Abstract
Introduction and hypothesis
Understanding patient preferences regarding provider characteristics is an under-explored area in urogynecology. This study aims to describe patient preferences for urogynecologic care, including provider gender, age, experience, and presence of medical trainees.
Methods
This was a multicenter, cross-sectional, survey-based study assessing patient preferences with a voluntary, self-administered, anonymous questionnaire prior to their first urogynecology consult. A 5-point Likert scale addressing provider gender, age, experience, and presence of trainees was used. Descriptive statistics summarized patient characteristics and provider preferences. Chi-squared (or Fisher’s exact) test was used to test for associations.
Results
Six hundred fifteen women participated from eight sites including all geographic regions across the US; 70.8% identified as white with mean age of 58.5 ± 14.2 years. Urinary incontinence was the most commonly reported symptom (45.9%); 51.4% saw a female provider. The majority of patients saw a provider 45–60 years old (42.8%) with > 15 years’ experience (60.9%). Sixty-five percent of patients preferred a female provider; 10% preferred a male provider. Sixteen percent preferred a provider < 45 years old, 36% preferred 45–60 years old, and 11% of patients preferred a provider > 60 years old. Most patients preferred a provider with 5–15 or > 15 years’ experience (49% and 46%, respectively). Eleven percent preferred the presence of trainees while 24% preferred trainee absence.
Conclusion
Patient preferences regarding urogynecologic providers included female gender and provider age 45–60 years old with > 5 years’ experience. Further study is needed to identify qualitative components associated with these preferences.
Keywords: Female pelvic medicine and reconstructive surgery, Gender, Medical learners, Patient preferences, Training, Urogynecology
Introduction
The Obstetrics and Gynecology (OB/GYN) workforce has shifted greatly from being male-dominated to female predominant. In 1973, only 10% of OBGYN faculty were women compared with 53% in 2012 [1]. An article by Neubardt in 1974 discussed female patients’ dissatisfaction with the medical field and the need for female gynecologists [2]. Since then, the field of OB/GYN has dramatically changed and now has the highest proportion of female residents (81% in 2012) [3].
A variety of studies have been performed over the last 20 years to determine factors that are considered when women are choosing an OB/GYN provider, and the data are conflicting on gender preferences [4-7]. In other medical specialties, female patients do not seem to have such a gender preference, and in certain surgical specialties, the majority of female patients have no gender preferences, citing other attributes such as reputation, skill, and patient-centered approach as being the most important considerations [8-10].
Little is known regarding patient preferences related to physician gender or age in the gynecologic subspecialties or for particular obstetrical or gynecologic conditions. As with the OB/GYN workforce, the gynecologic subspecialty workforce is becoming increasingly female. It was reported that 46% of urogynecology subspecialists were female in 2015 with predictions of 81% being female by 2045 [11]. As this emerging subspecialty grows, the age and experience of its providers will shift as well.
Most of the rapport that a physician has with the patient is created in the office setting. In an academic institution, it is common to have medical students, residents, and fellows participate in the care of a patient. In various settings, patients reported satisfaction with their interactions with trainees of all levels [12-14]. This is contrasted by literature in OB/GYN where male medical students are denied opportunities to be involved in patient care [15]. By being denied these important opportunities to build patient rapport, male medical students may be missing a vital component of their education, and this can affect future career goals. Currently, there is no evidence in the gynecologic subspecialties regarding patient preference for trainees.
The objective of this cross-sectional study was to investigate patient preferences regarding characteristics of urogynecologic providers as well as preferences for medical trainees in this setting.
Methods and materials
This multicenter, cross-sectional survey-based study was conducted through the Fellows’ Pelvic Research Network (FPRN). The FPRN is a US multicenter research consortium of Female Pelvic Medicine and Reconstructive Surgery fellows, overseen by the Society of Gynecologic Surgeons and the American Urogynecologic Society. This study included eight clinical sites which encompassed all geographic regions in the US as defined by the US Census Bureau. Institutional Review Board approval was obtained at each institution. This study was conducted between February 15, 2018, and August 15, 2018.
Patient preferences were assessed with a voluntary, self-administered, anonymous questionnaire prior to the patient’s first urogynecology patient consult. These questionnaires were completed in the waiting room prior to the patient being brought back to the examination room or being introduced to their urogynecology provider. Inclusion criteria included female patients, presenting for a new patient consultation for urogynecologic care, age > 18, and ability to read and understand English or Spanish. Patients were considered new if this was their first visit seeking urogynecologic care at that particular center. Patients were asked to seal their completed surveys in an envelope and place them in a locked box prior to their visit with their provider. No incentive or compensation was provided to the participant for the completion of this brief survey.
