Abstract
Objective:
To describe the variability in: 1) the contributions of 3D hip and knee kinematics to the dynamic knee valgus (DKV) movement pattern during a single limb squat in women with patellofemoral pain; and 2) the 3D strategies used to reduce DKV following an intervention.
Methods:
Secondary analysis of a feasibility study investigating a movement training intervention. In 23 participants, 2D knee frontal plane projection angles (FPPA) and 3D hip and knee frontal and transverse plane angles at peak knee flexion were calculated during a single limb squat at pre- and post-intervention, and the change in 2D and 3D angles computed. 3D angles at pre-intervention were summed for each participant to create cumulative bar graphs. Similar graphs were created for change in 3D angles. For visual comparison, graphs were ordered by increasing knee FPPA or change in knee FPPA.
Results:
The knee FPPA decreased from a mean of 7.2 degrees (SD: 7.1) to a mean of −8.9 degrees (SD: 8.9) following the intervention. A large portion of DKV, and change in DKV, was due to hip adduction and knee lateral rotation, yet participants with similar knee FPPA and change in knee FPPA, displayed variation in all 3D components and change in 3D components.
Conclusion:
People who demonstrate similar observed movement patterns during a weight-bearing task may use different 3D strategies for execution.
Keywords: 2-dimensional, Frontal Plane Projection Angle, movement patterns, musculoskeletal
INTRODUCTION
Movement impairments are possible contributors to pain or injury in diagnoses such as patella-femoral pain (PFP) (Powers, 2010). A common movement impairment in women with PFP is dynamic knee valgus (DKV), where the knee collapses inward during weight bearing activities (Powers, 2003). This particular movement impairment is characterized by varying degrees of increased hip adduction, hip medial rotation, knee abduction, and knee lateral rotation.
Different approaches have been used to quantify DKV during a variety of tasks. Three-dimensional (3D) motion analysis has been used to assess individual 3D hip and knee joint kinematics, and altered kinematics have been detected in individuals with PFP using this methodology (Nakagawa, Moriya, Maciel, and Serrão, 2012; Salsich and Long-Rossi, 2010; Willson and Davis, 2008a). Yet, two-dimensional (2D) motion analysis has become a more commonly utilized tool for assessing the DKV movement pattern due to its being more cost-effective, less time intensive and having greater availability in the clinical setting. In particular for PFP, 2D motion analysis focuses on the knee frontal plane projection angle (knee FPPA). There are reported 2D video analyses that have moderate to strong correlations with 3D frontal plane measures of the knee during the task of the single limb squat (Gwynne and Curran, 2014; Herrington et al., 2017). Yet, the 2D knee FPPA is not a result of a single joint, single plane motion. It is derived from various 3D components of both the hip and knee, and relationships between the knee FPPA and these 3D components are less clear (Herrington et al., 2017; Scholtes and Salsich, 2017). Understanding the primary drivers of DKV may provide insight into subject-specific mechanisms of pain development.
Reducing DKV is a target for interventions, and preliminary evidence suggests that a task-specific movement training program may be effective in reducing 3D kinematic components of DKV (Salsich et al, 2018), but it is not clear how patients achieve a more optimal movement pattern. Understanding the variation in kinematic strategies used to decrease DKV may inform movement-based treatment approaches and help identify treatment responders. The purpose of this paper is to describe the variability in: 1) the contributions of individual 3D hip and knee kinematics to the DKV movement pattern during a single limb squat in women with patellofemoral pain; and 2) the 3D strategies that are used to reduce DKV following intervention.
METHODS
This descriptive secondary analysis was based on data from a prospective, non-randomized, within-group, double baseline, feasibility intervention study (Salsich et al., 2018). This original study was approved by the Institutional Review Board at Saint Louis University (protocol #24433), and written informed consent was obtained from each participant.
Participants
In the original study, full data sets were analyzed on 23 females with patellofemoral pain (Salsich et al., 2018). This population is characterized by the following: mean age of 21.7 years (SD: 3.5), mean BMI of 22.3 (SD: 2.1), mean pain duration of 4.3 years (SD: 3.5) (Salsich et al., 2018).
