Abstract
The coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has attracted worldwide concerns because of its high person-to-person infectivity and lethality, and it was labeled as a pandemic as the rapid increase in the number of confirmed patients in most areas around the world became evident. The SARS-CoV-2 is mainly transmitted through respiratory droplets and close contact. There is also evidence of transmission through aerosols and digestive tracts. Because orthodontic treatment involves a large population who need routine return-visits, it was significantly affected and suspended because of the COVID-19 pandemic and the shutdown of the dental clinics and hospitals. Although the spread of COVID-19 has been effectively controlled in China, and many areas have gradually resumed work and classes, orthodontic participants are still under high risks of SARS-CoV-2 infection. This is due to the fact that the asymptomatic carriers of SARS-CoV-2 or patients in the incubation period may cause the cross-infection between orthodontic practitioners and patients. The close proximity between the practitioners and the patients, and the generation of droplets and aerosols that contain saliva and blood during treatment further increase the risks of transmission. In this article, we summarized the preventive strategies for control of SARS-CoV-2 transmission to protect both staff and patients during the orthodontic practice.
Highlights
-
•
Characteristics of COVID-19 and SARS-CoV-2 were introduced.
-
•
Potential transmission routes of SARS-CoV-2 during orthodontic practice were summarized.
-
•
Strategies for control of SARS-CoV-2 transmission in orthodontic practice were recommended.
Since its emergence in December 2019, the coronavirus disease 2019 (COVID-19) has spread rapidly and is now a global pandemic. The pathogen causing COVID-19 was initially named 2019-novel coronavirus (2019-nCoV), and then officially named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A public health emergency of international concern over this disease was announced by the World Health Organization on January 30, 2020.1 Because of the particularity of the dental treatment procedures, the risk of SARS-CoV-2 transmission between dental practitioners and patients could be high.2 Thus, all the routine dental practices were suspended after the outbreak of COVID-19 in many areas around the world, and only emergency services were provided.3 Because the COVID-19 has been effectively controlled in China and some other areas, dental clinics and hospitals are gradually resuming regular services. However, the prevention and the control of SARS-CoV-2 transmission during dental practice are still serious and challenging. The most critical reason is that asymptomatic patients and patients in their incubation period are also carriers of SARS-CoV-2 and can be infectious.4 It is difficult to identify and quarantine these patients in time, which can result in the SARS-CoV-2 transmission in the population. In addition, the close contact between dental staff and patients, as well as the droplets and aerosols generated during treatment containing saliva and blood, further increase the risk of SARS-CoV-2 transmission in dental practice.5 In addition, because of the previous suspension, many orthodontists are currently under heavy workload to reschedule the accumulated return-visit patients whose treatments were significantly affected and postponed. A study from Jordan found that although most Jordanian dentists were aware of COVID-19 symptoms, mode of transmission, and infection control and measures in the dental clinic, they had limited knowledge of the extra precautionary measures that are essential to protect the dental staffs and other patients from SARS-CoV-2 infection.6 Thus, the standard control measures in our previous daily orthodontic work may not be enough to prevent the transmission of SARS-CoV-2 and protect both practitioners and patients from the COVID-19. Effective control protocols during orthodontic practice are urgently needed.7
Characteristics of COVID-19 and SARS-CoV-2
Clinical manifestations
The most common manifestations of the COVID-19 infected patients are fever and dry cough. Some have fatigue, diarrhea, and other digestive tract symptoms. Severe patients can rapidly progress to acute respiratory distress syndrome, septic shock, metabolic acidosis, coagulation dysfunction, and multiple organ failure.8 Most patients who underwent chest computed tomography showed bilateral pneumonia with ground-glass opacity and bilateral patchy shadows.9 However, some patients who are SARS-CoV-2 carriers could be asymptomatic.4 Patients in the incubation period could also not show the typical symptoms. The incubation period of COVID-19 has been estimated at 3-14 days with an average of 5-6 days,10 , 11 but there is also evidence that it could be as long as 24 days.12 Studies have reported that majority of patients (50%-80%) were considered asymptomatic at the early phase of infection but released large amounts of SARS-CoV-2, which were infectious and posed enormous challenges for controlling the spread of COVID-19.13 , 14
Possible transmission routes