The questionnaire was designed by the authors with the assistance of experts in survey design. Urogynecology attendings and fellows provided feedback which was used to refine the survey. The survey was available in English and Spanish. Demographic variables ascertained included patient age, race, highest level of education, as well as which urogynecologic symptom(s) brought them to the office. Patients expressed preference for provider gender, age, experience, and presence of medical trainees on a 5-point Likert scale from “very much prefer” to “very much do not prefer.” Age, gender, and years of experience of the urogynecologic provider were recorded. Provider age was divided into three categories: < 45 years old, 45–60 years old, and > 65 years old. Years in practice were divided into three categories: < 5 year of experience, 5–15 years of experience, and > 15 years of experience. The survey also inquired about the effect of each of these factors on the quality of care they are receiving. In a similar fashion, responses were also ranked on a 5-point Likert scale from “very much affects” to “very much does not affect.” In addition, there was a free-text response question asking patients to state their reason for their preferences (Appendix A). Patients were able to indicate a preference for multiple groups, for example, by indicating they “very much prefer” a provider age 45–60 as well as “slightly prefer” a provider age > 60 years. Therefore, not all responses are mutually exclusive. The questionnaire was administered without any contact by research staff.
Using existing data on patient preference in general OB/GYN, it was estimated that 50% of patients would prefer female urogynecology providers [6]. With the estimated sample size of 385, a two-sided 95% confidence interval for a single proportion using the large sample normal approximation will extend 0.05 from the observed proportion of 50%.
Responses from the written surveys were entered into a REDCap [16] electronic data capture tool hosted at the University of Alabama at Birmingham. The primary investigator at each site entered their data into a centralized database. Patient demographics and provider characteristics were summarized using descriptive statistics (mean and standard deviation for continuous variables; frequency and percentage for categorical variables). Patient preference factors in Likert scale were reported using a bar chart. Associations of patient age, race, and education with urogynecologist care preferences were evaluated with chi-square or Fisher’s exact tests, as appropriate.
To analyze the qualitative response, the text was normalized by removing numbers, punctuations, stop words, extra whitespaces, and special characters and then switching all to lower case. Text mining using the term frequency-inverse document frequency (TF-IDF) index [17, 18] was performed to determine the relative importance of a word to a document (i.e., response). The TF-IDF is the product of term frequency (TF) and document frequency (DF). TF refers to how frequently a term appears in one document. The TF is then divided by the document length. DF is the number of documents that contain the term. The IDF is derived by taking the logarithm of the total number of documents divided by the number of documents where the specific term appears. A word cloud [19] was plotted to summarize the average TF-IDF index for each term with varying importance.
A p value < 0.05 was considered statistically significant in two-tailed statistical tests. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC), and graphical presentation was generated using R 3.4.4.
Results
A total convenience sample of 615 women participated in this study. The mean age was 58.5 ± 14.2 years, and 70.8% (429/606) identified their race as white (Table 1); 42.5% (260/612) of women achieved a college degree or higher level of education. The highest represented geographic area was the West (37.7%, 232/615), and the least represented was the Northeast (9.9%, 61/615). Urinary incontinence was the most commonly reported primary symptom as the reason for the consultation (45.9%, 278/606) followed by pelvic organ prolapse (28.9%, 175/606) although most patients (50.4%, 310/615) presented with more than one symptom. These additional symptoms included pelvic pain (9.6%, 58/606) and fecal incontinence (3.3%, 20/606); 51.4% (303/589) of patients saw a female provider at their initial visit. The majority of patients saw a provider 45–60 years old (42.8%, 252/589) with > 15 years of experience (60.9%, 359/589) (Table 2).
Table 1.
Patient demographics
| Demographics | All (n = 615) N (%) |
|---|---|
| Age (mean ± SD) | 58.49 ± 14.9 |
| < 45 years | 83 (16.6) |
| 45–60 years | 167 (27.2) |
| > 60 years | 251 (40.8) |
| Race | |
| White | 429 (70.8) |
| African American | 42 (6.9) |
| Hispanic | 101 (16.7) |
| Other | 34 (5.6) |
| Education | |
| No or some high school | 50 (8.2) |
| High school diploma | 89 (14.5) |
| Some college/Associate degree | 213 (34.8) |
| Bachelor degree | 140 (22.9) |
| Postgraduate degree | 120 (19.6) |
| Geographic region | |
| West | 232 (37.7) |
| Midwest | 96 (15.6) |
| South | 226 (36.8) |
| Northeast | 61 (9.9) |
SD = standard deviation
Table 2.