The following inclusion and exclusion criteria were verified by the principal investigator, a physical therapist, during a clinical screening examination of the knee joint. As part of the initial phone screening, an 11-point numeric pain scale was used to ensure participants had an average daily pain of at least 3/10 and pain duration of greater than 2 months. The clinical screening was used to evaluate the location of the source of pain. Participants had to have pain originating from the patellofemoral articulation (behind or around the patella) (Salsich et al., 2018). Palpation was performed by the principal investigator to rule out pain originating from the patellar tendon, quadriceps tendon, tibiofemoral joint, menisci or synovial plicae. Pain also had to be reproduced by at least two of the following tests: resisted quadriceps contraction, single limb squat, and step down (Salsich et al., 2018). During the in person screening, pain was documented via a visual analog scale a 100-mm line with a left anchor of “no pain” and a right anchor of “worst imaginable pain” to confirm the presence of pain in response to the 3 provocation tests.
Females with PFP had to demonstrate observable dynamic knee valgus during a single limb squat test on the involved, most painful limb to be an appropriate candidate for the intervention. A total of approximately 5 trials were observed by an experienced physical therapist. These trials were observed in real-time and were not recorded via camera. The participant was classified as having “observable dynamic knee valgus” if in the majority of trials the frontal plane knee angle increased by 10 degrees or more in the descent phase of the squat (Salsich et al., 2018). As shown previously, visual assessments of knee FPPA are reliable and are in agreement with quantitative FPPA change (Harris-Hayes et al., 2014).
Exclusion criteria for these participants included the following: body mass index (BMI) greater than 30 kg/m^2 due to kinematic methodology; a history or current report of knee ligament, tendon or cartilage injury; patellar instability or dislocation; prior knee surgery; known pregnancy; and neurological involvement that would influence movement patterns (Salsich et al., 2018).
Assessments
In the original study, participants were assessed at: Baseline; 6 weeks (pre-intervention); 12 weeks (post intervention); and 16 weeks. For each assessment, participants completed questionnaires to assess: pain (Visual Analog Scale); function (Patient-Specific Functional Scale) (Chatman et al., 1997); and activity level (Habitual Physical Activity Test) (Baecke, Burema, and Frijters, 1982; Salsich et al., 2018). In addition, 3-dimensional kinematic data and 2-dimensional video data were obtained during 5 movement tasks (i.e. ascend stairs, descend stairs, single limb squat, sit to stand and stand to sit). For the purposes of this paper we focus on the task of single limb squat and report the kinematic and video data from the pre-intervention and post-intervention time points for the 23 participants who completed the study.
Intervention
The intervention was led by a certified orthopaedic clinical specialist physical therapist with 24 years of experience who delivered the intervention in twelve 45 minute sessions (2x/week for 6 weeks). This intervention emphasized the principals of motor skill learning and consisted of supervised repetitive practice of functional daily tasks with a focus on maintaining optimal limb alignment during movement (Salsich et al., 2018).
Participants were trained in 2-3 tasks specific to their sport, leisure or work activities as well as 4 common pain provoking activities: 1) single limb squats; 2) double limb squats; 3) standing up from/ sitting down in a chair; and 4) ascending/descending stairs (Salsich et al., 2018). During all tasks participants were instructed to keep their hip, knee and ankle in line to avoid dynamic knee valgus and keep their shoulders and pelvis level during these tasks. The intensity of these exercises progressed when participants were able to maintain proper alignment without increasing pain. Gradations of each task were developed to accommodate the individual capabilities of each participant and to allow for improvements and progression in each task over time (e.g. increasing step height, adding external load, and increasing running speed). However, the intensity was decreased if it could not be performed at the given difficulty due to increased pain or incorrect movement (Salsich et al., 2018). As part of a home program, participants were instructed to incorporate optimal movement into all daily activities and to complete five repetitions of 2-3 tasks each day to reinforce the key concepts of optimal movement (Salsich et al., 2018).
