Abstract
Teleneurology in Spain had not been implemented so far in clinical practice, except in urgent patients with stroke. Telemedicine was hardly used in epilepsy, and patients and neurologists usually preferred onsite visits. Our goal was to study impressions of adult and pediatric epileptologists about the use of telemedicine after emergent implementation during the new coronavirus 2019 (COVID-19) pandemic.
Methods
An online survey was sent to the members of the Spanish Epilepsy Society and the members of the Epilepsy Study Group of the Catalan Neurological Society, inquiring about different aspects of telemedicine in epilepsy during the pandemic lockdown.
Results
A total of 66 neurologists responded, mostly adult neurologists (80.3%), the majority with a monographic epilepsy clinic (4 out of 5). Of all respondents, 59.1% reported to attend more than 20 patients with epilepsy (PWE) a week. During the pandemic, respondents handled their epilepsy clinics mainly with telephone calls (88%); only 4.5% used videoconference. Changes in antiseizure medications were performed less frequently than during onsite visits by 66.6% of the epileptologists. Scales were not administered during these visits, and certain types of information such as sudden expected unrelated death in epilepsy (SUDEP) were felt to be more appropriate to discuss in person. More than 4 out of 5 of the neurologists (84.8%) stated that they would be open to perform some telematic visits in the future.
Conclusions
In Spain, emergent implantation of teleneurology has shown to be appropriate for the care of many PWE. Technical improvements, extended use of videoconference and patient selection may improve results and patient and physician satisfaction.
Keywords: Telemedicine, Teleneurology, Epilepsy, Adult, Pediatric
1. Introduction
In Spain, teleneurology had not been implemented in routine clinical practice so far except in some areas such as stroke, particularly in islands and territories remote from specialized centers [1]. Telemedicine was hardly used in epilepsy, and patients and neurologists preferred onsite visits in spite of the potential feasibility of remote visits, especially for stable chronic patients [2].
However, the COVID-19 crisis has obliged health administrators and physicians to adopt and implement this system in a very short time to maintain patient care during the pandemic [3]. The aim of the study was to determine the perceptions of Spanish epileptologists practicing telemedicine during the COVID-19 pandemic lockdown.
2. Methods
An online survey was sent to the members of the Spanish Epilepsy Society (April 14th, 2020) and the members of the Epilepsy Study Group of the Catalan Neurological Society (April 24th, 2020). The survey remained open until May 11th, 2020.
We inquired about the features of their epilepsy clinics, type of technology used during the remote visits, type of information given to the patients and therapeutic changes performed, time taken compared with the onsite visits, and willingness (epileptologists and patients) to continue with telemedicine in the future. The study was approved by the Ethics Committee of our hospital.
3. Results
The questionnaire was answered by 66 epileptologists. Most of them (80.3%) were adult neurologists, whereas 19.7% were pediatric neurologists. Of the respondents, 56% reported having had some type of experience with telemedicine visits in the past, while 44% reported no previous experience, so they had to start using this system because of the lockdown in the context of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV)-2 pandemic.
The great majority of neurologists handled their epilepsy clinics through telephone calls (88%). About 8% of epileptologists reported having seen some patients onsite and contacted others by phone. Only 4.5% reported having used videoconference systems to contact their patients (see Table 1 ).
Table 1.
Results of the survey.
