-analysis as the main results, because in multilevel models at least 30 countries would be required to accurately estimate the country-level parameters (36). Findings on neighborhood disorder and lack of social cohesion are presented in the Results section of the text, while findings from analyses of the composite neighborhood problems score are shown in the Web material (Web Tables 3 and 4, Web Figure 1). We provide stage 1 results of the IPD meta-analysis (i.e., covariate-adjusted logistic models by country) for the composite neighborhood problems score in Web Table 3.
All analyses were performed using STATA 13 (StataCorp LLC, College Station, Texas).
RESULTS
After application of all inclusion and exclusion criteria (Figure 1), the pooled analytical sample contained 32,531 participants from 16 countries: Austria (n = 1,448), Belgium (n = 1,875), the Czech Republic (n = 1,645), Denmark (n = 1,491), England (n = 4,634), Estonia (n = 1,713), France (n = 1,250), Germany (n = 1,819), Israel (n = 561), Italy (n = 1,157), Luxemburg (n = 456), Slovenia (n = 1,144), Spain (n = 1,742), Sweden (n = 1,640), Switzerland (n = 1,310), and the United States (n = 8,646). Table 1 shows the characteristics of study participants by survey. For the total sample, 55.3% were female, and the mean age was 66.7 years. Over half of the sample (56.8%) was retired at the time of data collection. Although household wealth was defined in terms of 3 equally large categories within countries, in the analytical data set there was underrepresentation of individuals from the low wealth group, partly because of censoring of depression cases at baseline. After 2 years, the incidence of depression was 13.2%, with large variation by country (P < 0.001), ranging between 8.1% (Denmark) and 22.7% (Estonia).
Figure 1.
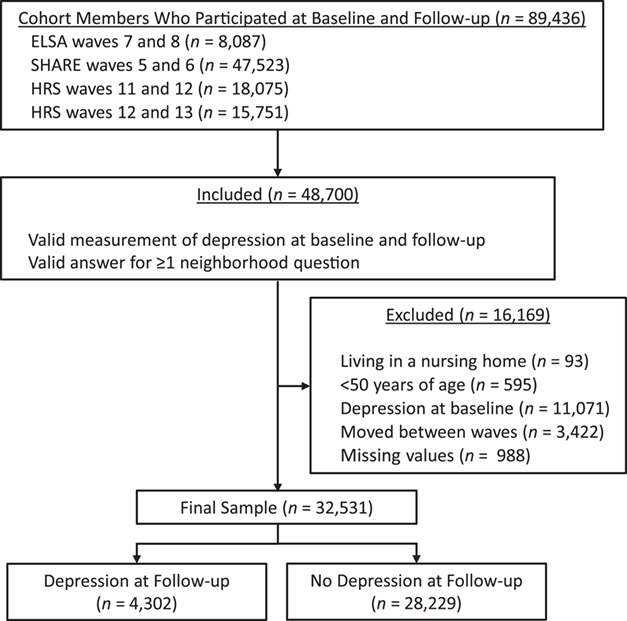
Selection of participants from 3 studies (the English Longitudinal Study of Ageing (ELSA), the Health and Retirement Study (HRS), and the Survey of Health, Ageing and Retirement in Europe (SHARE)) for a pooled data set on neighborhood perception and depression. The pooled data set contained information assessed in 16 different countries between 2012 and 2017. Note that the HRS collects information on neighborhood perception from half of the sample in each study wave. Because the survey mode alternates between waves, we extracted and merged data from both subsamples.
Table 1.
