Abstract
The province of Bergamo in Italy and in particular Papa Giovanni XXIII Hospital was one of the first areas to be hit by the SARS-CoV-2 outbreak and experience firsthand all the different phases of the crisis. We describe the timeline of the changes in overall urological workload during the outbreak period from lockdown to the slow reopening of activities. We sought to compare the 2020 hospital scenario with normality in the same period in 2019, highlighting the rationale behind decision-making when guidelines were not yet available. While we focus on the changes in surgical volumes for both elective (oncological and noncancer) and urgent cases, we have still to confront the risk of untreated and underdiagnosed patients.
Patient summary
We present a snapshot of changes in urology during the peak of the COVID-19 outbreak in our hospital in Bergamo, Italy. The effect of medical lockdown on outcomes for untreated or underdiagnosed patients is still unknown.
Keywords: COVID-19, Coronavirus, Urological surgery, Pandemic
Take Home Message
A noteworthy reduction in routine clinical and surgical urology practice has been experienced during the SARS-CoV-2 outbreak. The effect of medical lockdown on outcomes for untreated or underdiagnosed patients is still unknown.
The public health emergency caused by the SARS-CoV-2 outbreak rapidly spread from China to the entire world and pandemic status was declared by World Health Organization (WHO) on March 11, 2020 [1]. The first COVID-19 patient at Papa Giovanni XXIII Hospital in Bergamo was diagnosed on February 23, 2020 [2]. Our hospital is the tertiary referral center for the province of Bergamo, with nearly 900 active beds. Within 10 d from the first COVID-19 diagnosis, all the beds available in the respiratory unit and the infectious diseases department were full and six more COVID-19 wards were created, for a maximum of 326 beds. A total of 88 beds were occupied in the emergency room (ER), and beds in the intensive and sub-intensive care units were expanded from 70 to 100 (Table 1 ) [3]. From the start of the outbreak up to April 29, 2020, more than 2700 patients admitted to the ER for COVID-19 disease-related symptoms had a positive swab; of those, 1850 patients (68,5%) were admitted to COVID-19 wards. Reallocation of anesthesiologists from elective surgery management to acute COVID-19 patient care, the need to dedicate beds, nurses, and medical personnel to the new COVID-19 wards, and the concomitant reduction in health care personnel who were infected led to dramatic changes in routine clinical and surgical practice [2].
Table 1.
Comparison between the standard bed arrangement and the situation on March 23, 2020, at the peak of the crisis.
| Pre-COVID-19 situation | Situation during the COVID-19 surge |
||
|---|---|---|---|
| Mean beds used per day in 2019 | Beds used for non-COVID-19 | Beds used for COVID-19 | |
| Emergency medicine | 11.7 | 0 | 22 |
| Medicine department (adults) | 272.7 | 81 | 301 |
| Surgical department (adults) | 262.5 | 99 | 0 |
| Sub-intensive care | 16.8 | 0 | 12 |
| Intensive care | 47.5 | 12 | 76 |
| Pediatric department | 79.8 | 66 | |
| Other departments | 67.7 | 32 | |
| (A) Total beds used | 758.7 | 290 | 411 |
| Emergency department | |||
| Area for overflow treatment | 0 | 15 | |
| Temporary observation | 10 | 42 | |
| Resuscitation room | 4 | 6 | |
| (B) Total beds used | 14 | 63 | |
| Overall beds used (A + B) | 772.7 | 290 | 474 |
Our busy urology department typically has 40 beds and is normally staffed by 13 full-time urologists. There is daily activity across three operating rooms (ORs) for 15 surgical sessions per week and various inpatient and outpatient activities. More than 500 major cancer procedures, 400 transurethral resections of the bladder, 600 prostate biopsies, >2000 cystoscopies, and >15 000 outpatient medical examinations are performed annually.