| Survey items | n (%) |
|---|---|
| Age group of the respondents | |
| 25–35 yo | 5 (7.5) |
| 35–45 yo | 26 (39.4) |
| 45–55 yo | 21 (31.8) |
| > 55 yo | 14 (21.2) |
| Epilepsy clinic | |
| Monographic epilepsy clinic | 53 (80.3) |
| No monographic epilepsy clinic | 13 (19.7) |
| Direct care to patients with COVID-19 in addition to their neurology tasks | |
| Yes | 25 (37.9) |
| No | 41 (62.1) |
| Number of patients with epilepsy attended per week | |
| < 10 | 4 (6.1) |
| 10 to 20 patients | 23 (34.8) |
| > 20 patients | 39 (59) |
| Video-EEG available as a diagnostic tool in their facilities | 56 (84.4) |
| Changes in antiseizure medications (type or dose) during visits | |
| Less frequently than during onsite visits | 42(63.6) |
| Similar frequency to onsite visits | 24 (36.4) |
| Duration of remote visits | |
| Shorter time than onsite visits | 37 (56.1) |
| Similar time than onsite visits | 24 (36.4) |
| Longer time than onsite visits | 5 (7.6) |
| Administrative support to organize remote visits | |
| Support | 35 (53) |
| Self-organization | 31 (47) |
| Technical difficulties to communicate with the patients | |
| Sometimes | 22 (33.3) |
| Frequently | 5 (7.6) |
| Never | 6 (9.1) |
| Rarely | 33 (50) |
| Future teleneurology visits for patients with epilepsy | |
| Convinced to use in telemedicine | 22 (33.3) |
| Open to telematic visits in the future | 34 (51.52) |
| Preferred face-to-face visits | 6 (9.1) |
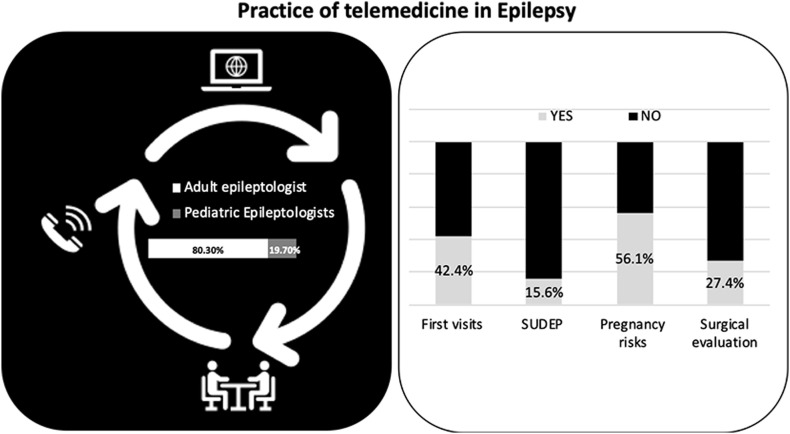
We specifically asked about first visits: of the respondents, 42.4% performed first visits also with telemedicine, while a significant percentage (38%) preferred to postpone them to see the patients onsite after the end of the lockdown period.
Care provided during the telemedicine visit was appropriate and enough in the majority of patients. Half of the epileptologists reported that they rarely had to reschedule the patient for an onsite follow-up. The most frequent reason to schedule another visit was the need for blood work, electroencephalogram (EEG), or neuroimaging to decide about diagnosis or treatment. The next most frequently reported reason for rescheduling (21%) was the need to perform a neurological examination onsite.
Most neurologists (90%) had to provide over the phone information regarding results of EEG or neuroimaging tests, and most believed that the patients understood it correctly. We also assessed if other types of sensitive information were provided to the patients. Of all respondents, 56.1% provided information about pregnancy risks over the phone in women of childbearing potential, while 43.9% felt that type of information should be given during an onsite visit. Regarding sudden expected unrelated death in epilepsy (SUDEP), the great majority (84.4%) reported that they preferred that discussion to be held with the patient and family during a normal visit (Fig. 1 ).
Fig. 1.
Types of attention in medicine. Telemedicine in epilepsy was used for patients with a first visit by almost half of the respondents. First visits were done by the phone by 40% of the respondents. More than 50% felt comfortable informing about pregnancy risks in a non-face-to-face way but only 1 out of 4 epileptologists found telemedicine useful to give information about surgical evaluation and only 15% about SUDEP.
Almost 60% of the respondents had an epilepsy surgery program in their hospital. Only 27.4% of them had to explain the results of the surgical evaluation over the phone. Of those, only 62.5% felt the patient had understood the information correctly.
A majority of the responders (83.3%) reported not having administered any questionnaires (quality of life, adverse effects, depression, etc.) over the phone or by videoconference.
Almost all the participants had the electronic medical record used by their hospitals available while they contacted their patients; however, 30.3% reported not having access to the common electronic medical record (the one containing all medical information of one patient, including data from different medical centers). Almost 20% could not make electronic prescriptions from their computers at the time they attended the patients.