Data Collection and Processing
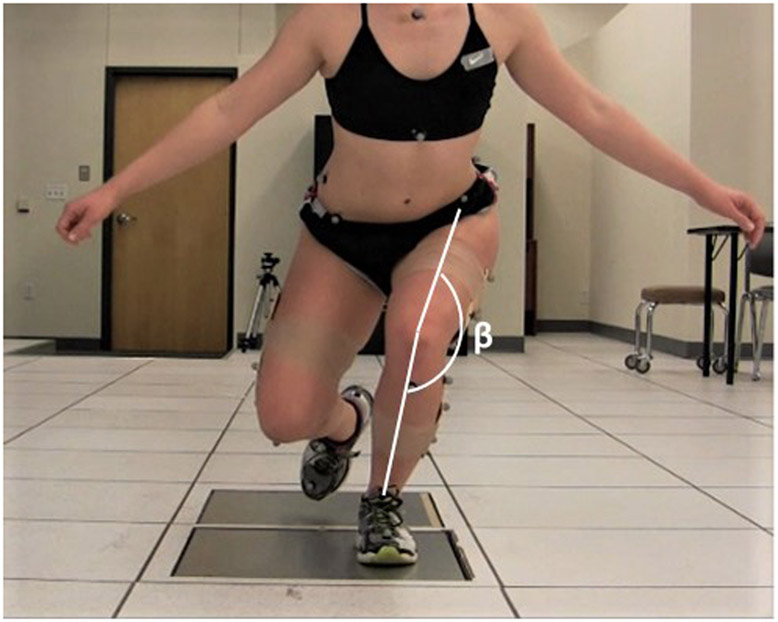
As previously described, 2D and 3D data were captured simultaneously during a single limb squat. 3D data were captured using an 8-camera, motion analysis system (Vicon, Oxford Metrics LTD. Oxford, England) sampled at 120 Hz and previously established methods (Salsich et al., 2018). Retro-reflective markers were placed by a single investigator on the pelvis and lower extremities bilaterally as follows: iliac crest, anterior superior iliac spine, posterior superior iliac spine, medial and lateral femoral epicondyles 4-marker thigh cluster, medial and lateral malleoli, 4-marker shank cluster, tibial tuberosity, fibular head, posterior calcaneus, 2nd toe (dorsum), 1st and 5th metatarsal heads, midfoot dorsum, lateral aspect of the calcaneus. Figure 1 provides a visual for this marker set that was used in the original study.
Figure 1.

The marker set used in the original study.
A 6-degrees-of-freedom model defined a set of coordinate axes for the pelvis, thigh, shank and foot. For the pelvis, the CODA model (Charnwood Dynamics Ltd., UK) was used. For each segment, the frontal plane was defined first. The frontal plane of the thigh was defined by the hip joint center (proximal endpoint) and the two femoral epicondyle markers (distal end) (Bell and Pedersen, 1990). The frontal plane of the shank in the original study was defined by the thigh distal endpoint (proximal end) and the two malleolus markers (distal end). While the frontal plane of the foot was defined by the two malleolus markers (proximal end) and the projection on the floor of the two malleolus markers (distal end). The local coordinate system of each segment was located at the proximal endpoint of each segment. The frontal plane defined the orientation of the x-axis (sagittal plane rotation). The z-axis (transverse plane rotation) was aligned so that it passed through the proximal endpoint and the distal endpoint of the segments. The y-axis (frontal plane rotation) was oriented orthogonal to both x and z axes.
For this secondary analysis, the tibial tuberosity and fibular head markers, which were redundant and unused markers in the original study, were used with the two malleolus markers to define the orientation of the x-axis (sagittal plane rotation) and y-axis (frontal plane rotation) of the shank; the z-axis (transverse plane rotation) was defined by the intersection of frontal and sagittal planes (Cappozzo, Catani, Della Croce, and Leardini, 1995). Comparing the two shank models using our 23 participants, the updated shank model positioned the knee joint, on average, in 12.3 degrees (SD: 5.6) more lateral rotation at peak knee flexion during a single limb squat than the shank model used in the original study. The updated shank model allows for better visualization in the cumulative bar graphs (described below) of the contribution of knee lateral rotation (a positive value) to DKV because the knee is not biased toward medial rotation (a negative value) as it is with the original shank model.
Following marker placement, a static standing trial was captured followed by 3 trials of a single limb squat on the involved or most painful limb. Participants started in full knee extension. They were instructed to complete the squat cycle from the start of knee flexion back to full knee extension in ~4 seconds and were allowed several practice trials until they became accustomed to the task (typically ~ 3 trials). Data were processed using Visual3D^TM software. The a priori kinematic variables of interest were the hip adduction angle (+ Hip Y), hip medial rotation angle (+ Hip Z), and knee lateral rotation angle (+ Knee Z) at the time of peak knee flexion. The knee abduction angle (+ Knee Y) at peak knee flexion was included in this analysis to fully describe the 3D kinematic components of DKV. Knee abduction and lateral rotation as defined by the right-hand rule were originally negative, but the values were negated so that all variables associated with DKV would be positive. Kinematic variables were averaged over the 3 trials for each time point. The average change in joint angle from pre- to post-treatment was calculated as the post-treatment value minus the pre-treatment value.