Baselinea and Follow-upb Characteristics (%c) of Adults Aged 50 Years or Older (n = 32,531) From 3 Surveys Included in a Study of Neighborhood Perception and Depression, 2012–2017
| Characteristic | Survey | Pooled Data | ||
|---|---|---|---|---|
| ELSA (n = 4,634) | HRS (n = 8,646) | SHARE (n = 19,251) | ||
| Sex | ||||
| Male | 46.3 | 42.0 | 45.5 | 44.7 |
| Female | 53.7 | 58.0 | 54.5 | 55.3 |
| Age group, years | ||||
| 50–59 | 18.2 | 26.2 | 28.4 | 26.4 |
| 60–69 | 43.3 | 30.2 | 37.1 | 36.1 |
| 70–79 | 29.1 | 31.1 | 24.8 | 27.1 |
| ≥80 | 9.3 | 12.6 | 9.7 | 10.4 |
| Country of birth | ||||
| Born in country of interview | 94.1 | 88.6 | 89.5 | 89.9 |
| Born outside country of interview | 5.9 | 11.4 | 10.5 | 10.1 |
| Educational attainment | ||||
| Primary (ISCED levels 0 and 1) | 19.2 | 12.8 | 17.3 | 16.4 |
| Secondary (ISCED levels 2–4) | 46.2 | 60.1 | 55.9 | 55.6 |
| Tertiary (ISCED levels 5 and 6) | 34.6 | 27.1 | 26.8 | 28.0 |
| Tertile of equalized household wealth | ||||
| Low | 26.1 | 22.4 | 30.8 | 27.9 |
| Medium | 35.7 | 36.2 | 33.4 | 34.5 |
| High | 38.2 | 41.4 | 35.8 | 37.6 |
| Economic activity | ||||
| Employed | 30.4 | 35.4 | 29.6 | 31.3 |
| Retired | 62.6 | 49.7 | 58.7 | 56.8 |
| Out of labor force | 7.0 | 14.9 | 11.7 | 11.9 |
| Partnership status | ||||
| In a couple | 77.1 | 68.5 | 63.9 | 67.0 |
| Alone | 22.9 | 31.5 | 36.1 | 33.0 |
| Current smoking | ||||
| No | 91.6 | 89.5 | 82.8 | 85.9 |
| Yes | 8.4 | 10.5 | 17.2 | 14.1 |
| No. of chronic diseases or conditions | ||||
| <2 | 76.9 | 41.5 | 76.3 | 67.2 |
| ≥2 | 23.1 | 58.5 | 23.7 | 32.8 |
| No. of ADL/IADL functional limitations | ||||
| 0 | 83.4 | 90.6 | 90.7 | 89.6 |
| ≥1 | 16.6 | 9.4 | 9.3 | 10.4 |
| Neighborhood disorderd,e | 0.13 (0.004) | 0.12 (0.003) | 0.15 (0.002) | 0.14 (0.002) |
| Lack of social cohesiond,f | 0.09 (0.003) | 0.13 (0.003) | 0.08 (0.001) | 0.09 (0.001) |
| Composite neighborhood scored,g | 0.11 (0.003) | 0.13 (0.003) | 0.11 (0.001) | 0.12 (0.001) |
| Depression at follow-uph | ||||
| Yes | 10.4 | 10.4 | 15.2 | 13.2 |
| No | 89.6 | 89.6 | 84.8 | 86.8 |
Abbreviations: ADL, Activities of Daily Living; ELSA, English Longitudinal Study of Ageing; HRS, Health and Retirement Study; IADL, Instrumental Activities of Daily Living; ISCED, International Standard Classification of Education; SHARE, Survey of Health, Ageing and Retirement in Europe.
a Baseline measures: ELSA, 2014/2015; HRS, 2012 and 2014; SHARE, 2013.
b Follow-up measures: ELSA, 2016/2017; HRS, 2014 and 2016; SHARE, 2015.
c Percentages may not sum to 100 because of rounding.
d Values are expressed as mean (standard error).
e The neighborhood disorder measure captured perceived 1) vandalism and crime/graffiti and 2) cleanliness of the residential area; values ranged between 0 and 1.
f Lack of social cohesion included 1) not feeling part of the neighborhood and 2) not receiving help if in trouble; values ranged between 0 and 1.
g The composite neighborhood score comprised all 4 perceived neighborhood characteristics; values ranged between 0 and 1.
The IPD meta-analyses models showed significantly elevated odds ratios for clinically relevant depressive symptoms by neighborhood disorder (odds ratio (OR) = 1.44, 95% confidence interval (CI): 1.28, 1.61) and lack of social cohesion (OR = 1.99, 95% CI: 1.75, 2.26) after adjustment for sex and age (Web Figure 2). In the fully adjusted models (Figure 2), the pooled odds ratio for neighborhood disorder was 1.25 (95% CI: 1.11, 1.41), with individual odds ratios ranging between 0.52 and 2.11 and significantly higher than 1 in the Czech Republic, Denmark, and the United States. Lack of social cohesion had a pooled odds ratio of 1.76 (95% CI: 1.54, 2.01), with individual odds ratios ranging from 0.91 to 5.36 and significantly elevated in Belgium, the Czech Republic, Estonia, France, Germany, Slovenia, England, and the United States. Meta-regression indicated stronger associations between lack of social cohesion and depression in more equal countries (β = −0.174, P = 0.01), as measured by Gini index. Furthermore, there was a tendency for associations between lack of social cohesion and depression to be stronger in countries with higher levels of air pollution (β = 0.152, P = 0.09) (Table 2).