The SARS-CoV-2 has been found the evidence of rapid person-to-person transmission and susceptible to different age groups in clinical epidemiology studies.11 The virus is mainly transmitted by respiratory droplets from talking, coughing, or sneezing, and direct or indirect contact with nasal, oral, and eye mucous.15 It has been reported that SARS-CoV-2 was widely distributed on floors, computer mice, trash cans, sickbed handrails, and in the air up to 4 m away from patients in hospital wards.16 Another study also found that SARS-CoV-2 could remain viable and infectious on different types of environmental surfaces for a few hours or up to several days.17 The contact with these contaminated surfaces would largely increase the risk of transmission. More importantly, studies have indicated that aerosol transmission of SARS-CoV-2 is plausible because the virus in aerosols can stay viable and infectious for about 3 hours.17, 18, 19 In addition, a growing number of clinical evidence reminds us that the digestive system may also serve as an alternative route of infection because SARS-CoV-2 could be detected from the stool specimen of the confirmed patient.20 , 21 SARS-CoV-2 could also be detected in the self-collected saliva of most infected patients, even if not in nasopharyngeal aspirate, suggesting the possibility of salivary gland infection and possible transmission.22 , 23 Another study also suggested that angiotensin-converting enzyme II–expressing cells in oral mucosa, especially in epithelial cells of the tongue, might provide possible routes of entry for the SARS-CoV-2, which indicates that the oral cavity is a potentially high-risk route for SARS-CoV-2 infectious susceptibility.24
Possible transmission routes of SARS-CoV-2 during orthodontic practice
During the orthodontic practice, the patient's mouth and nose are in close proximity to orthodontists and assisting staffs for long periods. The communication, coughing, or sneezing during the practice can easily bring out the respiratory droplets. Direct contact with saliva or blood of the infected patients during orthodontic procedures within the mouth include photographing, impression taking, oral scanning, bracket, and attachment bonding or removal, archwire changing, anchorage screw implantation, and so on. Indirect contact with contaminated dental settings and environmental surfaces will also increase the risk of virus transmission. The use of orthodontic tools and materials, including pliers, power chains, and adhesives, which are usually not individually packaged or disposable, will increase the risk of cross-infection. In addition, the use of high-speed handpieces and high-pressure 3-way syringes during bracket or attachment bonding and removal will generate a large number of saliva or blood-mixed droplets and aerosols which could remain suspended in the air for long periods before they settle on environmental surfaces or enter the respiratory tract.5 , 25 In addition, fecal-oral routes may also be a potential transmission route during orthodontic procedures, especially the self-operation by patients, such as the placement and removal of the clear aligners, elastics, and other removable appliances. Thus, the major transmission routes of SARS-CoV-2 in orthodontic practice are respiratory droplets, direct or indirect contact, saliva or blood-mixed aerosols, and the digestive tract. Effective control strategies to prevent the transmission of SARS-CoV-2 through these routes are needed.7
Infection control strategies in orthodontic practice
Although vaccines are the most effective strategy for preventing infectious disease, research groups around the world are accelerating the development of COVID-19 vaccines using various approaches, but there are still no vaccines available for COVID-19 currently.26 , 27 Therefore, it is critical to take infection prevention and control measures to lower the risk of transmission as the next best option. Orthodontic care providers should know the transmission routes of SARS-CoV-2, how to screen suspected patients, and what protective measures should be taken. Because there are no official guidelines for control of SARS-CoV-2 transmission during the orthodontic practice in China and worldwide as this manuscript was drafted, listed below is a summary and recommendations of the control measures that could be followed by orthodontic care providers based on the practice experience in West China Hospital of Stomatology, Sichuan University, previously published literature on control protocols in dental practice, and guidelines for the management of COVID-19 released by the major health bodies, such as the National Health Commission of China, World Health Organization, and national dental associations.8 , 28, 29, 30, 31
Basic principles
1. Strengthen the organization and management of the clinic or hospital, make systematic plans and procedures for the prevention and control of COVID-19, and give training to all staff, including cleaners and security personnel, to make sure everyone is aware.
2. Pay close attention to the changes in the pandemic situation and adjust the control strategies according to the management requirements of the national and local health administrative institutions.
3. Strictly perform the procedures of patient evaluation and pre-examination and triage before orthodontic practice to achieve early detection, early reporting, and early isolation for COVID-19 suspected or infected patients.