Between-day intra-rater reliability of the 3D frontal and transverse plane kinematic variables were calculated using the intraclass correlation coefficient (ICC(3,3)) (Shrout and Fleiss, 1979). Data on 11 female subjects were collected on two occasions, an average of 6.4 days (SD: 1.6) apart using the mean of 3 trials from each day. Standard error of measurement (SEM) was estimated from the ICCs. Between-day reliability ranged from ICC(3,3) (SEM) of 0.65 (3.0 degrees) to 0.79 (2.5 degrees). Within-session trial-to-trial variability calculated across 3 trials has been previously published (Salsich, Graci, and Maxam, 2012). Within-session ICC(3,1) (Shrout and Fleiss, 1979) ranged from 0.89-0.98. SEMs ranged from 1.0 degrees to 2.0 degrees.
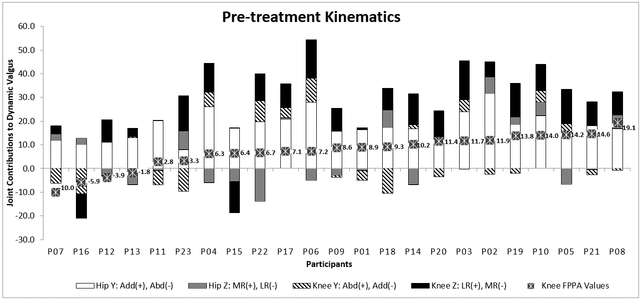
Two-dimensional data were captured during the squat trials using a Canon VIXIA HF M50 Video Camera (Canon U.S.A, Inc. Huntington, NY) or Bonita 720C Video Camera (Vicon, Oxford Metrics LTD. Oxford, England) positioned at a height of 45 cm, 3 meters anterior to the participant. The data collected were processed using Dartfish ProSuite 7 (Dartfish, Switzerland). Two-dimensional knee FPPA was used as a method of quantifying dynamic knee valgus. The knee FPPA was measured at peak knee flexion, determined visually by one investigator, by drawing a line from the Anterior Superior Iliac Spine (ASIS) of the involved limb down through the midpoint of the knee and then another line from the midpoint of the knee to the midpoint of the ankle. The knee FPPA was then calculated as 180 degrees minus the angle formed by a line bisecting the femur and a line bisecting the tibia (Figure 2). Increasing angles (positive Knee FPAA values) corresponded to increasing dynamic knee valgus. The angle measurements were averaged across the 3 trials for each time point, and the average change in angle from pre- to post- treatment was calculated as the post-treatment value minus the pre-treatment value.
Figure 2.
The 2D knee frontal plane projection angle (knee FPPA = 180 – ∣β∣)
Intra-rater reliability of knee FPPA measures was established by measuring angles on 15 randomly selected, masked videos, on two occasions approximately 1 week apart. A fixed-effects model, ICC(3,1), was used because the effect of the single rater was assumed to be fixed (Shrout and Fleiss, 1979). The intra-class correlation coefficient (ICC(3,1)) was 0.948. Inter-rater reliability was established between two investigators who measured the same 15 angles on one occasion. A mixed-effects model, ICC(2,1), was used because the effect of raters was assumed to be random (Shrout and Fleiss, 1979). The ICC(2,1) value was 0.993.
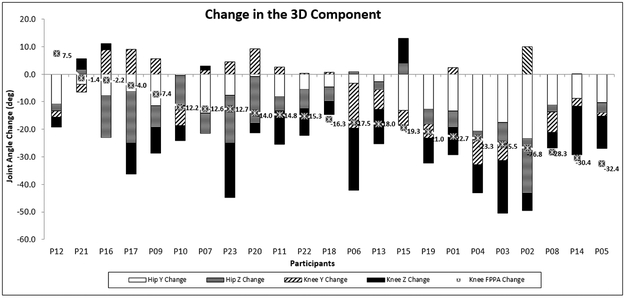
For each participant, cumulative bar graphs were constructed using the 3D kinematics. Separate graphs were constructed for angles at pre-treatment and for the change in angles between pre- and post-treatment. Using pre-treatment values, a composite graph was created by plotting individual participant cumulative bar graphs in order of increasing knee FPPA. Another composite graph was created using the change values from pre- to post-treatment to plot individual cumulative bar graphs in order of increasing change in knee FPPA.