Figure 2.
Continues.
Table 2.
Associations of Perceived Neighborhood Disorder and Lack of Social Cohesion With Depression in 16 High-Income Countries (Meta-Regression Analysis), 2012–2017
| Country-Level Indicator a | Neighborhood Disorder b | Lack of Social Cohesion c | ||||
|---|---|---|---|---|---|---|
| β | SE | P Value | β | SE | P Value | |
| Age 50 Years or Older | ||||||
| Sample size (no. of individuals) | 0.021 | 0.038 | 0.60 | −0.059 | 0.047 | 0.23 |
| % of female participants | 0.098 | 0.060 | 0.13 | −0.044 | 0.094 | 0.65 |
| GDP PPP per capita, CID | −0.065 | 0.088 | 0.47 | −0.052 | 0.128 | 0.69 |
| Gini index of income inequalityd | −0.026 | 0.054 | 0.64 | −0.174 | 0.061 | 0.01 |
| Population density (no. of people/km2) | 0.002 | 0.059 | 0.97 | 0.089 | 0.073 | 0.24 |
| % of population that is urban | 0.016 | 0.074 | 0.84 | −0.064 | 0.104 | 0.55 |
| % of forest coverage | −0.062 | 0.080 | 0.45 | 0.055 | 0.110 | 0.63 |
| Air pollution (PM2.5 level), μg/m3 | 0.044 | 0.062 | 0.49 | 0.152 | 0.083 | 0.09 |
| In Retirement | ||||||
| Sample size (no. of individuals) | 0.054 | 0.056 | 0.35 | −0.097 | 0.063 | 0.15 |
| % of female participants | 0.084 | 0.083 | 0.33 | −0.186 | 0.121 | 0.15 |
| GDP PPP per capita, CID | 0.061 | 0.114 | 0.60 | −0.003 | 0.158 | 0.99 |
| Gini index of income inequality | 0.019 | 0.070 | 0.79 | −0.188 | 0.082 | 0.04 |
| Population density (no. of people/km2) | 0.044 | 0.078 | 0.58 | 0.194 | 0.087 | 0.04 |
| % of population that is urban | 0.133 | 0.094 | 0.18 | 0.096 | 0.123 | 0.45 |
| % of forest coverage | −0.175 | 0.099 | 0.10 | −0.102 | 0.125 | 0.43 |
| Air pollution (PM2.5 level), μg/m3 | 0.038 | 0.078 | 0.64 | 0.205 | 0.102 | 0.07 |
Abbreviations: CID, current international dollars; GDP PPP, gross domestic product at purchasing power parity; PM2.5, particulate matter less than or equal to 2.5 μm in diameter; SE, standard error.
a Raw data were standardized before meta-regression.
b Associations between neighborhood disorder and depression did not differ by welfare regime (individuals aged ≥50 years: F(4, 11) = 1.29, P = 0.33; retired individuals: F(4, 11) = 1.18, P = 0.37).
c Associations between lack of social cohesion and depression did not differ by welfare regime (individuals aged ≥50 years: F(4, 11) = 1.73, P = 0.21; retired individuals: F(4, 11) = 0.71, P = 0.60).
d Scores on the Gini index can range from 0 to 100, with higher numbers indicating more inequality (32).