4. Manage only orthodontic emergencies in areas where COVID-19 spreads; nonemergency orthodontic practices should be postponed.32 , 33 After the effective control of COVID-19 in the area, first-visit or return-visit patients should be carefully scheduled and avoid the aggregation of patients and their companies.
5. Reinforce the hand hygiene, use personal protective equipment, and take disinfection measures for dental settings, tools, and medical wastes to avoid iatrogenic infection.
6. Reduce the use of high-speed dental handpieces and high-pressure 3-way syringes during the practice while increasing the use of saliva ejectors with high volume to minimize the environment pollution by droplets and aerosols.
Pre-examination and triage of patients before orthodontic procedures
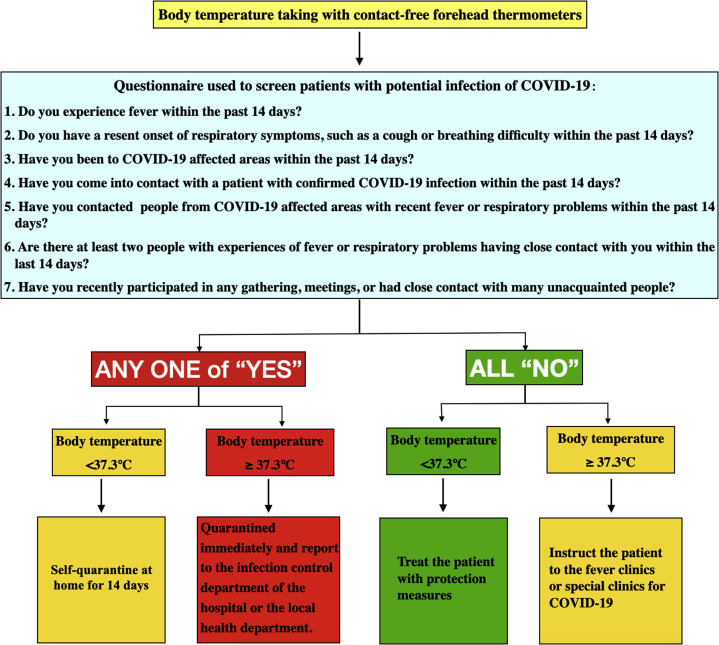
Before entering the dental clinics or hospitals, each patient should be evaluated at the entrance, whether they are suspected patients of COVID-19. To date, the National Health Commission of the People's Republic of China has released the seventh edition of the Guideline for the Diagnosis and Treatment of COVID-19.8 According to the guideline, first, the temperature of each patient should be taken using contact-free forehead thermometers. Second, a questionnaire should be used to screen the suspected patients to take different actions according to the triage of the patients, as shown in the flow chart of the Figure . Notably, staff responsible for temperature measurements and questionnaires should take protective measures as recommended in the Table . In addition, a safety distance of at least 6 ft or 2 m between people should be maintained while completing the questionnaire or in the waiting area in case that they spray droplets from their nose or mouth, which may contain viruses when someone coughs, sneezes, or speaks.34 , 35 In addition, patients are also suggested to wear face masks during the pre-examination and triage procedures as well as the waiting for treatment.34
Fig.
The procedures of pre-examination and triage before the orthodontic practice.
Table.