RESULTS
As a result of the intervention both 2D and 3D kinematics changed considerably. The knee FPPA decreased from a mean of 7.2 degrees (SD: 7.1) to a mean of −8.9 degrees (SD: 8.9) following the intervention. Furthermore, the 3D kinematics for hip adduction, hip medial rotation, and knee lateral rotation all improved following the intervention (Salsich et al., 2018). Movement speed during the squat was similar for the pre- and post-intervention time points (Mean Pre: 3.6 seconds (SD: 0.9); Mean Post: 4.2 seconds (SD: 1.2).
In Figure 3, each cumulative bar graph represents the 3D components that comprise the 2D knee FPPA during a single limb squat. A large portion of the 3D movement pattern exhibited by these participants was due to hip adduction (+ Hip Y) and knee lateral rotation (+ Knee Z). Yet, each participant still displayed a unique compilation of 3D components to achieve DKV. Some participants even exhibited hip lateral rotation (− Hip Z) and knee adduction (− Knee Y) while demonstrating positive 2D FPPA values during squatting.
Figure 3. Pre-treatment 3D kinematics for each participant listed in the order of increasing 2D knee FPPA.
Each stacked column represents a participant’s 3D angle compilation during peak knee flexion of the single limb squat. Contributors of dynamic knee valgus include: hip adduction (Add): (+ Hip Y), hip medial rotation (MR): (+ Hip Z), knee abduction (Abd): (+ Knee Y), and knee lateral rotation (LR): (+ Knee Z).
Figure 4 compares two participants at the pre-intervention time point. Participants P04 and P15 exhibited variability among the 3D components while both had nearly identical knee FPPA values (6.3 and 6.4 respectively). Their 3D movement pattern was composed of varying amounts of Hip Y, Knee Y, and Knee Z. Participant P15 exhibited hip adduction (+ Hip Y), slight knee abduction (+ Knee Y), and knee medial rotation (− Knee Z), whereas P04 exhibited greater hip adduction (+ Hip Y), greater knee abduction (+ Knee Y) and knee lateral rotation (+ Knee Z).
Figure 4. A pre-treatment comparison of 3D kinematics for participants, P04 and P15.
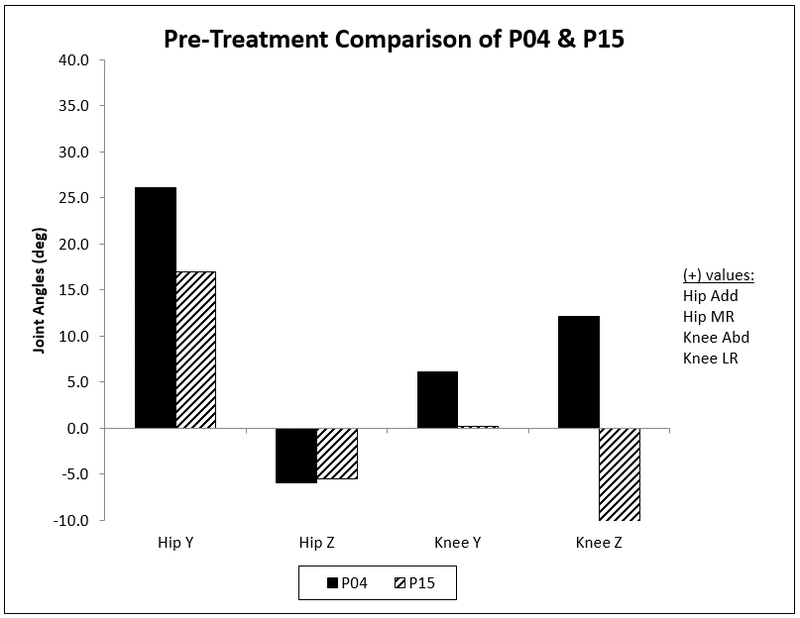
The knee FPPA pre-treatment values are respectively, 6.3 degrees (P04) and 6.4 degrees (P15). Positive values represent Hip Y: adduction (Add), Hip Z: medial rotation (MR), Knee Y: abduction (Abd), and Knee Z: lateral rotation (LR).
