Abstract
Background
Low-resource countries with fragile healthcare systems lack trained healthcare professionals and specialized resources for COVID-19 patient hospitalization, including mechanical ventilators. Additional socio-economic complications such as civil war and financial crisis in Libya and other low-resource countries further complicate healthcare delivery.
Methods
A cross-sectional survey evaluating hospital and intensive care unit's capacity and readiness was performed from 16 leading Libyan hospitals in March 2020. In addition, a survey was conducted among 400 doctors who worked in these hospitals to evaluate the status of personal protective equipment.
Results
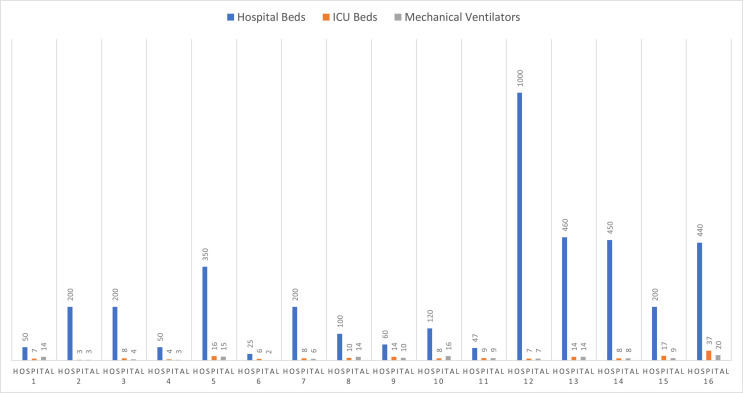
Out of 16 hospitals, the highest hospital capacity was 1000 in-patient beds, while the lowest was 25 beds with a median of 200 (IQR 52–417, range 25–1000) hospital beds. However, a median of only eight (IQR 6–14, range 3–37) available functioning ICU beds were reported in these hospitals. Only 9 (IQR 4.5–14, range 2–20) mechanical ventilators were reported and none of the hospitals had a reverse transcription-polymerase chain reaction machine for COVID-19 testing. Moreover, they relied on one of two central laboratories located in major cities. Our PPE survey revealed that 56.7% hospitals lacked PPE and 53% of healthcare workers reported that they did not receive proper PPE training. In addition, 70% reported that they were buying the PPE themselves as hospitals did not provide them.
Conclusion
This study provides an alarming overview of the unpreparedness of Libyan hospitals for detecting and treating patients with COVID-19 and limiting the spread of the pandemic.
Keywords: COVID-19, Intensive care units, Personal protective equipment, Pandemic, Outbreak, SARS-CoV-2
List of abbreviations: COVID-19, Coronavirus disease 2019; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; ICU, Intensive care unit; PPE, Personal protective equipment; WHO, World Health Organization
Highlights
-
•
We report the healthcare system preparedness for COVID19 in low resource settings.
-
•
We provide insight into the health care situation in Libya during the civil war and COVID19 outbreak.
-
•
Our study provides the infrastructure status of intensive care units in Libya.
-
•
The low number of personal protective equipment plays a significant role in spreading the infection among healthcare workers.
-
•
Civil war along with COVID19 pandemic can have catastrophic consequences for the healthcare system in African countries.
Introduction
The World Health Organization (WHO) designated the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19). It led to numerous cases of severe viral pneumonia and was first identified in the city of Wuhan, Hubei Province, China [1]. As of May 22, 2020, more than 5 million cases and 335,000 deaths were recorded worldwide [2] (see Fig. 1 ).
Figure 1.
Hospital basic characteristics, according to number of hospital beds, intensive care unit (ICU) beds, and mechanical ventilators.
Recent reports indicated that 20–45% of individuals with COVID-19 would require hospitalization [3,4]. Moreover, the intensive care unit (ICU) admission rates were reported to be between 5% and 26% in countries such as the USA, Italy, and China [[5], [6], [7], [8], [9], [10]]. Patients with COVID-19 may develop acute respiratory distress syndrome (ARDS), which requires endotracheal intubation and mechanical ventilation. In addition, precautions have to be taken to avoid aerosol-generating droplets during intubation [[11], [12], [13], [14]].
Specialized high-resource clinical settings with highly trained healthcare professionals and access to mechanical ventilators are essential for hospitalization of COVID-19 patients; none of which are feasible in low-resource countries with a fragile healthcare system. Furthermore, inadequate governmental plans in low-resource countries and the presence of socio-economic factors, such as civil war and financial crises, further complicate healthcare delivery [15,16]. The low number of reported cases in such countries could be due to a limited availability of testing resources and decreased ability of the healthcare system to detect and treat COVID-19 cases [17].