Protective levels and equipment recommended for different applications
| Protective level | Protective equipment | Applications |
|---|---|---|
| Level I | Disposable surgical cap Disposable surgical mask Work clothes Disposable latex gloves Face shield if necessary | Staff working on pre-examination triage Staff working on the front desk Cleaners and security personnel |
| Level II | Disposable surgical cap Medical protective mask (N95) Work clothes Disposable surgical clothing Disposable latex gloves Goggles or face shield if necessary Waterproof boot covers | Staff working on photograph taking, impression taking, digital oral scanning, x-ray examination, and management for reusable items and medical wastes. Assistants who pass the materials and tools |
| Level III | Disposable surgical cap Medical protective mask (N95) Work clothes Hooded disposable medical isolation gown Disposable latex gloves Goggles or face shield Waterproof boot covers | Orthodontists and assistants who work closely with the patients and perform procedures that may spray or splash repository droplets, saliva, or blood while using high-speed handpieces and high-pressure 3-way syringes |
Personal protective measures
Hand hygiene
Strict hand hygiene is a simple and effective way to cut off the spread of the virus. To reinforce the compliance of hand washing, a 2-before and 3-after hand hygiene guideline is proposed. Specifically, the 2-before is to wash hands before the patient examination and before treatment procedures; the 3-after is to wash hands after touching the patient, after touching the surroundings and equipment without disinfection, and after touching the oral mucosa, blood, body fluid, and so on. In addition, orthodontic staff should avoid touching their own eyes, mouth, and nose.7 Hand hygiene should also be applied before eating as well as before and after using the bathroom to avoid the fecal-oral transmission.21
Personal protective equipment
Because droplets, contact, and aerosols are the major transmission routes of SARS-CoV-2 during orthodontic practice, barrier-protection equipment is strongly recommended for all orthodontic staff. The protective measures include wearing a disposable working cap, disposable surgical mask, working clothes, protective goggles or face shield, disposable latex gloves or nitrile gloves, and disposable isolation clothing as well as waterproof boot covers. The protective levels and equipment for different applications are recommended in the Table. Notably, the orthodontist and the assistant working in close proximity to the patient are recommended the highest level of protection and to wear hooded medical isolation clothing that covers the body as much as possible, especially during the use of high-speed handpieces and high-pressure 3-way syringes. In addition, it is recommended to wear 2 layers of latex or nitrile gloves during long practice procedures. It is critical to pay special attention to the operation of the tools, especially sharp instruments. In the case of inadvertent laceration, it would increase the risk of infection because the virus can enter the punctured skin directly and cause the infection.
The order of wear and removal of the personal protective equipment
To avoid indirect contact with contaminated protective equipment, the order of wear and removal is critical and recommended as below based on the guideline from the Handbook of COVID-19 Prevention and Treatment.36
Wear order is as follows: (1) put on work clothes and work shoes; (2) wash hands; (3) put on a disposable surgical cap; (4) put on protective facemask (or N95); (5) put on inner disposable nitrile or latex gloves (if necessary); (6) put on goggles, disposable surgical clothing (put on separate waterproof boot covers if wearing clothing without foot covers); (7) put on hooded disposable medical isolation gown (for orthodontists and first assistants) and face shield; and (8) put on outer disposable nitrile or latex gloves.
Removal order is as follows: (1) wash hands and remove visible bodily fluids or blood contaminants; (2) wash hands and replace gloves with a new pair (if 2 layers of gloves used, replace the outer gloves with a new pair); (3) wash hands and remove face shield and hooded disposable medical isolation gowns along with gloves (turn inside out, while rolling them down) (note: remove the outer gloves with clothing if 2 layers of gloves used; remove the waterproof boot covers with clothing if used); (4) wash hands and put on new gloves (if 2 layers of gloves used, replace the inner gloves with a new pair); (5) wash hands and remove goggles; (6) wash hands and remove the mask; (7) wash hands and remove the cap; (8) wash hands and remove gloves; and (9) wash hands, take a shower, put on clean clothes, and enter the clean area.
Infection controls during orthodontic procedures
During the epidemic period of the COVID-19, it is recommended to manage only orthodontic emergencies to prevent further harm, such as brackets debonding, archwire or ligature wire deformation or shifting, oral mucosa irritations, and anchorage implants loosening.37, 38, 39 Nevertheless, orthodontists or assistants should evaluate the emergencies before allowing the patients to come to the office by requesting photographs or videos from the patients. If the emergency could be managed at home by remote instructions to the patients over the phone or other communication tools, such as WeChat (Tencent, Shenzhen, China) and WhatsApp (Menlo Park, Calif), it is unnecessary for them to come to the office.33 First-visit and nonemergency return-visit patients are suggested to schedule after the COVID-19 epidemic is effectively controlled in the area. The recommendations to prevent the transmission of SARS-CoV-2 during the main orthodontic procedures were summarized as below.
Mouthrinse before orthodontic procedures
Preprocedural mouthrinse with antimicrobial agents is beneficial to reduce the salivary load of oral microbes. The commonly used chlorhexidine for mouthrinse has not been proven to be effective in disinfecting SARS-CoV-2. However, a 0.5%-1% povidone iodine solution is recommended as it has been reported to be able to disinfect SARS-CoV-1 and SARS-CoV-2.40 , 41 Because SARS-CoV-2 is vulnerable to oxidation, mouthrinse containing oxidative agents such as 1% hydrogen peroxide is also recommended.7 , 41 The patients should be instructed to swish the mouth rinse for 2-3 minutes and spit gently into a disposable cup. Saliva ejectors with low or high volume should be used to eject the gargle immediately to reduce the generation of droplets.
