Abstract
Traumatic brain injury (TBI) is a leading cause of death and disability in young adults worldwide. TBI survival is associated with persistent neuropsychiatric and neurological impairments, including posttraumatic epilepsy (PTE). To date, no pharmaceutical treatment has been found to prevent PTE or ameliorate neurological/neuropsychiatric deficits after TBI. Brain trauma results in immediate mechanical damage to brain cells and blood vessels that may never be fully restored given the limited regenerative capacity of brain tissue. This primary insult unleashes cascades of events, prominently including neuroinflammation and massive oxidative stress that evolve over time, expanding the brain injury, but also clearing cellular debris and establishing homeostasis in the region of damage. Accumulating evidence suggests that oxidative stress and neuroinflammatory sequelae of TBI contribute to posttraumatic epileptogenesis. This review will focus on possible roles of reactive oxygen species (ROS), their interactions with neuroinflammation in posttraumatic epileptogenesis, and emerging therapeutic strategies after TBI. We propose that inhibitors of the professional ROS-generating enzymes, the NADPH oxygenases and myeloperoxidase alone, or combined with selective inhibition of cyclooxygenase mediated signaling may have promise for the treatment or prevention of PTE and other sequelae of TBI.
Keywords: Posttraumatic epilepsy, Oxidative-stress, Neuroinflammation, Redox-signaling, NADPH oxidase, Myeloperoxidase and Traumatic Brain Injury
1. Introduction
Traumatic brain injury (TBI) is a major cause of death and disability among young adults in the United States. Each year an estimated 1.7 million Americans sustain a TBI: 52,000 die, 275,000 are hospitalized and survive (Leo and McCrea, 2016), and about 124,000 develop long-term disability (Selassie et al., 2008). Depending upon the type, severity and location of the injury and the age, general health and genetic constitution of the individual, TBI may result in wide range of disabilities with potentially devastating impact on quality of life. These may include sensory, motor and cognitive impairments, affective disturbances (Stocchetti & Zanier, 2016), as well as posttraumatic epilepsy (PTE), which will be the focus of this review.
PTE is defined as recurring spontaneous seizures occurring more than 7 days after injury. PTE complicates 3–5% of moderate TBI and as many as 50% of severe TBI. TBI is the leading cause of epilepsy with onset in young adulthood (Annegers, 1996; Annegers et al., 1998). While the specific mechanisms of human posttraumatic epileptogenesis are not known, the formation of a posttraumatic epileptic focus must involve some subset of the pathophysiological cascades unleashed by brain trauma.
There is presently no means to prevent or cure any of the functional impairments induced by TBI, including PTE. Pharmacological treatment for PTE and other epilepsies is symptomatic – drugs must be taken regularly to suppress seizures. Over 2 dozen drugs are now available for treatment of epilepsy, but the proportion of patients with adequate seizure control did not grow appreciably as new drugs were introduced, and about 1/3 of epilepsy patients suffer seizures that cannot be controlled with antiseizure drugs (Loscher and Schmidt, 2011).
Because the physiological basis of the propensity to spontaneously generate paroxysms of abnormal hypersynchronous neuronal activity (seizures) in clinical epilepsy is unknown, current antiseizure drugs have been developed to suppress seizures by altering the balance of neural excitation and inhibition (White et al., 2007; Loscher et al., 2013). Epilepsy drug development has largely been guided using evoked seizure models (Loscher and Schmidt, 2011; Loscher et al., 2013), and the discovered drugs overwhelmingly target neuronal and synaptic mechanisms (Kaminsky et al., 2014). While the sheer number of drugs available for the treatment of epilepsy attests to the success of this drug development strategy, the lack of disease-preventing or disease-modifying drugs and the sizable proportion of unresponsive patients suggests that clinically important pathogenic mechanisms may have been overlooked.