Provider characteristics
| Demographics | All (n = 615) N (%) |
|---|---|
| Provider age (mean ± SD) | |
| < 45 years | 166 (28.2) |
| 45–60 years | 252 (42.8) |
| > 60 years | 171 (29) |
| Provider gender | |
| Male | 286 (48.6) |
| Female | 303 (51.4) |
| Provider years of experience | |
| < 5 years | 135 (22.9) |
| 5–15 years | 96 (16.3) |
| > 15 years | 359 (60.9) |
SD = standard deviation
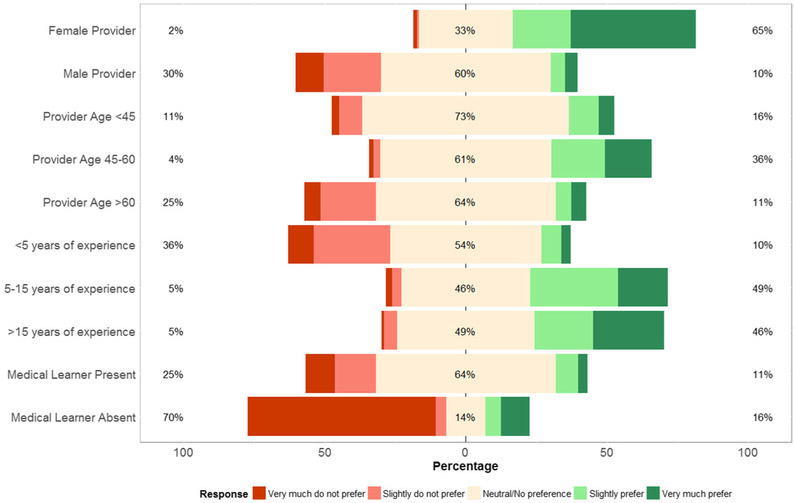
When patients were asked to select three important characteristics related to provider age, provider gender, provider experience, and medical trainees, the most commonly selected factors were female provider (73.3% 362/494), 5–15 years of experience (54%, 267/494), and provider age 45–60 years old (37.7%, 186/494). Sixty-five percent (373/576) of patients preferred a female provider, and 10% (50/519) preferred a male provider. There was no significant association among patient age, race, or education level and preference for provider gender (all p > 0.05). Sixteen percent (80/500) of patients preferred a provider < 45 years old, 36% (189/532) preferred a provider 45–60 years old, and 11% (54/500) preferred a provider > 60 years old. Most patients preferred a provider with 5–15 or > 15 years of experience (49%, 251/515; 46%, 235/513, respectively). Patients tended to choose providers within their own age group (p = 0.02). Eleven percent (58/512) of patients preferred the presence of trainees while 24% (122/508) preferred their absence (Fig. 1). Although most patients had no preference for the presence of trainees, women with a higher education level preferred the absence of trainees (p = 0.01). Geographic region was significantly associated with provider gender, age, and years of training. More patients preferred female providers in the West, South, and Northeast than the Midwest (p < 0.01). A higher proportion of patients in the South preferred that their provider be < 60 years old (p = 0.02). Patients in the South and Northeast preferred providers with ≥ 15 years of experience (p < 0.01).
Fig. 1.
Patient preference factors in Likert scale for Female Pelvic Medicine and Reconstructive Surgery Care
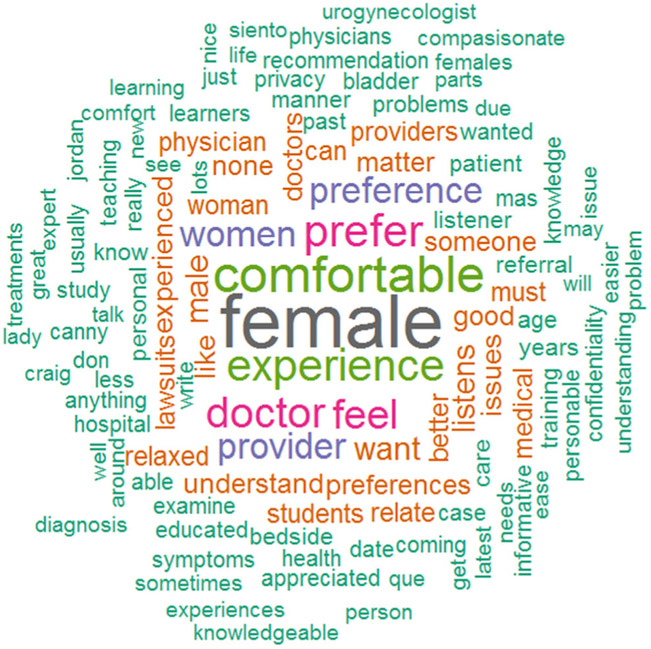
The majority of patients were scheduled with their FPMRS provider based on a physician referral (61.9%, 354/572) or first available appointment (17.7%, 101/572). There were 192 patients (31.2%) who completed the free-text portion of the survey which related to the reason for their preferences. The text analysis result revealed that patient preferences were commonly due to listening, understanding, experience of the provider, and the feeling of being comfortable with a female provider. Examples of comments include “A doctor who spends time explaining and listening well,” “I like doctors with experience but not so old that they no longer are studying or researching latest practices,” and “I feel more comfortable and secure with a female provider.”