Photographing
Photographic records of the facial and dental images could be taken in a separate unit. For patients with high throat sensitivity, the reflector should not be placed too deep in the mouth, which may otherwise cause irritation, nausea, and vomiting, leading to the generation of droplets.42 Photographers should strictly implement the principle of “one patient, one use, and one disinfection” for auxiliary equipment such as retractors and reflectors.
X-ray examination
Although the intraoral x-ray examination is the most commonly used radiographic technique in dental practice, it can stimulate saliva secretion, gagging, and coughing.42 Direct contact to the saliva during the examination would also increase the risk of infection transmission. Therefore, extraoral radiographies, such as panoramic radiography and cone-beam computed tomography, are more appropriate alternatives during the epidemic period of COVID-19.2
Dental impression taking
Before taking the dental impression, patients should be informed of the potential risks of nausea and gagging in advance. Patients should also be instructed to inhale through the nose and exhale out the mouth. When taking the impression, the patient should wear a waterproof towel on the chest and hold a disposable cup in case of saliva splashing, or nausea and vomiting caused by throat irritation from the alginate or silicone rubber materials. It is important to avoid contamination of the devices used in mixing the alginate material by putting it on a tray. After solidification and taking out of the impression, wash the saliva or blood on the surface gently with slow running water to prevent splashing and then disinfect the impressions. Alginate and silicone rubber impressions should be disinfected by immersing in 1000 mg/L chlorine-containing disinfectants for 15-30 minutes before they are cast or sent to the factories.43 , 44
Digital oral scanning
Patients who need clear aligner orthodontic treatment and other customized appliances can obtain digital dental models through oral scanning. This approach may also help to reduce cross-infection possibilities when compared with traditional methods of alginate or silicone rubber impressions during storage and delivery. During the scanning, the staff should avoid inducing the pharyngeal reflex of the patient by gentle operation when scanning the molar regions. To avoid aerosol in the air caused by using a 3-way syringe to dry the tooth surfaces during the scanning, cotton rolls could be alternatively used to wipe the patient's tooth surfaces and keep the mouth dry by using saliva ejectors. Use the touchpad of the scanning bar to control and avoid the use of the touch screen, which may not be effectively disinfected because of its special screen characteristics. After scanning, the handle of the scanner should be sprayed and wiped with 75% alcohol. The intraoral head of the scanner should be “one patient, one use, and one disinfection.”
Treatment plan-making
For the first-visit patients, after the initial examinations and records have been taken, it is recommended to make the next appointment for return-visit on a separate day to communicate with the patients about treatment alternatives. The purpose of this is to reduce the staying time that patients are in the clinic or hospital and to avoid the potential risk of cross-infection caused by the aggregation of patients.
Bracket or attachment bonding and removal
During the treatment of the return-visit patients, especially the first-time bonding or the final removal of the appliances, the orthodontist and the assistant will be working in close proximity to the patient for an extended period. During bonding or removal of the brackets, trimming of the attachments, interproximal reduction, and so on, the staff should reduce the use of high-speed handpieces and high-pressure 3-way syringes. Low-speed handpieces or manual devices are alternatives that can be used to reduce the formation of droplets and aerosols. If high-speed handpieces are necessary to use, an anti-retraction handpiece with specially designed anti-retractive valves or other anti-reflux designs is recommended. These alternative designs have a greater reduction in the backflow of oral microbes into the waterlines of the handpiece and dental unit as compared with the handpiece without anti-retraction function.45 Nevertheless, the use of high-speed handpieces and high-pressure 3-way syringes in the patient's mouth could easily splash the saliva or blood to form aerosols. Therefore, in addition to the level III personal protective measures (Table), the use of high-volume saliva ejectors and the 4-handed or 6-handed cooperation technique should be adopted to prevent cross-infection as well as to improve working efficiency. In addition, a plasma air sterilizer should be turned on continuously for air disinfection, especially during the procedures related to the use of high-speed handpieces and high-pressure 3-way syringes, and the windows of the room should be open to allow natural ventilation. The principle of “one room, one patient, and one disinfection” should also be followed.