While many factors may have contributed to the failure of clinical trials to identify effective treatments, growing attention to the complexity of TBI and new insights into the mechanisms mediating epileptogenesis after brain injury point to new strategies and avenues of intervention. In particular, two recent advances provide a likely path to the development of novel drugs to control currently refractory seizures and to prevent the development of epilepsy after epileptogenic brain insults (e.g. Infection, stroke and trauma). First, a body of research that has grown exponentially since the 1990s has elaborated a wide variety of non-neuronal and non-synaptic mechanisms that may contribute to epileptogenesis. These include astroglial (Aronica et al., 2012; Robel, 2017) and microglial (Eyo et al., 2017; Hiragi et al. 2018) mechanisms, blood-brain barrier disruption (Heinemann et al., 2012; van Vliet et al., 2015), inflammation (Vezzani and Granata, 2005; Vezzani et al., 2013; de Vries et al., 2016), generation of reactive oxygen species (ROS) and oxidative stress (Shin et al., 2011; Pearson-Smith and Patel, 2017. The second advance is the development of etiologically realistic syndrome specific models of acquired epilepsies that feature the development of chronic spontaneous recurrent seizures (Kelly et al., 2001; D’Ambrosio et al., 2004; 2005; Dube et al., 2006; Stewart et al. 2010; Rakhade et al., 2011; Reid et al., 2016; Ping and Jin, 2016), and are highly likely to incorporate epileptogenic mechanisms that operate in the corresponding human epilepsies (Curia et al., 2016). Together, these advances should pave the way for discovery of novel treatments to address the needs of patients whose seizures are inadequately controlled by available anti-seizure drugs and to prevent epilepsy after brain injury. This review will focus on the roles of ROS, professional ROS-generating enzymes and neuroinflammation, and on strategies targeting them, either alone or in combination with cyclooxygenase-related inflammatory mechanisms, to treat or prevent epilepsy.
2. Reactive Oxygen Species, Redox Signaling & Oxidative Stress
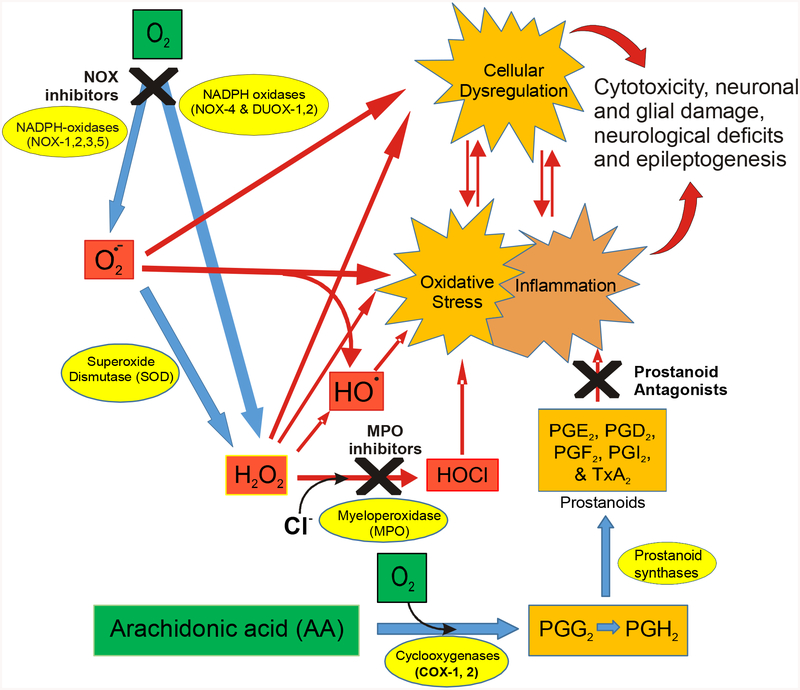
ROS – superoxide (O2●−), hydrogen peroxide (H2O2) and the hydroxyl radical (●OH) – are the reactive products of sequential 1-electron reduction of molecular oxygen. They are generated by mitochondria, and by other cellular enzymes often as side products of oxidative metabolism. ROS, particularly the highly reactive radical species, O2●− and ●OH, can oxidize lipids, nucleic acids and proteins to damage membranes and DNA, and inactivate enzymes, receptors and ion channels (Pisoschi and Pop, 2015). They can also react spontaneously or via enzyme catalyzed reactions to generate further damaging species. In the presence of iron, superoxide and H2O2 are converted to the much more reactive ●OH. Moreover, superoxide will react with nitric oxide to generate peroxynitrite (ONOO-). Myeloperoxidase (MPO) produces hypochlorous acid (HOCl−) and inducible nitric oxide synthase (iNOS) produces nitric oxide (NO●). Cyclooxygenases (COX-1 and COX-2) produce prostaglandin intermediates from arachidonic acid, via peroxidase activity first to PGG2 then to PGH2. A family of NADPH oxidase (NOX) enzymes catalyze the production of O2●− and H2O2 from molecular oxygen. These are the key players in the cellular generation of ROS and induction of neuroinflammation (Fig 1).