In Figure 5, each cumulative bar graph depicts the change in 3D components between pre- and post-intervention time points, and the graphs are ordered by the change in knee FPPA values between the same time points. All participants but one showed a decrease in the knee FPPA following intervention. The majority of change in 3D kinematics was due to a change in Hip Y (decrease in hip adduction), Knee Z (decrease in knee lateral rotation), and Hip Z (decrease in hip medial rotation) while the least amount of change noted was due to Knee Y (decrease in knee abduction).
Figure 5. Change in 3D kinematics for each participant, listed in the order of increasing change in 2D knee FPPA.
Each stacked column is a composite of a participant’s change in kinematics at peak knee flexion of the single limb squat between pre- and post-intervention. The change in 3D components equals the post-treatment values minus the pre-treatment values. Contributors of dynamic knee valgus include: hip adduction (+ Hip Y), hip medial rotation (+ Hip Z), knee abduction (+ Knee Y), and knee lateral rotation (+ Knee Z). A negative change in each variable indicates a reduction in dynamic knee valgus.
Figure 6 takes a closer look at two participants with varying amounts of change in the 3D components but similar pre-treatment knee FPPA values and change in knee FPPA. Participants P02 and P03 exhibited pre-treatment knee FPPA values of 11.9 degrees and 11.7 degrees, respectively, and their amount of change for the knee FPPA between time points was 26.8 degrees (P02) and 25.5 degrees (P03). However, the change in their 3D components varied across the individual joints. Both participants changed similarly with respect to Hip Y with both starting at high amounts of hip adduction and decreasing 73%. Yet following the intervention P02’s levels of − Knee Y (knee adduction) remained unchanged while P03 changed from + Knee Y to − Knee Y (knee adduction). Both P02 and P03 ultimately decreased their levels of + Knee Z (knee lateral rotation), but only P03 achieved − Knee Z (knee medial rotation) following the intervention.
Figure 6. Comparison of the 3D kinematics of P02 and P03 from pre- to post-treatment.
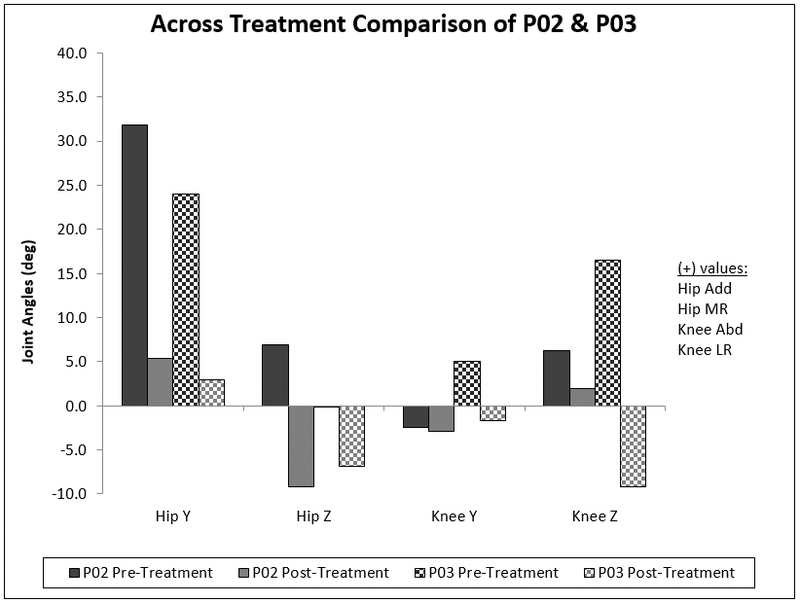
Original pre-treatment knee FPPA values are 11.9 degrees (P02) and 11.7 degrees (P03). Post-treatment knee FPPA values are −14.9 degrees (P02) and −13.8 degrees (P03). The change in knee FPPA for both participants is respectively, 26.8 degrees (P02) and 25.5 degrees (P03). Positive values represent Hip Y: adduction (Add), Hip Z: medial rotation (MR), Knee Y: abduction (Abd), and Knee Z: lateral rotation (LR).