Archwire changing and bending
Individually packaged archwires are recommended to use in the fixed orthodontic treatment to avoid cross-infection. When the archwires need to be adjusted during the orthodontic treatment, such as the bending of 3 orders or the adding of the curve, spray and wipe the archwire with 75% alcohol after it is removed from the mouth. During the bending, 2 layers of gloves are suggested to be worn in case of glove tear or potential skin laceration from the archwires.
Removable appliance adjustment
Removable appliances, including clear aligners, are directly in contact with the saliva and the oral mucosa, making them potential transmission media of SARS-CoV-2. Appliances should be washed and sprayed with 75% alcohol or 1000 mg/L chlorine-containing disinfectants before the adjustment. Care should be taken to avoid pharyngeal reflex during wear and removal.
Disinfection of the dental settings between the treatment of patients
After the completion of 1 patient, the disinfection of dental settings and related surfaces should be done before the treatment of the next patient. The saliva ejector tubes should be flushed with at least 150 ml 1000 mg/L chlorine-containing disinfectant. The spittoon area should also be flushed and cleaned with 1000 mg/L chlorine-containing disinfectant. The handpieces and 3-way syringes should be run to discharge water for 30 seconds, which will help to flush out the patient materials that may have entered the waterlines. The dental chair should be sprayed with 75% alcohol and completely wiped and disinfected with 1000 mg/L chlorine-containing disinfectant. After disinfection, the possible touching areas of the dental setting by the orthodontist and the assistant during the treatment should be covered with a new antifouling membrane. An interval of 3-5 minutes is recommended between 2 consecutive patients to allow for optimal disinfection.
Instructions to the patient
Many aspects of orthodontic treatment require the cooperation of patients, such as the wearing and removal of the clear aligners, retainers, functional appliances, rubber band elastics, and so on. Orthodontic staff should inform the patients to incorporate proper hand hygiene before and after self-operation as well as before and after meals and defecation. Instruct the patients to use the 6-step hand washing method to avoid the transmission of the virus by contact and potential fecal-oral routes. In addition, patients who wear removable appliances should be instructed to keep the appliances stored in containers after removal rather than out on open surfaces to prevent the possible transmission of SARS-CoV-2.
Management for reusable items and medical wastes
After the practice, the reusable orthodontic instruments, such as pliers, should be pretreated, cleaned, sterilized, and properly stored in accordance with the protocol for the disinfection and sterilization of the dental instrument. Other items with high contact frequency, such as goggles, light-curing lamps, etchants, adhesive resins, elastic line, power chain, and lighters, should be sprayed with 75% alcohol and wiped with 1000 mg/L chlorine-containing disinfectant. For clear aligner attachment templates or other indirect bonding devices, 75% alcohol should also be used to spray and disinfect and then allowed to dry before preservation for future use. The medical waste generated by the treatment of patients should be stored in the specially made medical waste bags then transported and disposed of in accordance with the management requirements for medical waste.
Air and environment disinfection
Because the airborne infection is 1 of the major concerns in orthodontic practice, the disinfection and purification of the air are of great importance to prevent the spread of the COVID-19 and other microbes. Plasma air sterilizers can be left continuously running for air disinfection in an environment with human activity, especially in the working area and the waiting area. In addition, the ultraviolet light should be turned on after treatment or lunch break for environmental surface disinfection for 30-60 minutes, twice a day. If the ultraviolet light is not available, spray and wipe the surfaces, such as the floor, desk, and chair, with 1000 mg/L chlorine-containing disinfectant every 2-3 hours. In addition, natural ventilation is a simple and effective way of air purification. Under air circulation, the microbial colonies can be significantly reduced by 77.3%-79.3% within the first 30 minutes, and up to 96.4%-99.5% within 75 minutes.46
Digital patient follow-up
It is recommended to follow up with patients digitally through photographs or video calls using the phone or other communication tools, such as WeChat and WhatsApp, to not only monitor the orthodontic progress but also to minimize the repeated patient contact and ensure patient safety in case of orthodontic emergencies.33 , 47 It was reported that during the COVID-19 epidemic period, 90% of the public dental hospitals in China provided dental consultations online,3 which could also be helpful to relieve the patient anxiety caused by the suspension of the return-visit.