In addition, concerns regarding personal protective equipment (PPE) availability have been reported in the literature and anecdotally by frontline health professionals [18,19]. These concerns have been addressed by WHO in a report, wherein recommendations and guidance for rational use of PPE during the COVID-19 pandemic have been provided for healthcare workers [20].
Owing to these problems in low-resource countries, their ability and capacity to manage and control COVID-19 has raised concerns and may indirectly result in higher mortality rates. This study aims to provide an overview on the preparation level of the hospitals to manage COVID-19 in low-resource countries.
Methods
A cross-sectional survey evaluating the capacity as well as the readiness of hospitals and ICUs was conducted in March 2020 by collecting data from 16 leading hospitals in Libya. The survey recorded the following data: type of hospital, number of hospital and ICU beds, nurse-to-patient ratio, number of infectious disease and pulmonary specialists, presence of antibiotic policy and stewardship, presence of microbial isolation measures, weaning protocol, availability of infectious disease diagnostic techniques, data recording policy, and daytime laboratory availability during shifts. Only hospitals with ICUs that could receive patients with COVID-19 (secondary or tertiary centers) were included in the analysis. Hospitals without ICUs were excluded from the study.
Additionally, a survey was conducted among 400 doctors who worked in these hospitals to evaluate the availability of PPE and the presence of PPE training programs. Healthcare workers were also enquired about the ability of hospitals to provide PPE.
Statistical analysis was performed using SPSS (IBM SPSS Statistics, Version 25.0; IBM Corp., Armonk, NY). Descriptive analysis was reported by frequency, percentage, mean, and standard deviation. Nonparametric data were presented as median and interquartile range (IQR).
Results
Hospital size and bed volume
Out of 16 hospitals, 14 were public, and two were private hospitals. The maximum hospital bed capacity was 1000 in-patient beds, while the lowest was 25 beds. Seven hospitals had less than 200 beds, while nine of them had more than 200 beds. Of the 16 hospitals, only nine (56.3%) were tertiary centers, whereas the remaining were secondary centers. Eleven (68.8%) of them were teaching hospitals, and the remaining were in rural or nonteaching categories. There was a median of 200 (IQR 52–417, range 25–1000) hospital beds among all 16 hospitals. However, a median of 8 (IQR 6–14, range 3–37) available functioning ICU beds were found in the hospitals. In most hospitals, 10 (62.5%) were mixed ICUs (surgical and medical), and the remaining were medical ICUs. There was a median of 9 (IQR 4.5–14, range 2–20) mechanical ventilators in the hospitals.
Infection control
Only 10 out of 16 hospitals reported having written recommendations for antibiotics. In contrast, 10 (62.5%) hospitals had written infection control guidelines for COVID-19, including interventions to control infection sources, identifying and isolating suspected cases, and disinfection measures. Only 3 (18.8%) hospitals reported an antibiotic stewardship program.
Laboratory infection surveillance
None of the hospitals had a reverse transcription-polymerase chain reaction machine for detecting COVID-19. Moreover, they relied on central laboratories in either Tripoli or Benghazi, located hundreds of kilometers from some of these hospitals. No other coronavirus testing methods were available in any of the hospitals. Additionally, blood culture accessibility was reported in 11 hospitals, while others had no access. Lastly, septic screening procedures were not available in 62.5% of hospitals.
Availability of healthcare workers
The nurse to patient ratio was 1:4 and 1:2 in 62.5% and the remaining 37.5% of hospitals, respectively. There was a shortage of nurses during the night shift, with only two hospitals having four nurses in the ICU, while no nurses were present in seven hospitals. Three hospitals had one nurse for two patients, and only four hospitals had a 1:1 nurse to patient ratio. In addition, no triage system for COVID-19 was reported in 12 (75%) hospitals.
Only nine hospitals had infectious disease specialists at the consultant level, whereas no such specialists were found in seven hospitals. However, intensive care specialists were available for 24 h a day in nine (56.3%) hospitals, four hospitals had them on-call for 24 h a day, and three hospitals lacked the 24-h presence of such specialists.
Personal protective equipment (PPE)
We received 300 responses from 400 doctors who were questioned (response rate 75%). Out of 300 doctors who responded to the survey, 170 (56.7%) reported that the supply of PPE was inadequate. In addition, 159 (53%) reported that they did not receive proper PPE training. Furthermore, 210 (70%) of them reported that the hospitals were not providing PPE and purchased their own.