DISCUSSION
These findings suggest that even though participants may satisfy the visual criteria for a diagnosis of DKV (e.g. during screening as described above), or move similarly during a weight bearing task from a 2D perspective, they can still demonstrate a broad variation in 3D kinematics. The 3D strategies used by these participants to decrease DKV also exhibited considerable variability, in that the change in the magnitude of individual joint kinematics was different across subjects. This DKV movement pattern, while driven largely by hip adduction, still revealed different 3D profiles across participants, which might explain why previous investigators found low to moderate associations between the knee FPPA and individual 3D segment or joint kinematics (Herrington et al., 2017; Scholtes and Salsich, 2017; Willson and Davis, 2008a). Scholtes and Salsich (2017) reported knee FPPA correlations ranging from 0.04 (3D knee abduction) to 0.42 (3D hip adduction) in women with patellofemoral pain who performed a single limb squat. Similarly, Willson and Davis (2008b) reported correlations ranging from 0.01 (tibial external rotation) to 0.61 (femoral adduction) in a similar population during the same task. Collectively, our findings and those of previous investigators suggest that visual classification or 2D measures of DKV, while indicative of the presence and/or magnitude of the DKV movement pattern, cannot illuminate the specific joint or segment contributions to the pattern.
Several study limitations should be noted. The study sample was fairly homogenous and consisted of women who were relatively young, healthy, and active. Thus these results may not be generalizable to all people with PFP. However, young women with DKV are a large subgroup of people with PFP, and thus are important to this study. Another limitation is that the 3D kinematic results may have been influenced by the error associated with repeated marker placement. Although mean differences in the kinematics were detected despite marker placement error (Salsich et al., 2018), this error could have influenced the variability in individual kinematics presented in this manuscript.
Following intervention, the 2D movement pattern (knee FPPA) improved an average of 16.1 degrees, and as reported previously, the 3D components of hip adduction, hip medial rotation and knee lateral rotation also improved (Salsich et al., 2018). The improved knee FPPA indicates that the DKV movement pattern decreased following intervention, consistent with previous findings obtained after a single session of instruction (Scholtes and Salsich, 2017). However, the amount of change in the individual 3D kinematics varied widely across participants, with hip adduction being the only variable that was consistently reduced in every participant following the intervention. The change in hip adduction angle ranged from a decrease of 0.43 degrees to a decrease of 23.4 degrees; hip medial rotation change ranged from a 4.2 degrees increase to a 19.7 degrees decrease; knee abduction change ranged from a 10.0 degrees increase to a 16.4degrees decrease; and knee lateral rotation change ranged from a 8.9 degrees increase to a 22.5 degrees decrease. From these findings it is clear that although both 2D and 3D kinematics improved, no single joint or segment rotation is solely responsible for improvement in knee FPPA values during the single limb squat.
It is difficult to use the amount of change in 2D knee FPPA to discern the amount of change in 3D kinematics. As depicted in Figure 5, the participants with the largest amounts of 2D change did not necessarily show the greatest degree of 3D change. Sources of error, possibly due to variability in soft tissue architecture or differences in sagittal plane movement pre- to post-intervention could have influenced the 2D knee FPPA. However, knee flexion angles were similar between the pre-intervention (mean: 78.0 degrees, SD: 5.6 degrees) and post-intervention (mean: 77.7 degrees, SD: 7.3 degrees) time points. Thus it does not appear that sagittal plane motion confounded the effect of the intervention on the 2D knee FPPA. Rather, participants appeared to use a variety of 3D strategies to accomplish the goal of reducing DKV.
The intervention included in the study consisted solely of high-repetition practice of daily tasks, with a focus on optimal limb alignment during movement. Participants were instructed to keep their knee in line with their hip and ankle and keep their pelvis level, but were able to choose their own strategy for accomplishing this task. All participants “chose” to reduce hip adduction, possibly because the instructions addressed both the pelvis and femur in the frontal plane, however they did so to varying degrees and utilized a variety of additional 3D strategies at the hip and knee to accomplish the same goal of DKV reduction. By choosing their own strategy this may have helped result in a wide array of 3D profiles post-treatment. More specific instructions targeted at isolated joints and planes may have resulted in a more consistent 3D profile. Nonetheless, pain and function improved on average following the movement training intervention (Salsich et al., 2018), so perhaps more specific movement instructions are not necessary to yield positive outcomes for most individuals. That said, there might be specific subgroups that need more targeted approaches. For example, P21 had one of the highest FPPA values pre-treatment (14.6 degrees) (Figure 2), and had a negligible change post-treatment (decreased 1.4 degrees) (Figure 4). This participant also had minimal improvement in hip adduction and knee abduction, while worsening with respect to hip medial rotation and knee lateral rotation. Perhaps additional instruction to keep the thigh turned out, for example, would have resulted in greater kinematic improvements for this individual. Further research is necessary to determine if more exact instruction would result in greater kinematic improvement and more consistent 3D profiles among participants. Additionally, structural alignment factors (e.g. foot pronation, tibial rotation, and femoral anteversion) may have limited the improvement of the DKV movement pattern in some participants, and thereby contributed to the variability in movement profiles observed.