When asked about patients' impressions, 78.8% of respondents stated that some patients would like to have this type of telephone/videoconference follow-up in the future. Only 10% felt that very few patients would be interested in this system.
4. Discussion
All over the world, the COVID-19 pandemic has forced hospitals to dedicate facilities and staff to the attention of infected patients. Depending on the specific needs of the institutions, neurologists have been asked to integrate into COVID teams, usually with support from infectious disease physicians [4]. However, the regular, nonemergent attention of neurological patients has continued over the last two months [5]. Since lockdown in Spain came into force [6], onsite visits were converted to telemedicine visits. Our survey shows the impressions of the epileptologists dealing with this new type of care.
In our country, most of the visits have been done over the phone. That contrasts with other countries such as the US where more hospitals are equipped with telematic platforms able to connect patients and physicians not only with audio but also video [7]. Many of the restrictions concerning the use of these platforms with medical information have been lifted during the pandemic. Videoconference was only used by a minority of the neurologists responding this survey because most healthcare facilities could not offer these platforms with such short notice. Videoconference, however, may be more convenient to reinforce the relationship with patients and to perform the neurological examination [8]. It is likely that if this type of attention continues in the future and if video is available, more neurologists will take on also first visits in this way. In our survey, however, up to 38% of neurologists decided to postpone first visits to be able to establish personal contact and get to know their new patients. The feeling that onsite visits could be more appropriate to discuss delicate issues such as pregnancy-related risks or SUDEP is reflected in the high number of epileptologists that did not speak of these during telephone visits. It is unclear whether the use of teleconference would change that. The technical requirements also will have to include remote access to electronic prescriptions and shared common medical records. In addition, the exchange of online material such as scales that the patients could fill in and send back should be possible to complete care. Coding and reimbursement will not be such a problematic issue in Spain as it is in other countries as the US. In the European Union (EU), Germany and France have already initiated the legislation to use the telemedicine [9,10]. Clinical trials to prove the use of telemedicine have been increasingly registered in the last 10 years but usually in other fields than neurology [11]. In 2011, the EU had already mentioned the rights of patients to receive health attention within its borders [12]; telemedicine could facilitate a better medical attention for European citizens.
In general, the performance of telephone visits was very good. Most patients did not need to be rescheduled and when so, the most frequent reason was the need for additional diagnostic tests to make a decision, which would have happened anyway during onsite visits. Information regarding tests was felt to be understood, with less patients seemingly understanding completely the results of presurgical evaluation. This is a complex issue that probably is more adequate to be done onsite to be able to transmit better the risk and benefit balance of the surgical procedure.
Antiseizure medications were changed less often than during regular visits. However, this can be attributed mainly to the hospital situation during the pandemic, which made physicians very cautious about introducing new drugs to diminish the possibility of adverse reactions or seizure worsening requiring a visit to the emergency room.
In any case, most of our respondents felt that telemedicine is a possibility for the future, 84.8% felt open to attend some patients in this way, and most thought that they even saved time doing this type of visits. The survey showed that the most likely groups to benefit from this strategy of follow-up included patients with well-controlled epilepsy on stable doses of medication, patients with intellectual disability, or patients with difficult mobility or driving restrictions who live remotely and usually depend on family members to travel. Patients participating in clinical trials who do not require specific procedures such as blood work or diagnostic tests may also benefit from this [13].
In summary, the emergent implantation of telemedicine in epilepsy in Spain has shown that remote visits, even using only telephone, may be appropriate for a significant part of patients with epilepsy. The care of our chronic patients could benefit even more if video systems are installed and more complete access to electronic records and online scales is granted. Patients with epilepsy may have a wider experience with e-tools for seizure counting and with seizure detection devices, so they may be friendlier to technology than other neurology patients [14]. It is perceived that some patients would agree to be controlled in this way in the future [15]. Prospective studies evaluating outcome of these patients compared with patients who are attended onsite would be helpful to establish the effectiveness of this type of remote care.
Funding
There are no funders to report for this submission. ECB was supported by fellowship grant RH041910.