Discussion
Hospitals in Libya were found to be unprepared for the COVID-19 pandemic. Hospital beds and mechanical ventilators were lacking in number to combat the pandemic adequately. In addition, the absence of infection control policies and COVID-19 testing kits may place hospitals at a higher risk of disease transmission, as low testing ability can increase the spread of SARS-CoV-2 infection and hinder containment efforts. Our study focused on the main centers in important cities, which were designated to receive and manage patients with COVID-19.
To the best of our knowledge, this is the first study describing ICU capacity, hospital resources, and readiness for the COVID-19 pandemic in low-resource countries. However, more studies are required in this area to compile a comprehensive overview of the preparedness of such countries.
Considerable attention must be paid when interpreting the study results, as a low number of ICU beds is a primary concern for countries at risk of COVID-19 outbreak. Despite having a large number of hospital beds, a report by WHO found that only around 40% of hospital beds are available and functioning in Libyan hospitals [21].
Based on the data collected from hospitals in Tripoli, a city with a population of 1.165 million people, we estimated that 100 ICU beds were available [22]. In addition, the largest hospital had 20 functioning mechanical ventilators, while some hospitals had only 2–6, which is the result of low government spending on healthcare. These numbers are concerning as a previous study conducted in the UK has shown that two-thirds of ICU-admitted patients require mechanical ventilation [23]. However, the civil war in Libya has resulted in the closure of borders limiting the import of foreign equipment, replacement parts, or qualified personnel to repair malfunctioning ventilators in Libyan hospitals. Therefore, it is necessary that the government provide an adequate number of mechanical ventilators and repair the existing ones, especially in the leading hospitals authorized to admit COVID-19 patients and those with ARDS as it can cause respiratory failure [7,24].
About two-thirds (62.5%) of hospitals have a patient to nurse ratio of 4:1. This shortage of nurses is a significant concern and questions the ability of the Libyan healthcare system to respond to COVID-19. Moreover, most of the nurses in Libya are prepared through small community colleges without undergoing training in intensive care. This necessitates urgent intervention by either importing nurses from foreign countries with specific training and experience, or by implementing appropriate training courses for nurses with an aim to work effectively in an ICU setting.
Education and training of ICU staff is the most effective measure to control infection. The training conducted for healthcare workers during COVID-19 should focus on the following: handling and disinfecting PPE, online lecture courses aiming to provide guidance training, and courses to improve staff preparedness as well as their abilities to combat COVID-19, and to treat patients appropriately [25,26].
Another primary concern raised in this study was the lack of infection control protocols and practice in the hospitals, wherein it was found that only 10 (62.5%) hospitals recorded infection control measures. In a study conducted in China, a lack of infection control measures was the most common cause of healthcare worker-associated SARS-CoV-2 infection [27]. Therefore, implementing infection control strategies, appropriate PPE removal, recording vital signs and information of healthcare workers, and providing an adequate supply of PPE are crucial for decreasing the risk of SARS-CoV-2 infection among healthcare workers.
Of the 300 participants questioned in this study, more than half stated a low availability of PPE and training, which is a major concern. Most of the participants reported purchasing PPE by themselves. In addition, some revealed that the PPE provided by hospitals is inadequate in type and insufficient in quantity, resulting in their reuse or prolonged use. These highlight the importance of providing sufficient and appropriate PPE to COVID-19 affected hospitals [28,29]. WHO has recommended the provision of PPE to healthcare workers during the COVID-19 pandemic, including medical masks, protective eye gear, gloves, respirators, and gowns. However, some strategies can be followed to facilitate PPE availability, such as using PPE appropriately and correctly, coordinating PPE supply nationally and internationally, and minimizing PPE use by reducing viral exposure using glass windows, delaying elective procedures, and restricting the number of healthcare workers to a safe level [20].
A previous study found that about 90% of healthcare workers exhibited incorrect doffing techniques [30]. Therefore, there is an urgent need to provide training on using PPE correctly, and on its appropriate size and amount as self-contamination can occur during removal or manipulation of PPE [31].
Another primary concern is the availability of COVID-19 laboratory testing facilities. Only two laboratories located in Tripoli and Benghazi carried out COVID-19 testing. As of May 12, 2020, only 2935 tests have been carried out in Libya since the start of the pandemic with an average potential of less than 50 tests per day, which is very low compared to other countries [[32], [33], [34]]. This is due to the shortage of testing supplies and the absence of local laboratories. Moreover, diagnosis and treatment of suspected cases may be delayed due to the remoteness of testing laboratories, as it requires several hours for the samples to reach. Without rapid detection and quarantine of patients with COVID-19, the infection can spread quickly. Moreover, two hospitals were reportedly attacked in Tripoli, imposing more pressure on the healthcare system to combat and control COVID-19.