We repeated the analyses for retired individuals. In the sex- and age-adjusted models, neighborhood disorder had an odds ratio of 1.48 (95% CI: 1.28, 1.71), while the odds ratio for lack of social cohesion was 2.06 (95% CI: 1.73, 2.45) (Web Figure 3). Although the pooled odds ratios decreased after adjustment for all covariates, they remained higher in this subsample than in the full sample. The pooled odds ratio for neighborhood disorder was 1.35 (95% CI: 1.16, 1.57)—10% higher when including only participants at retirement compared with all participants aged 50 years or older. The pooled odds ratio for lack of social cohesion was 1.93 (95% CI: 1.61, 2.30), indicating 17% higher odds of depression during retirement (Web Figure 4). Meta-regression analyses found significantly elevated risk of depression by lack of social cohesion in more equal countries (β = −0.188, P = 0.04) and in countries with higher population density (β = 0.194, P = 0.04) (Table 2). There was a tendency for associations between neighborhood disorder and depression to be weaker in countries with more forest coverage (β = −0.175, P = 0.099) and for associations between lack of social cohesion and depression to be stronger in countries with higher levels of air pollution (β = 0.205, P = 0.07).
The pooled neighborhood associations were robust and did not significantly differ when estimated in 1-stage IPD meta-analysis (random or fixed country effects) or in random-effects 2-stage IPD meta-analysis (Web Table 5). Analyses that used the composite neighborhood problems score produced risk estimates comparable to those calculated for lack of social cohesion (full sample: OR = 1.74, 95% CI: 1.49, 2.03; in retirement: OR = 1.96, 95% CI 1.60, 2.40) (Web Figure 1). Similarly to the main analysis, we found stronger associations between neighborhood problems and depression in more equal countries (β = −0.160, P = 0.04). In the subsample of retirees, there was a tendency toward weaker associations between neighborhood problems and depression in countries with more forest coverage (β = −0.248, P = 0.095) and toward stronger associations in countries with higher population density (β = 0.202, P = 0.07) (Web Table 4).
DISCUSSION
This cross-national longitudinal study provides evidence for a link between perceived neighborhood disorder and lack of social cohesion and depression among adults aged 50 years or older. These findings are based on analyses of data from 3 representative panel surveys including 32,531 participants across 16 high-income countries. Risk estimates were 10%–17% higher, on average, in a subsample containing only retired individuals than in the total sample. We identified low country-level variation between risks of depression by neighborhood problems, which could be partly explained by macro-level indicators such as income inequality, population density, forest coverage, and air pollution.
Our findings are in line with those of previous cross-sectional studies (9) and longitudinal studies exploring the possible effect of perceived neighborhood disorder (10, 11, 26) and social cohesion/social capital (12, 13, 25, 37) on the risk of depression in older age. As people age and then retire, the geographical extent of their mobility space tends to decrease, and they often become more reliant on their community and local services (9). At the same time, depression trajectories widen by neighborhood quality in aging individuals (12), leading to stronger associations between neighborhood and depression among retired individuals.
These findings suggest that the broader social, economic, and environmental context of a country might modify the association between neighborhood characteristics and depression. In Southern European countries, neighborhood disorder and lack of social cohesion did not increase the risk of depression, while in Eastern European and Anglo-Saxon countries we often found strong and significant associations. Type of welfare regime did not statistically explain differences, which may have been due to the low number of countries in each welfare-regime group. However, other unexplored social norms and cultural values predicting source of social support (community vs. family and close relatives) and ways of coping with residential stressors might be better predictors of modification of the relationship.
Meta-regression analysis estimated stronger risks of depression by lack of social cohesion, when people were living in economically more equal countries. Egalitarian countries tend to have better health outcomes, which might be linked via social capital or other aspects of social organization (38). Perceived lack of social cohesion in more equal economies, therefore, violates the normative rules of the society and the general expectation of people with regard to their neighborhoods and neighbors. This perceived discrepancy between reality and expectations might cause insecurity and lead to higher levels of psychological distress. There was also weak evidence for a modifying role of air pollution in the link between social cohesion and depression, which seems to be important in more polluted countries, where social cohesion can buffer the distress induced by air pollution (39). In addition to income inequality and air pollution, findings among retired individuals revealed that in countries where people live in closer proximity to each other, lack of social cohesion predicted depression more strongly. The value of the immediate community increases with higher population density, especially for individuals who are more reliant on their surroundings. Finally, neighborhood disorder tended to be associated with higher risk of mental health problems in countries with less forest coverage. Exposure to nature may be protective for mental health by reducing the hazardous effect of environmental distress (40) caused by (for example) neighborhood disorder, traffic noise, or air pollution.