Declaration of competing interest
All authors declare no conflicts of interest related to this study.
Acknowledgments
The authors thank the Spanish Epilepsy Society and the Epilepsy Study Group of the Catalan Neurological Society.
References
- 1.Mutgi S.A., Zha A.M., Behrouz R. Emerging subspecialties in neurology: telestroke and teleneurology. Neurology. 2015;84(22):e191–e193. doi: 10.1212/WNL.0000000000001634. [DOI] [PubMed] [Google Scholar]
- 2.Kissani N., Lengané Y.T.M., Patterson V., Mesraoua B., Dawn E., Ozkara C. Telemedicine in epilepsy: how can we improve care, teaching, and awareness? Epilepsy Behav. 2020;103(Pt A) doi: 10.1016/j.yebeh.2019.106854. [DOI] [PubMed] [Google Scholar]
- 3.Klein B.C., Busis N.A. COVID-19 is catalyzing the adoption of teleneurology. Neurology. 2020 doi: 10.1212/wnl.0000000000009494. [DOI] [PubMed] [Google Scholar]
- 4.Manji H., Carr A.S., Brownlee W.J., Lunn M.P. Neurology in the time of covid-19. J Neurol Neurosurg Psychiatry. 2020;91(6):568–570. doi: 10.1136/jnnp-2020-323414. [DOI] [PubMed] [Google Scholar]
- 5.Grossman SN, Han SC, Balcer LJ, Kurzweil A, Weinberg H, Galetta SL, et al. Neurology May 2020, 10.1212/; DOI: 10.1212/WNL.0000000000009677. [DOI] [PubMed]
- 6.Legido-Quigley H., Mateos-García J.T., Campos V.R., Gea-Sánchez M., Muntaner C., McKee M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Heal. 2020;5(5):e251–e252. doi: 10.1016/S2468-2667(20)30060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatcher-Martin J.M., Adams J.L., Anderson E.R., Bove R., Burrus T.M., Chehrennama M. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology. 2020;94(1):30–38. doi: 10.1212/WNL.0000000000008708. [DOI] [PubMed] [Google Scholar]
- 8.Janssen F., Awadallah M., Alhalabi A., Körber B., Lang R., Scibor M. Telemedicine in general neurology: use of audiovisual consultation for on call back-up service in an acute care hospital. J Neurol. 2018;265(4):880–884. doi: 10.1007/s00415-018-8756-4. [DOI] [PubMed] [Google Scholar]
- 9.Brauns H.J., Loos W. Telemedizin in Deutschland: Stand – Hemmnisse – Perspektiven. Bundesgesundheitsblatt - Gesundheitsforsch - Gesundheitsschutz. 2015;58(10):1068–1073. doi: 10.1007/s00103-015-2223-5. [DOI] [PubMed] [Google Scholar]
- 10.Ohannessian R., Yaghobian S., Chaleuil M., Salles N. Télémédecine en France: revue des essais cliniques enregistrés entre 2000 et 2015. Eur Res Telemed. 2016;5(2):29–36. [Google Scholar]
- 11.ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US)https://clinicaltrials.gov/ct2/results?term=Neurology&cond=Telemedicine. Search of: Neurology | Telemedicine - List Results - ClinicalTrials.gov.
- 12.Union EP-OJ of the E, 2011 undefined. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients' rights in cross-border healthcare.
- 13.Wechsler L.R. Advantages and limitations of teleneurology. JAMA Neurol. 2015;72(3):349–354. doi: 10.1001/jamaneurol.2014.3844. [DOI] [PubMed] [Google Scholar]
- 14.Ryvlin P., Beniczky S. Seizure detection and mobile health devices in epilepsy: update and future developments. Epilepsia. 2018;59:7–8. doi: 10.1111/epi.14088. [DOI] [PubMed] [Google Scholar]
- 15.Dorsey E.R., Glidden A.M., Holloway M.R., Birbeck G.L., Schwamm L.H. Teleneurology and mobile technologies: the future of neurological care. Nat Rev Neurol. 2018;14(5):285–297. doi: 10.1038/nrneurol.2018.31. [DOI] [PubMed] [Google Scholar]