Our study evaluated the preparedness of the ICUs in a low-resource country and provided means to compare the healthcare capacity and preparedness of other low-resource countries in managing the COVID-19 pandemic. This is the first report on the capacity of a low-resource country to respond to the pandemic. Future studies could focus on the availability of trained infection prevention and control specialists, as recommended by the WHO [35]. Moreover, there is a need for future surveys to focus on hand hygiene containing information regarding the availability of hand hygiene materials and its related training as they play a crucial part in the healthcare system of low-resource countries to control COVID-19.
Conclusions
This study provides an overview of ICU capacity and preparedness in Libyan hospitals during the COVID-19 pandemic. Immediate efforts and determined actions are needed to improve the situation in Libyan hospitals. Furthermore, this study provides information on the alarming decline in intensive care services that render Libya vulnerable to COVID-19. Moreover, this may result in increased propagation of SARS-CoV-2 and raise mortality in a low-resource country that is already devastated by civil war.
Ethics
Ethical approval for this study was granted from the Bioethics Committee at Biotechnology Research Center in Libya. All participants provided consent before participating in the study.
Authorship statement
Conceptualization: M. Elhadi, Ahmed Msherghi, Ala Khaled.
Data curation: Muhammed Elhadi, Ahmed Msherghi, Mohammed Alkeelani, Ali Alsuyihili, Ala Khaled, Anis Buzreg, Tariq Boughididah, Mohamed Abukhashem, Ayiman Alhashimi, Samer Khel, Rawanda Gaffaz, Najah Ben Saleim, Sumayyah Bahroun, Abdelmunam Elharb, Mohamed Eisay, Nafati Alnafati, Bushray Almiqlash, Marwa Biala, Esra Alghanai.
Investigation: M. Elhadi, A. Msherghi.
Writing - Original draft: M. Elhadi.
Writing - review & editing: Muhammed Elhadi, Ahmed Msherghi, Mohammed Alkeelani, Ali Alsuyihili, Ala Khaled, Anis Buzreg, Tariq Boughididah, Mohamed Abukhashem, Ayiman Alhashimi, Samer Khel, Rawanda Gaffaz, Najah Ben Saleim, Sumayyah Bahroun, Abdelmunam Elharb, Mohamed Eisay, Nafati Alnafati, Bushray Almiqlash, Marwa Biala, Esra Alghanai.
All authors agree to accept equal responsibility for the accuracy of this paper and the authors approved the final article.
Declaration of Competing Interest
The authors declare no conflicts of interest.
Funding
This study was not supported by any grant or funding from a department or institute.
E-mail addresses of the authors
Ahmedmsherghi@gmail.com (A. Msherghi), Albshrimohamed@gmail.com (M. Alkeelani), Al4light@gmail.com (A. Alsuyihili), ala.khaled.el@gmail.com (A. Khaled), anisbuzreg94@gmail.com (A. Buzreg), Tariq.bugadeda@gmail.com (T. Boughididah), bukhshe@gmail.com (M. Abukhashem), emanalghrari@yahoo.com (A. Alhashimi), samer17ly@gmail.com (S. Khel), Drrgaffaz@hotmail.com (R. Gaffaz), najahas352@gmail.com (N. Ben Saleim), Sumayyah.ghyth@gmail.com (S. Bahroun), Abdelmoneem_93@yahoo.com (A. Elharb), Alfajralfaj@gmail.com (M. Eisay), Nafatyshgra@gmail.com (N. Alnafati), eledia092@gmail.com (B. Almiqlash), Marwabiala07@gmail.com (M. Biala), Esraaer2@gmail.com (E. Alghanai).
Provenance and peer review
Not commissioned; externally peer reviewed.
Acknowledgements
We would like to show our appreciation for the nursing department and all healthcare staff who have been supportive of the efforts in our fight against COVID-19.