Figure 1:
TBI results in inflammation and increased ROS generation, which are closely linked and self-reinforcing. Pathological ROS production can both alter the activities of redox regulated enzymes and pathways and directly induce cytotoxic oxidative stress, initiating or exacerbating inflammation. Both ROS and inflammatory mediators can alter and impair the function of neurons, glia and other brain cells, resulting in increased production of inflammatory mediators and increased neuronal excitability. The figure illustrates how inhibitors of ROS-generating enzymes and of proinflammatory prostanoid receptors can be deployed either together or separately to alter the vicious cycles of inflammation, oxidative stress and cellular dysregulation that drive secondary injury after TBI.
When the cells are in homeostasis, there is a balance between ROS generation by mitochondria and ROS producing pro-oxidant enzymes (e.g. NOX, iNOS, MPO and COX) and ROS scavenging by antioxidant enzymes (e.g. catalase, superoxide dismutase and glutathione reductase), and endogenous antioxidant molecules such as glutathione, ascorbic acid and tocopherols (Valko et al., 2007; Circu and Aw, 2010). Outside of the microbicidal oxidative burst of phagocytic cells, ROS have conventionally been regarded as unavoidable toxic byproducts of oxidative metabolism that are kept in check by cellular antioxidant defenses. However, in homeostatic conditions, ROS also participate in redox signaling (Jiang et al., 2011; Lambeth and Neish, 2014, Scheiber and Chandel, 2014). Contained, localized generation of ROS, particularly H2O2, can reversibly oxidize vulnerable protein cysteine residues to modulate the activities of a wide range of enzymes, ion channels and transporters (Valko et al., 2007; Jiang et al., 2011). Oxidative stress arises when the balance between ROS levels and antioxidant environment is upset, leading to deleterious effects (Hole et al., 2011). Excess ROS can cause irreversible oxidative damage to cells, proteins, lipids, and DNA leading to cellular necrosis or apoptosis and consequent cellular or tissue injury (Chaudhari et al., 2014; Lambeth and Neish, 2014). Moreover, superoxide can inactivate antioxidant enzymes. Therefore, oxidative stress is implicated in a variety of acute and chronic diseases (Keyer et al., 1995; Maraldi, 2013). Two possible therapeutic approaches can be utilized to reduce the ROS in the body: i) scavenge ROS by administering antioxidants or enhancing the activities of endogenous antioxidant enzymes, ii) prevent or diminish ROS generation by inhibiting the various pro-oxidant enzymes.
3. NADPH-Oxidases
NOXs and dual oxidases (DUOXs) comprise a family of seven enzymes that together constitute the primary source of regulated physiological ROS production (Sirokmany et al., 2016). Each produces ROS as the principal product of its catalytic activity. NOX1, NOX2, NOX3 and NOX5 generate superoxide while NOX4, DUOX1 and DUOX2, predominantly produce hydrogen peroxide (Bedard and Krause, 2007; Nisimoto et al., 2014; Ma et al., 2017). These ROS-producing enzymes are differentially expressed in a variety of tissues and cell types throughout the body, where they play key roles in redox signaling (Lambeth and Neish, 2014; Scheiber and Chandel, 2014; Nordzeike and Medrano-Fernandez, 2018) and other specialized functions. For instance, the well-studied prototypic NOX, NOX2, was first found in phagocytic cells (neutrophils and macrophages), where it is highly enriched. It fuels the cytotoxic respiratory burst in these cells and has long been recognized for its role in innate immunity (Rada, 2008) and inflammatory diseases (Segal, 1996; Biemond et al., 1986; Weiss and Reddy, 1989).
While all NOX isoforms have been detected (mRNA or protein) in brain tissue, the regional distribution of NOX isoforms in the brain has not yet been extensively mapped. NOX2 and NOX4 appear to be the main isoforms expressed in the brain under physiological conditions, and NOX2 is quantitatively the most important (Sorce et al., 2017; Sorce and Krause, 2009). Both have been demonstrated in tissue samples from a variety of brain regions including neocortex, hippocampus and cerebellum (Sorce and Krause, 2009; Ma et al., 2017). NOX2 is predominantly expressed in microglia, consistent with these cells’ role as the principal resident immune cells in the brain with the potential for phagocytic activity. NOX1, NOX2 and NOX4 expression has been reported in primary cultures of neurons, astrocytes and microglia from various species. NOX enzymes are inducible and upregulation of 1 or more NOX isoforms, almost invariably including NOX2, has been reported after experimental brain insults and in brain tissue from patients suffering from brain injuries and from a variety of neurological/neurodegenerative disorders (Ma et al., 2017). NOX expression has been reported to be elevated in human brain after TBI, and in patients suffering from Alzheimer’s disease, amyotrophic lateral sclerosis and multiple sclerosis (Ma et al., 2017;2018). Experimental brain insults that result in increased NOX expression include controlled cortical impact (mechanical brain injury), ischemia/re-perfusion, and status epilepticus induced by electrical stimulation, the muscarinic agonist, pilocarpine and the excitotoxin, kainic acid (Patel et al., 2005; Pestana et al., 2010; Zhang et al., 2012; Cooney et al., 2013;Williams et al., 2015).