This study had several strengths. We report here (for the first time, to our knowledge) pooled risks of depression for neighborhood disorder and lack of social cohesion among adults aged 50 years or older based on data from several high-income countries, many of them (e.g., Southern and Eastern European countries) often neglected in research. The presented analyses were based on longitudinal data with baseline and follow-up measures of outcome, placing this among the few prospective studies in the neighborhood literature. Effect estimates from 16 different countries were pooled together by IPD meta-analyses, taking into account demographic, socioeconomic, and health confounders. Moreover, we have provided possible explanations for country-level differences in the risk of depression by neighborhood problems.
The study also had limitations. First, the exposure, outcome, and covariates were all self-reported measures. Although we excluded possible depression cases at baseline to avoid the potential for underlying depression to distort the perceptions of neighborhood or covariates, we could not completely rule out reverse causation or an unmeasured psychological mechanism (e.g., reporting behavior) leading to biased estimates (41). Second, despite the high correlation between outcome measures, they have relevant differences (23): The CES-D Scale tends to have stronger associations with social and demographic factors than the EURO-D, indicating a more extreme pool of cases, and it captures a shorter time interval (1 week vs. 1 month). Third, there was a significant number of missing values for neighborhood perception. Although the sample size was not related to the variation between effect parameters, nonresponse bias might have influenced the results. Missing values for neighborhood originated from the survey method in ELSA and HRS (e.g., leave-behind questionnaire), while in SHARE only part of the sample (household respondents) was asked about their residential area, providing very different reasons for missingness in the pooled data set. Fourth, because neighborhood perception was not assessed in each wave, we could not include the same year of baseline and follow-up for all surveys, which meant that it is possible that unknown macroeconomic or societal changes may have affected the results. Fifth, several European and North American countries were not included in this study, due to either a lack of data or insufficient data harmonization. We cannot exclude the possibility that the absence of these countries may have influenced the study’s findings.
Future research should make use of comparable multicenter surveys (e.g., Gateway to Global Aging Data) and extend its focus to low- and middle-income countries. Although there are cross-sectional multicenter studies on residential environment and health available in different country settings (42), longitudinal evidence is needed to better understand how macro-level social and environmental indicators shape neighborhood effects. In addition, using objectively measured neighborhood exposure would overcome possible bias related to the use of self-report measures. Neighborhood environment is a significant determinant of mental health and has the potential to reduce the negative effects of socioeconomic inequalities on health (42). Moreover, it is modifiable and therefore offers policy-makers opportunities for intervention to enhance health among older adults (6). Policies, especially in countries with a stronger link between neighborhood and depression, should focus on improving the physical qualities of residential areas and supporting social ties in communities, which can reduce mental health problems and related disability and make positive contributions to healthy aging.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Center for Research on Environment, Society and Health, School of GeoSciences, University of Edinburgh, Edinburgh, United Kingdom (Gergő Baranyi, Jamie R. Pearce, Chris J. L. Dibben); Swiss National Centre of Competence in Research “LIVES—Overcoming Vulnerability: Life Course Perspectives,” Center for the Interdisciplinary Study of Gerontology and Vulnerability, University of Geneva, Geneva, Switzerland (Stefan Sieber, Stéphane Cullati); and Department of Readaptation and Geriatrics, Faculty of Medicine, University of Geneva, Geneva, Switzerland (Stéphane Cullati, Delphine S. Courvoisier).
This work was supported by the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie Actions (agreement 676060 (LONGPOP) with G.B., J.R.P., and C.J.L.D.) and the Swiss National Centre of Competence in Research “LIVES—Overcoming Vulnerability: Life Course Perspectives,” which is financed by the Swiss National Science Foundation (grant 51NF40-160590 to S.S. and S.C.).
The English Longitudinal Study of Ageing (ELSA) was developed by a team of researchers based at University College London, the United Kingdom National Centre for Social Research, and the Institute for Fiscal Studies. Funding was provided by the US National Institute of Aging and a consortium of United Kingdom government departments coordinated by the Office for National Statistics. ELSA data were collected by the National Centre for Social Research and made available through the UK Data Archive.
The Health and Retirement Study (HRS) was sponsored by the US National Institute on Aging (grant U01AG009740) and conducted by the University of Michigan. This analysis used Early Release data (for wave 2016), which have not been cleaned and may contain errors that will be corrected in the Final Public Release version of the data set.