References
- 1.Organization WH . WHO; 2020. Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. [Google Scholar]
- 2.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, february 12-march 16, 2020. MMWR Morbidity and mortality weekly report. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 7.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls Publishing; 2020. Features, evaluation and treatment coronavirus (COVID-19). StatPearls. Treasure island (FL) StatPearls Publishing LLC. [PubMed] [Google Scholar]
- 9.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323(16):1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 10.Arentz M., Yim E., Klaff L., Lokhandwala S., Riedo F.X., Chong M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323(16):1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheung J.C., Ho L.T., Cheng J.V., Cham E.Y.K., Lam K.N. Staff safety during emergency airway management for COVID-19 in Hong Kong. The Lancet Respiratory medicine. 2020;8(4):e19. doi: 10.1016/S2213-2600(20)30084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yao W., Wang T., Jiang B., Gao F., Wang L., Zheng H. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meng L., Qiu H., Wan L., Ai Y., Xue Z., Guo Q. Intubation and ventilation amid the COVID-19 outbreak: wuhan's experience. Anesthesiology. 2020 doi: 10.1097/ALN.0000000000003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orser B.A. Recommendations for endotracheal intubation of COVID-19 patients. Anesth Analg. 2020 May;130(5):1109–1110. doi: 10.1213/ANE.0000000000004803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daw M.A. 2020. Corona virus infection in Syria, Libya and Yemen; an alarming devastating threat. Travel medicine and infectious disease; p. 101652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daw M.A. Libyan healthcare system during the armed conflict: challenges and restoration. African journal of emergency medicine : Revue africaine de la medecine d'urgence. 2017;7(2):47–50. doi: 10.1016/j.afjem.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Organization WH . 2019. Coronavirus disease 2019 (COVID-19). Situation report—71.https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200331-sitrep-71-covid-19pdf?sfvrsn=4360e92b_6. 2020 [Google Scholar]
- 18.Mandrola J. CoViD-19 and PPE: some of us will die because of the shortage. Recenti Prog Med. 2020;111(4):183. doi: 10.1701/3347.33175. [DOI] [PubMed] [Google Scholar]
- 19.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages - the need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med. 2020;382(18):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 20.Organization WH WHO Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19): interim guidance. https://wwwwhoint/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control
- 21.Organization WH . 2017. Health emergencies and humanitarian response update.https://wwwwhoint/hac/crises/lby/sitreps/en/ [Google Scholar]
- 22.Factbook TW Major urban areas — population by central intelligence agency. https://wwwciagov/library/publications/the-world-factbook/fields/350html. 2018
- 23.Mahase E. Covid-19: most patients require mechanical ventilation in first 24 hours of critical care. BMJ. 2020;368:m1201. doi: 10.1136/bmj.m1201. [DOI] [PubMed] [Google Scholar]
- 24.Murthy S., Gomersall C.D., Fowler R.A. Care for critically ill patients with COVID-19. Jama. 2020 doi: 10.1001/jama.2020.3633. [DOI] [PubMed] [Google Scholar]
- 25.Goh K.J., Wong J., Tien J.-C.C., Ng S.Y., Duu Wen S., Phua G.C. Preparing your intensive care unit for the COVID-19 pandemic: practical considerations and strategies. Crit Care. 2020;24(1):215. doi: 10.1186/s13054-020-02916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong J., Goh Q.Y., Tan Z., Lie S.A., Tay Y.C., Ng S.Y. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2020;67(6):732–745. doi: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peng J., Ren N., Wang M., Zhang G. Practical experiences and suggestions for the 'eagle-eyed observer': a novel promising role for controlling nosocomial infection in the COVID-19 outbreak. J Hosp Infect. 2020;105(1):106–107. doi: 10.1016/j.jhin.2020.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Sullivan E.D. PPE guidance for covid-19: be honest about resource shortages. BMJ. 2020;369:m1507. doi: 10.1136/bmj.m1507. [DOI] [PubMed] [Google Scholar]
- 29.Rowan N.J., Laffey J.G. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from Coronavirus disease (COVID19) pandemic - case study from the Republic of Ireland. Sci Total Environ. 2020;725:138532. doi: 10.1016/j.scitotenv.2020.138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Phan L.T., Maita D., Mortiz D.C., Weber R., Fritzen-Pedicini C., Bleasdale S.C. Personal protective equipment doffing practices of healthcare workers. J Occup Environ Hyg. 2019;16(8):575–581. doi: 10.1080/15459624.2019.1628350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Phua J., Weng L., Ling L., Egi M., Lim C.-M., Divatia J.V. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. The Lancet Respiratory medicine. 2020;8(5):506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Libya NCfDC . 2020. https://covid19ly/. 2020 (COVID19 status in April,s 10). [Google Scholar]
- 33.Max Roser H.R., Ortiz-Ospina Esteban, Joe Hasell. Coronavirus disease (COVID-19) – Statistics and Research. https://ourworldindataorg/coronavirus. 2020
- 34.Elhadi M., Msherghi A. COVID-19 and civil war in Libya: the current situation. Pathog Glob Health. 2020:1–2. doi: 10.1080/15575330.2020.1769292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Organization WH . 2019. Minimum Requirements for infection prevention and control (IPC) programmes.https://wwwwhoint/infection-prevention/publications/core-components/en/ [Google Scholar]