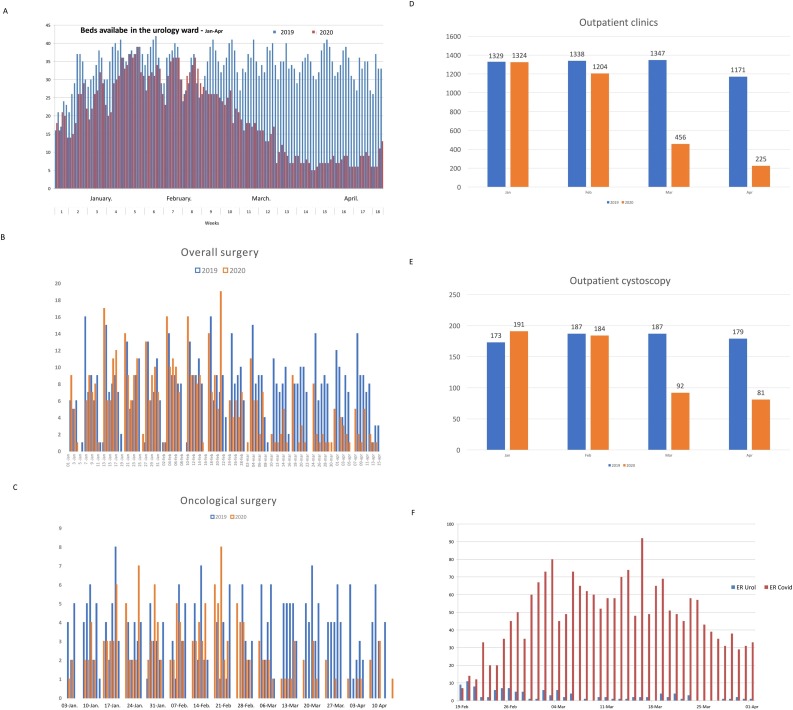
Here we report the timeline of changes in overall urological activities during the outbreak period in terms of both inpatient and outpatient volumes, and compare the same period in 2019 and 2020 (February 15–April 30). Starting from February 22, 2020, the number of beds available for urology decreased from 40 to 20 (50%) within 2 wk, and no more than ten beds were dedicated to urological pathology after March 15 (25%). At that time, no national or international urological guidelines or recommendations were available to direct decision-making.
Comparison of the same time interval for 2019 and 2020 revealed a 65% drop in ward admittance (2626 vs 1192 patients; Fig. 1 A). Similarly, urological ORs were reduced from three per day to one per day within the following 2 wk, and after March 5 only two ORs per week were available. This resulted in a dramatic 75% reduction in overall surgical procedures compared to the same period in 2019: 108 surgical procedures were performed in 2020, compared to 445 in 2019, between March 5 and April 20 (Fig. 1B). In particular, there was a 67% reduction in oncological procedures: 55 oncological procedures were performed in 2020 compared to 171 in 2019 (Fig. 1C). We decided to prioritize surgery for bladder cancer (radical cystectomy and transurethral resection for high-risk cases) and locally advanced kidney cancer (cT3–4), as well as for testicular and highly suspicious adrenal cancer, a choice supported by subsequently published national and international urology guidelines [4], [5]. Given this strategy, all patients in this high-priority group were treated, except for those needing intensive care, as the unit was full with COVID-19 patients. Campi et al [6] retrospectively analyzed the proportion of high-priority major cancer surgery cases at three Italian academic urological centers. According to their results, up to 68% of uro-oncologic surgical procedures can be postponed during times of emergency, including high-risk prostate cancer, which typically represents nearly 40% of all radical prostatectomies. We decided to give these surgeries lower prioritization, given that a delay of up to 12 mo seems to not alter operative and cancer-specific outcomes or, at least, other treatment modalities can be considered [4], [5]. So, which patients are we still missing?
Fig. 1.
(A) Beds occupied between January and April in 2019 and 2020 for urological patients. Distribution of (B) overall and (C) oncological surgery in the period from January to April in 2019 and 2020. (D,E) Reduction in outpatient and cystoscopy activity during the COVID-19 outbreak crisis. (F) Access to the emergency room for COVID-19 disease and for urological disease.
A delay in cancer treatment can be a major concern. However, the risk of delay in the diagnosis of cancer or other life-threatening conditions is just as important, if not even more so. Our department decided to keep outpatient clinics open (with a 50% reduction) for any emergency consultation, all oncological patients requiring a urological evaluation, and patients with high-risk non–muscle-invasive bladder cancer within the first year of follow-up who were scheduled for cystoscopy. However, 25% of these patients preferred to postpone their office visit or failed to attend their consultation (Fig. 1D,E) owing to concern about entering a COVID-19 contaminated area or for correlated health issues. Moreover, prostate biopsies (with a high-risk prostate cancer detection rate of 16% in our 2019 database; data unpublished) were completely discontinued in these 2 mo of the crisis and still have not resumed to date.