Data collection in the Survey of Health, Ageing and Retirement in Europe (SHARE) was funded by the European Commission through the Fifth Framework Programme (grant QLK6-CT-2001-00360), the Sixth Framework Programme (projects SHARE-I3 (grant RII-CT-2006-062193), COMPARE (grant CIT5-CT-2005-028857), and SHARELIFE (grant CIT4-CT-2006-028812)), the Seventh Framework Programme (projects SHARE-PREP (grant GA 211909), SHARE-LEAP (grant GA 227822), and SHARE M4 (grant GA 261982)), and Horizon 2020 (projects SHARE-DEV3 (grant GA 676536) and SERISS (grant GA 654221)) and by the European Commission’s Directorate-General for Employment, Social Affairs and Inclusion. Additional funding was received from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the US National Institute on Aging (grants U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, and HHSN271201300071C), and various national funding sources (see http://www.share-project.org). This analysis used data from SHARE waves 5 and 6 (10.6103/SHARE.w5.610, 10.6103/SHARE.w6.610); see Börsch-Supan et al. (19) for methodological details.
This publication reflects only the authors’ views, and the Research Executive Agency of the European Commission is not responsible for any use that may be made of the information it contains.
Conflict of interest: none declared.
References
- 1. Hasin DS, Sarvet AL, Meyers JL, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75(4):336–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the Global Burden of Disease Study 2010. PLoS Med. 2013;10(11):e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174(4):307–311. [DOI] [PubMed] [Google Scholar]
- 4. Luppa M, Sikorski C, Luck T, et al. Age- and gender-specific prevalence of depression in latest-life—systematic review and meta-analysis. J Affect Disord. 2012;136(3):212–221. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization Global Health and Aging. Bethesda, MD: National Institutes of Health; 2011.. (NIH publication no. 11-7737). [Google Scholar]
- 6. Rechel B, Grundy E, Robine JM, et al. Ageing in the European Union. Lancet. 2013;381(9874):1312–1322. [DOI] [PubMed] [Google Scholar]
- 7. Buchtemann D, Luppa M, Bramesfeld A, et al. Incidence of late-life depression: a systematic review. J Affect Disord. 2012;142(1–3):172–179. [DOI] [PubMed] [Google Scholar]
- 8. Deng Y, McQuoid DR, Potter GG, et al. Predictors of recurrence in remitted late-life depression. Depress Anxiety. 2018;35(7):658–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Barnett A, Zhang CJP, Johnston JM, et al. Relationships between the neighborhood environment and depression in older adults: a systematic review and meta-analysis. Int Psychogeriatr. 2017;30(8):1153–1176. [DOI] [PubMed] [Google Scholar]
- 10. Bierman A. Marital status as contingency for the effects of neighborhood disorder on older adults’ mental health. J Gerontol B Psychol Sci Soc Sci. 2009;64B(3):425–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Roberts RE, Kaplan GA, Shema SJ, et al. Does growing old increase the risk for depression? Am J Psychiatry. 1997;154(10):1384–1390. [DOI] [PubMed] [Google Scholar]
- 12. Ruiz M, Scholes S, Bobak M. Perceived neighbourhood social cohesion and depressive symptom trajectories in older adults: a 12-year prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2018;53(10):1081–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. 2015;69(10):1021–1028. [DOI] [PubMed] [Google Scholar]
- 14. Chung H, Ng E, Ibrahim S, et al. Welfare state regimes, gender, and depression: a multilevel analysis of middle and high income countries. Int J Environ Res Public Health. 2013;10(4):1324–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bambra C, Eikemo TA. Welfare state regimes, unemployment and health: a comparative study of the relationship between unemployment and self-reported health in 23 European countries. J Epidemiol Community Health. 2009;63(2):92–98. [DOI] [PubMed] [Google Scholar]
- 16. Esping-Andersen G. The Three Worlds of Welfare Capitalism. Cambridge, United Kingdom: Polity Press; 1990. [Google Scholar]