Conclusions
Although the COVID-19 is currently under effective control in China and many areas are gradually resuming normal activities, the increase in population mobility and the rising number of confirmed patients worldwide also pose great challenges for the prevention and control of COVID-19. Because there may still be asymptomatic patients or patients in the incubation period after the resumption of regular activities, and a large number of orthodontic patients from a widespread distribution in need of orthodontic return-visits, all procedures related to the orthodontic practice should be strictly performed with preventive measures to control the potential transmission of SARS-CoV-2. The control strategies include, but are not limited to, pre-examination and triage of patients, hand hygiene, personal protective measures, mouthrinse, reducing the use of high-speed handpieces while increasing the use of high-volume saliva ejectors during bracket or attachment bonding and removal, disinfection during archwire changing or bending and removable appliance adjustment, disinfection of dental settings between patients, instructions to patients, management of reusable items and medical wastes, air and environment disinfection, and digital patient follow-up. We must constantly bear in mind that the threat of infection is not visible, which poses a challenge on the orthodontic practice; thus, effective control measures should be taken to prevent the transmission of SARS-CoV-2 and protect both practitioners and patients from the COVID-19.
Footnotes
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and none were reported.
This review was supported by the Research and Develop Program of West China Hospital of Stomatology, Sichuan University (LCYJ2019-14).
References
- 1.World Health Organization Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) Available at:
- 2.Meng L., Hua F., Bian Z. Coronavirus Disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Y., Zhou Y., Liu X., Tan J. Health services provision of 48 public tertiary dental hospitals during the COVID-19 epidemic in China. Clin Oral Investig. 2020;24:1861–1864. doi: 10.1007/s00784-020-03267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.An N., Yue L., Zhao B. Droplets and aerosols in dental clinics and prevention and control measures of infection [in Chinese] Zhonghua Kou Qiang Yi Xue Za Zhi. 2020;55:223–228. doi: 10.3760/cma.j.cn112144-20200221-00081. [DOI] [PubMed] [Google Scholar]
- 6.Khader Y., Al Nsour M., Al-Batayneh O.B., Saadeh R., Bashier H., Alfaqih M. Dentists’ awareness, perception, and attitude Regarding COVID-19 and infection control: cross-sectional study Among Jordanian dentists. JMIR Public Health Surveill. 2020;6:e18798. doi: 10.2196/18798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Health Commission of the People’s Republic of China Guideline for the diagnosis and treatment of novel coronavirus pneumonia. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml Available at: [DOI] [PMC free article] [PubMed]
- 9.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Backer J.A., Klinkenberg D., Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill. 2020;25:2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China [in Chinese] Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Wang Y., Wang Y., Chen Y., Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures [published online March 5, 2020] J Med Virol. 2020 doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lu C.W., Liu X.F., Jia Z.F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guo Z.D., Wang Z.Y., Zhang S.F., Li X., Li L., Li C. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020 [published online April 10, 2020] Emerg Infect Dis. 2020;26 doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wax R.S., Christian M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anesth. 2020;67:568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang J., Du G. COVID-19 may transmit through aerosol [published online March 24, 2020] Ir J Med Sci. 2020 doi: 10.1007/s11845-020-02218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gu J., Han B., Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158:1518–1519. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.To K.K., Tsang O.T., Yip C.C., Chan K.H., Wu T.C., Chan J.M.C. Consistent detection of 2019 novel coronavirus in saliva [published online Feb 12, 2020] Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu R., Cui B., Duan X., Zhang P., Zhou X., Yuan Q. Saliva: potential diagnostic value and transmission of 2019-nCoV. Int J Oral Sci. 2020;12:11. doi: 10.1038/s41368-020-0080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu H., Zhong L., Deng J., Peng J., Dan H., Zeng X. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wei J., Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control. 2016;44(9 Suppl):S102–S108. doi: 10.1016/j.ajic.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahn D.G., Shin H.J., Kim M.H., Lee S., Kim H.S., Myoung J. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19) J Microbiol Biotechnol. 2020;30:313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lurie N., Saville M., Hatchett R., Halton J. Developing Covid-19 vaccines at pandemic speed. N Engl J Med. 2020;382:1969–1973. doi: 10.1056/NEJMp2005630. [DOI] [PubMed] [Google Scholar]