CONCLUSION
Participants with PFP who were visually classified as having DKV demonstrated variable 3D hip and knee kinematic profiles during a single limb squat, even among participants who had similar 2D knee FPPA. Knee FPPA improved following a task-specific movement training intervention, however the amount of change in individual 3D kinematics varied across participants, even among those who exhibited a similar change in 2D knee FPPA, suggesting that people who demonstrate similar observed movement patterns and change in movement patterns during a weight-bearing task may use different 3D strategies to accomplish the task. Overall, while 2D kinematics provide useful clinical information, knowledge of the 3D kinematics is beneficial for understanding the contributions of individual joints to the overall movement pattern.
Footnotes
Declaration of Interest
The authors declare no conflict of interest.
REFERENCES
- Baecke JA, Burema J, Frijters JER 1982. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. American Journal of Clinical Nutrition 36: 936–942. [DOI] [PubMed] [Google Scholar]
- Bell AL, Pedersen DR 1990. A comparison of the accuracy of several hip center location prediction methods. Journal of Biomechanics 23: 617–621. [DOI] [PubMed] [Google Scholar]
- Cappozzo A, Catani F, Della Croce U, Leardini A 1995. Position and orientation in space of bones during movement. Clinical Biomechanics 10: 171–178. [DOI] [PubMed] [Google Scholar]
- Chatman AB, Hyam SP, Neel JM, Binkley JM, Stratford PW, Schomberg A, Stabler M 1997. The Patient-Specific Functional Scale: Measurement properties in patients with knee dysfunction. Physical Therapy 77: 820–829. [DOI] [PubMed] [Google Scholar]
- Gwynne CR, Curran SA 2014. Quantifying frontal plane knee motion during single limb squats: Reliability and validity of 2-dimensional measures. International Journal of Sports Physical Therapy 9: 898–906. [PMC free article] [PubMed] [Google Scholar]
- Harris-Hayes M, Steger-May K, Koh C, Royer NK, Graci V, Salsich GB 2014. Classification of lower extremity movement patterns based on visual assessment: Reliability and correlation with 2-dimensional video analysis. Journal of Athletic Training 49: 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrington L, Alenezi F, Alzhrani M, Alrayani H, Jones R 2017. The reliability and criterion validity of 2D video assessment of single leg squat and hop landing. Journal of Electromyography and Kinesiology 34: 80–85. [DOI] [PubMed] [Google Scholar]
- Nakagawa TH, Moriya ÉT, Maciel CD, Serrão FV 2012. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. Journal of Orthopaedic and Sports Physical Therapy 42: 491–501. [DOI] [PubMed] [Google Scholar]
- Powers CM 2003. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. Journal of Orthopaedic and Sports Physical Therapy 33: 639–646. [DOI] [PubMed] [Google Scholar]
- Powers CM 2010. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. Journal of Orthopaedic and Sports Physical Therapy 40: 42–51. [DOI] [PubMed] [Google Scholar]
- Salsich GB, Graci V, Maxam DE 2012. The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. Journal of Orthopaedic and Sports Physical Therapy 42: 1017–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salsich GB, Long-Rossi F 2010. Do females with patellofemoral pain have abnormal hip and knee kinematics during gait? Physiotherapy Theory and Practice 26: 150–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salsich GB, Yemm B, Steger-May K, Lang CE, Van Dillen LR 2018. A feasibility study of a novel, task-specific movement training intervention for women with patellofemoral pain. Clinical Rehabilitation 32: 179–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholtes SA, Salsich GB 2017. A dynamic valgus index that combines hip and knee angles: Assessment of utility in females with patellofemoral pain. International Journal of Sports Physical Therapy 12: 333–340. [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL 1979. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin 86:420–428. [DOI] [PubMed] [Google Scholar]
- Willson JD, Davis IS 2008a. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clinical Biomechanics 23: 203–211. [DOI] [PubMed] [Google Scholar]
- Willson JD, Davis IS 2008b. Utility of the frontal plane projection angle in females with patellofemoral pain. Journal of Orthopaedic and Sports Physical Therapy 38: 606–615. [DOI] [PubMed] [Google Scholar]