- 17. Steptoe A, Breeze E, Banks J, et al. Cohort profile: the English Longitudinal Study of Ageing. Int J Epidemiol. 2013;42(6):1640–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fisher GG, Ryan LH. Overview of the Health and Retirement Study and introduction to the special issue. Work Aging Retire. 2018;4(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Börsch-Supan A, Brandt M, Hunkler C, et al. Data resource profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 2013;42(4):992–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sonnega A, Faul JD, Ofstedal MB, et al. Cohort profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43(2):576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 22. Prince MJ, Reischies F, Beekman AT, et al. Development of the EURO-D scale—a European Union initiative to compare symptoms of depression in 14 European centres. Br J Psychiatry. 1999;174(4):330–338. [DOI] [PubMed] [Google Scholar]
- 23. Courtin E, Knapp M, Grundy E, et al. Are different measures of depressive symptoms in old age comparable? An analysis of the CES-D and Euro-D scales in 13 countries. Int J Methods Psychiatr Res. 2015;24(4):287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Suemoto CK, Ueda P, Beltran-Sanchez H, et al. Development and validation of a 10-year mortality prediction model: meta-analysis of individual participant data from five cohorts of older adults in developed and developing countries. J Gerontol A Biol Sci Med Sci. 2017;72(3):410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fone D, White J, Farewell D, et al. Effect of neighborhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychol Med. 2014;44(11):2449–2460. [DOI] [PubMed] [Google Scholar]
- 26. Stafford M, McMunn A, Vogli R. Neighbourhood social environment and depressive symptoms in mid-life and beyond. Ageing Soc. 2011;31(6):893–910. [Google Scholar]
- 27. UNESCO Institute for Statistics International Standard Classification of Education: ISCED 2011. Montreal, QC, Canada: UNESCO Institute for Statistics; 2012. [Google Scholar]
- 28. Jürges H. Health inequalities by education, income and wealth: a comparison of 11 European countries and the US. Appl Econ Lett. 2010;17(1):87–91. [Google Scholar]
- 29. Chan KS, Kasper JD, Brandt J, et al. Measurement equivalence in ADL and IADL difficulty across international surveys of aging: findings from the HRS, SHARE, and ELSA. J Gerontol B Psychol Sci Soc Sci. 2012;67(1):121–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ferrera M. The ‘Southern model’ of welfare in social Europe. J Eur Soc Policy. 1996;6(1):17–37. [Google Scholar]
- 31. The World Bank World Bank Open Data. World Development Indicators. Washington, DC: World Bank; 2017. https://data.worldbank.org/. Accessed January 31, 2019. [Google Scholar]
- 32. The World Bank World Development Indicators. Gini Index (World Bank Estimate). Washington, DC: World Bank; 2017. https://data.worldbank.org/indicator/SI.POV.GINI/. Accessed January 31, 2019. [Google Scholar]
- 33. Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med. 2017;36(5):855–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Basagaña X, Pedersen M, Barrera-Gomez J, et al. Analysis of multicentre epidemiological studies: contrasting fixed or random effects modelling and meta-analysis. Int J Epidemiol. 2018;47(4):1343–1354. [DOI] [PubMed] [Google Scholar]
- 36. Bryan ML, Jenkins SP. Multilevel modelling of country effects: a cautionary tale. Eur Sociol Rev. 2016;32(1):3–22. [Google Scholar]
- 37. Choi N, Kim J, Dinitto DM, et al. Perceived social cohesion, frequency of going out, and depressive symptoms in older adults: examination of longitudinal relationships. Gerontol Geriatr Med. 2015;1:2333721415615478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kawachi I, Kennedy BP, Lochner K, et al. Social capital, income inequality and mortality. Am J Public Health. 1997;87(9):1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wang RY, Xue DS, Liu Y, et al. The relationship between air pollution and depression in China: is neighbourhood social capital protective? Int J Environ Res Public Health. 2018;15(6):Article 1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hartig T, Mitchell R, Vries S, et al. Nature and health. Annu Rev Public Health. 2014;35:207–228. [DOI] [PubMed] [Google Scholar]
- 41. Diez Roux AV. Neighborhoods and health: where are we and were do we go from here? Rev Epidemiol Sante Publique. 2007;55(1):13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mitchell RJ, Richardson EA, Shortt NK, et al. Neighborhood environments and socioeconomic inequalities in mental well-being. Am J Prev Med. 2015;49(1):80–84. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