Discussion
This study showed that a convenience sample of women in the US seeking urogynecologic subspecialty care had a preference for provider gender, experience, age, as well as a preference for trainees. Of the women with a preference for gender, a majority preferred female providers. However, less than a third of patients preferred not to see a male provider. While this topic was previously not studied in gynecologic subspecialties, these results differ from previous work in general obstetrics and gynecology, which was mixed regarding provider gender preference [4-7]. Patients preferred that their providers be 45–60 years old and have at least 5 years of experience. A quarter of patients preferred not to have trainees, with the current study showing that more years of education was associated with a preference to not have medical learners. Most patients scheduled their appointment with a specific urogynecologic provider based on a referral from their doctor, and many considered recommendations from friends and online reviews.
Qualitative descriptions of patient preferences revealed considerations of bedside manner, listening, empathy, experience, and the feeling of being comfortable with a specific provider gender. We did not see a significant association among patient age, race, or education level and their preference for provider gender. While empirically it was presumed these patient characteristics would be associated with their preferences, this study was not powered specifically to look at this association. However, patients tended to choose providers within their own age group (p = 0.02). Although most patients had no preference for the presence of trainees, with increased education level, more patients preferred the absence of trainees (p = 0.01). Patients expressed a preference against male over female trainees twice as often (31.8 vs. 13.7%), which is in line with previous evidence in the OB/GYN literature where male medical students were denied opportunities to be involved in patient care [15].
In this era of patient satisfaction, it is important to consider factors which help to improve patient experience and meet patients’ needs. The results of this study suggest that, if possible, a large gynecologic subspecialty practice should consider including providers of both genders of various ages and experience. Furthermore, given that a proportion of patients prefers to not have trainees involved in their care, practices should potentially consider discussing trainee involvement as part of the patient scheduling process. Practices could consider specific in-office materials which highlight benefits of trainees of which patients may not be aware. While every effort should be made to provide learning opportunities for trainees regardless of gender, awareness of patient preferences will allow for more sensitivity to the patient experience. The alternative would be for the patient to seek care at a non-academic practice.
Limitations of this study should be acknowledged. Although patients’ location, age, race, education level, and primary symptom were representative of the population in the US as well as those presenting for urogynecologic care, all of the practices sampled had academic affiliations and thus may not be representative of practices in a community setting. The northeast area of the country was disproportionately under-represented. Timing of the survey prior to appointments was selected to minimize bias. However, it is possible patients were aware of the gender, experience, or age of their provider while filling out the questionnaire which may have influenced their responses. The survey was completed privately and placed in a sealed envelope after completion, but it is possible patients were influenced by the social desirability of their responses. As this survey was administered anonymously without any contact by research staff, some patients may have elected to not answer every question. It is also possible that the referring provider may have introduced bias by referring the patient to a particular urogynecologic provider. Furthermore, while the questionnaire was designed with consideration of previous work and utilized experts in study design, the questionnaire was not validated prior to administration.
Despite these limitations, this study is of a geographically, educationally, and ethnically diverse sample of American women who represent the population seeking care with a urogynecologic provider at an academic institution and fills a void in the literature regarding an understanding of their preferences. Patients who spoke English and Spanish were included, which further enhances the generalizability. Providers of all age, experience, and genders were represented. This study provides insight into the attitudes of patients with pelvic floor disorders and may help guide providers, medical centers, and offices increase awareness of patient preferences.
Patients’ preferences regarding urogynecologic providers included female gender and provider age 45–60 years old with > 5 years of experience. Understanding the factors that influence patients’ expectations and experience is vital in creating an environment that serves their needs. Further study is needed to identify qualitative components associated with these preferences.
Supplementary Material
Fig. 2.
Word cloud plot representing qualitative response in patient preference. The font size corresponds to the relative importance of each term in the response. The most influential words are the largest
Acknowledgments
Funding This study was supported by a grant from the AUGS/SGS Group of the Fellows’ Pelvic Research Network. The funding source had no role in the conduct of the research, data collection, analysis, interpretation of data, writing of the manuscript, or decision to submit the manuscript for publication. Statistical analysis of research reported in this publication was partially supported by National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR003096.