Because the ER was almost entirely dedicated to assisting COVID-19 patients and was full up to April 20, 2020, we observed a reduction in urological emergencies during the crisis (Fig. 1F). However, the number of ward admissions from the ER for urological conditions and the number of patients undergoing typically urgent surgical treatment remained stable (Supplementary Table 1). How can this be explained? We can assume that patients admitted to the ER were only those who really required treatment, while patients with less demanding symptoms who would normally have used the ER, preferred to stay away from the hospital and avoid the risk of contamination. Another possibility is that some patients might have been unable to reach the hospital because of the lockdown status and the lack of ambulances and other emergency vehicles. As smaller hospitals in the region completely shut down their urological departments, we still have no answer to this.
The progressive reduction in new COVID-19 cases from April 20, 2020 relieved pressure on the hospital organization and was followed by the new scenario of stepwise reopening of surgical and clinical activities. In this respect, in a tertiary referral center that will remain a COVID-19 hub because of central decisions, the challenge is to correctly balance the need to start again with the likely possibility of facing a second wave of the disease. As urologists, we are now facing the need to reorganize the surgical mix according to the ORs available. From April 10 to May 1, three urological ORs were available, with a plan to increase to one OR a day from May 4, 2020. Oderda et al [7] calculated that the waiting time for uro-oncological procedures is estimated to double by the end of April or triple by the end of June 2020. However, many non-oncological procedures require careful assessment and cannot be deferred indefinitely. At the same time, we need to develop different strategies for outpatient consultations to reduce direct and potentially dangerous access to the hospital and ensure the safety of patients and health care personnel [8]. The COVID-19 scenario has revolutionized our traditional approach to urological waiting lists and stratification of priorities. Most questions regarding the real overall impact on outcomes remain unanswered as it is too early to evaluate the medium-term effects of a medical lockdown. It seems likely that this unprecedented scenario will change our management practice in the future, especially once we finally understand what happened to the missing patients.
Author contributions: Marco Roscigno had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Roscigno, Naspro.
Acquisition of data: Muttin, Angiolilli.
Analysis and interpretation of data: Roscigno, Piccichè.
Drafting of the manuscript: Roscigno, Naspro.
Critical revision of the manuscript for important intellectual content: Da Pozzo, Deiana, Pezzoli.
Statistical analysis: Piccichè.
Obtaining funding: None.
Administrative, technical, or material support: None.
Supervision: None.
Other: None.
Financial disclosures: Marco Roscigno certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: None.
Acknowledgments
The authors would like to thank the entire staff of the Urology Department and the Crisis Unit of Papa Giovanni XXIII Hospital, Bergamo.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.euf.2020.05.022.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Sohrabi C., Alzafi Z., O’Neill N. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naspro R., Da Pozzo L.F. Urology in the time of corona. Nat Rev Urol. 2020;17:251–253. doi: 10.1038/s41585-020-0312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buoro S., Di Marco F., Rizzi M. Papa Giovanni XXIII Bergamo Hospital at the time of the COVID -19 outbreak: letter from the warfront. Int J Lab Hematol. 2020 doi: 10.1111/ijlh.13207. [DOI] [PubMed] [Google Scholar]
- 4.Ficarra V., Novara G., Abrate A. Urology practice during COVID -19 pandemic. Minerva Urol Nefrol. 2020 doi: 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed] [Google Scholar]
- 5.Stensland K.D., Morgan T.M., Moinzadeh A. Considerations in the triage of urologic surgeries during the COVID-19 pandemic. Eur Urol. 2020;77:663–666. doi: 10.1016/j.eururo.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campi R., Amparore D., Capitanio U. Assessing the burden of nondeferrable major uro-oncologic surgery to guide prioritisation strategies during the COVID -19 pandemic: insights from three Italian high-volume referral centres. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.03.054. S0302-2838(20)30229-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oderda M., Roupret M., Marra G., et al. The impact of COVID-19 outbreak on uro-oncological practice across Europe: which burden of activity are we facing ahead? Eur Urol. In press. https://doi.org/10.1016/j.eururo.2020.04.036. [DOI] [PMC free article] [PubMed]
- 8.Boehm K., Ziewers S., Brandt M.P., et al. Telemedicine online visits in urology during the COVID-19 pandemic—potential, risk factors, and patients’ perspective. Eur Urol. In press. https://doi.org/10.1016/j.eururo.2020.04.055. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.