- 28.National Health Commission of the People’s Republic of China Guideline for the prevention and control of novel coronavirus pneumonia in medical institutes. http://www.nhc.gov.cn/yzygj/s7659/202001/b91fdab7c304431eb082d67847d27e14.shtml Available at:
- 29.National Health Commission of the People’s Republic of China Guideline for the use of medical protective equipment in the prevention and control of novel coronavirus pneumonia. http://www.nhc.gov.cn/yzygj/s7659/202001/e71c5de925a64eafbe1ce790debab5c6.shtml Available at:
- 30.Chinese Stomatological Associations Suggestions on the prevention and control of outpatient clinic treatment during the outbreak of new coronavirus pneumonia. http://www.cndent.com/archives/68495?from=timeline&isappinstalled=0 Available at:
- 31.World Health Organization Country & technical guidance - coronavirus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance Available at:
- 32.Tang H.S., Yao Z.Q., Wang W.M. Emergency management of prevention and control of the novel coronavirus infection in departments of stomatology [in Chinese] Zhonghua Kou Qiang Yi Xue Za Zhi. 2020;55:246–248. doi: 10.3760/cma.j.cn112144-20200205-00037. [DOI] [PubMed] [Google Scholar]
- 33.Caprioglio A., Pizzetti G.B., Zecca P.A., Fastuca R., Maino G., Nanda R. Management of orthodontic emergencies during 2019-NCOV. Prog Orthod. 2020;21:10. doi: 10.1186/s40510-020-00310-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not be enough. Int J Environ Res Public Health. 2020;17:2932. doi: 10.3390/ijerph17082932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cook T.M. Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic - a narrative review. Anaesthesia. 2020;75:920–927. doi: 10.1111/anae.15071. [DOI] [PubMed] [Google Scholar]
- 36.Liang T. Handbook of COVID-19 prevention and treatment. http://meghalayaonline.gov.in/covid/images/materials/handbook.pdf Available at:
- 37.Bradford C.B., Shroff B., Strauss R.A., Laskin D.M. A needle in a haystack: report of a retained archwire fragment in the pterygomandibular space. Am J Orthod Dentofacial Orthop. 2019;155:881–885. doi: 10.1016/j.ajodo.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 38.Jauhar P., Machesney M.R., Sharma P.K. Ingestion of an orthodontic archwire resulting in a perforated bowel: a case report. J Orthod. 2016;43:237–240. doi: 10.1080/14653125.2016.1201907. [DOI] [PubMed] [Google Scholar]
- 39.Umesan U.K., Ahmad W., Balakrishnan P. Laryngeal impaction of an archwire segment after accidental ingestion during orthodontic adjustment. Am J Orthod Dentofacial Orthop. 2012;142:264–268. doi: 10.1016/j.ajodo.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 40.Kariwa H., Fujii N., Takashima I. Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions, and chemical reagents. Jpn J Vet Res. 2004;52:105–112. [PubMed] [Google Scholar]
- 41.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vandenberghe B., Jacobs R., Bosmans H. Modern dental imaging: a review of the current technology and clinical applications in dental practice. Eur Radiol. 2010;20:2637–2655. doi: 10.1007/s00330-010-1836-1. [DOI] [PubMed] [Google Scholar]
- 43.Hiraguchi H., Nakagawa H., Uchida H., Tanabe N. Effect of rinsing alginate impressions using acidic electrolyzed water on dimensional change and deformation of stone models. Dent Mater J. 2003;22:494–506. doi: 10.4012/dmj.22.494. [DOI] [PubMed] [Google Scholar]
- 44.Kang Y.S., Rueggeberg F., Ramos V., Jr. Effects of chlorine-based and quaternary ammonium-based disinfectants on the wettability of a polyvinyl siloxane impression material. J Prosthet Dent. 2017;117:266–270. doi: 10.1016/j.prosdent.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 45.Hu T., Li G., Zuo Y., Zhou X. Risk of hepatitis B virus transmission via dental handpieces and evaluation of an anti-suction device for prevention of transmission. Infect Control Hosp Epidemiol. 2007;28:80–82. doi: 10.1086/510808. [DOI] [PubMed] [Google Scholar]
- 46.Fu Shaw L., Chen I.H., Chen C.S., Wu H.H., Lai L.S., Chen Y.Y. Factors influencing microbial colonies in the air of operating rooms. BMC Infect Dis. 2018;18:4. doi: 10.1186/s12879-017-2928-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dave M., Seoudi N., Coulthard P. Urgent dental care for patients during the COVID-19 pandemic. Lancet. 2020;395:1257. doi: 10.1016/S0140-6736(20)30806-0. [DOI] [PMC free article] [PubMed] [Google Scholar]