Footnotes
Conflicts of interest This study was supported by a grant from the AUGS/SGS Group of the Fellows’ Pelvic Research Network.
The authors report no conflict of interest.
Conference presentations Presented at the 45th Annual Scientific Meeting of the Society of Gynecologic Surgeons, Tucson, AZ,March 31-April 3, 2019
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s00192-019-04189-0) contains supplementary material, which is available to authorized users.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rayburn WF, Liu CQ, Elwell EC, Rogers RG. Diversity of physician faculty in obstetrics and gynecology. J Reprod Med. 2016;61(1–2):22–6. [PubMed] [Google Scholar]
- 2.Neubardt SB, moderator. Women’s liberation and the male gynecologist [roundtable]. Med Aspect Hum Sex 1974;8:158–199. [Google Scholar]
- 3.Jolliff L, Leadley J, Coakley E, Sloane RA. Women in US academic medicine and science: statistics and benchmarking report 2011–2012. Washington, DC: Association of American Medical Colleges; 2012. [Google Scholar]
- 4.Haar E, Halitsky V, Stricker G. Factors related to the preference for a female gynecologist. Med Care. 1975;13:782–90. [DOI] [PubMed] [Google Scholar]
- 5.Johnson AM, Schnatz PF, Kelsey AM, Ohannessian CM. Do women prefer care from female or male obstetrician–gynecologists? A study of patient gender preference. J Am Osteopath Assoc. 2005;105:369–79. [PubMed] [Google Scholar]
- 6.Plunkett BA, Kohli P, Milad MP. The importance of physician gender in the selection of an obstetrician or a gynecologist. Am J Obstet Gynecol. 2002;186(5):926–8. [DOI] [PubMed] [Google Scholar]
- 7.Janssen SM, Lagro-Janssen AL. Physician’s gender, communication style, patient preferences and patient satisfaction in gynecology and obstetrics: a systematic review. Patient Educ Couns. 2012;89(2):221–6. 10.1016/j.pec.2012.06.034. [DOI] [PubMed] [Google Scholar]
- 8.Huis Int’Veld EA, Canales FL, Furnas HJ. The impact of a plastic surgeon’s gender on patient choice. Aesthet Surg J. 2017. April 1;37(4):466–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dusch MN, O’Sullivan PS, Ascher NL. Patient perceptions of female surgeons: how surgeon demeanor and type of surgery affect patient preference. J Surg Res. 2014. March;187(1):59–64. [DOI] [PubMed] [Google Scholar]
- 10.Abghari MS, Takemoto R, Sadiq A, Karia R, Phillips D, Egol KA. Patient perceptions and preferences when choosing an orthopaedic surgeon. Iowa Orthop J. 2014;34:204–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Brueseke T, Muffly T, Rayburn W, Connolly A, Nieto M, De La Cruz J, et al. Workforce analysis of female pelvic medicine and reconstructive surgery, 2015 to 2045. Female Pelvic Med Reconst Surg. 2016;22:385–9. [DOI] [PubMed] [Google Scholar]
- 12.York NL, DaRosa DA, Markwell SJ, Niehaus AH, Folse R. Patients’ attitudes toward the involvement of medical students in their care. Am J Surg. 1995;169(4):421–3. [DOI] [PubMed] [Google Scholar]
- 13.O’Malley PG, Omori DM, Laudry FJ, Jackson J, Kroenke K. A prospective study to assess the effect of ambulatory teaching on patient satisfaction. Acad Med. 1997;72(11):1015–7. [DOI] [PubMed] [Google Scholar]
- 14.Malcolm CE, Wong KK, Elwood-Martin R. Patients’ perceptions and experiences of family medicine residents in the office. Can Fam Physician. 2008;54(4):570–1. [PMC free article] [PubMed] [Google Scholar]
- 15.Jiang X, Altomare C, Egan JF, Tocco DB, Schnatz PF. The ObGyn clerkship: are students denied the opportunity to provide patient care and what is the role of gender? Conn Med. 2012;76(4):231–6. [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.(2011) TF–IDF. In: Sammut C, Webb GI (eds) Encyclopedia of Machine Learning. Springer, Boston, MA. [Google Scholar]
- 18.Joachims T. A probabilistic analysis of the Rocchio algorithm with TFIDF for text categorization: DTIC document, 1996. [Google Scholar]
- 19.Fellows I. wordcloud: Word Clouds, 2018. R package version 2.6. https://CRAN.R-project.org/package=wordcloud.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.