Thus, excessive induction and activity of NOX isoforms is associated with brain tissue injury and dysfunction in a variety of pathological conditions and experimental brain insults (Lambeth, 2007; Sorce and Krause, 2009). Conversely, NOX inhibition or genetic deletion of specific NOX isoforms is often reported to improve outcomes after experimental insults that typically induce elevated NOX expression. For example, pharmacological inhibition of NOX activity significantly diminished neurodegeneration after electrically or pilocarpine-induced status epilepticus in rats (Pestana et al., 2010; Williams et al., 2015). Genetic deletion of NOX2 and NOX4 have both been reported to reduce infarct volume in rodent stroke models (Chen et al. 2011, Klienschnitz et al., 2010). In rodent TBI models, inhibition of NOX2 has been reported to attenuate injury-induced increases of markers of astroglial and microglial activation, decrease neuronal loss in neocortex and hippocampus, and improve functional recovery (Zhang et al., 2012; Feng et al., 2017). In NOX2 knockout mice, microglial activation was attenuated and neurogenesis enhanced after TBI compared to wild type (Dohi et al., 2010; Wang et al., 2018b).
NOXs are increasingly recognized as major sources ROS contributing to the pathophysiology of a wide range of clinical conditions and attractive targets for the development of new drugs (Bedard and Krause, 2007; Kahles and Brandes, 2013; Lambeth and Neish, 2014; Diebold et al., 2015; Sorce et al., 2017). NOX-generated ROS may contribute to pathology in two ways. First, elevated ROS production may lead to pathological dysregulation of redox-regulated processes. Also, excessive ROS generation may lead to oxidative damage to cells and tissues. Superoxide is the product of the most abundant NOX in brain and it the most common free radical generated following traumatic brain injury (Kontos and Povlishock, 1986; Kontos and Wei, 1986). Under the acidic conditions characteristic of TBI, superoxide converts to hydroperoxyl radical (HO2●), a more lipid soluble and powerful oxidant than the superoxide itself. This results in greater lipid peroxidation and additional brain tissue damage and mitochondrial disfunction (Mustafa et al., 2010; Singh et al., 2013). It has also been shown that peroxynitrite (ONOO-) exacerbates pathophysiology post TBI, demonstrated by treatment with iNOS inhibitor or peroxynitrite scavenger, which resulted in beneficial effects in TBI injured mice and rats (Deng-Bryant et al., 2008; Mesenge et al., 1998; Wada et al., 1998). These data indicate a mainly deleterious role of ROS in TBI and support the idea that inhibition of NOX activity after TBI will have therapeutic benefit.
4. Myeloperoxidase (MPO)
Myeloperoxidase is actively synthesized by promyelocytes and promyelomonocytes in bone marrow during the differentiation. MPO accounts for up to 2–5% of the cellular protein in neutrophils (Bos et al., 1978). Phagosomes of neutrophils discharge the cocktail of antimicrobial systems to destroy the microorganisms in the body (Klebanoff, 2005). The cocktail includes MPO, hydrogen peroxide and halide (mainly chloride) ion (Hampton et al., 1998). The potent and primary antimicrobial oxidant produced by MPO is hypochlorous acid (HOCl or OCl−) (Fig 1), other reactive agents and radicals synthesized by MPO are OSCN−, NO2● and Thr●. While the HOCl acts as microbial killing and is useful for protection against invading microorganisms, in pathological conditions, all these reactive species and radicals will react with lipids, proteins, and DNA and other biomolecules leading to various pathologies, including cardiac dysfunction, atherosclerosis, diabetes; and CNS diseases such as ischemia/reperfusion and Parkinson’s disease (Malle et al., 2006; Malle et al., 1997). It is yet to be determined whether myeloperoxidase will play a direct role in TBI pathophysiology, however, when the blood brain barrier (BBB) is compromised during severe and penetrating traumatic brain injuries, neutrophils are infiltrated into the brain. It has been shown that infiltrated neutrophils are involved in inflammation and neurodegeneration, via exacerbating oxidative-stress environment and working with other innate immunity cells (Ryu et al., 2007).
5. Cyclooxygenase-1 and Cycloxygenase-2
Both COX-1 and COX-2 catalyze the conversion of arachidonic acid to prostaglandin-G2 and then to prostaglandin-H2, which will be converted to a five different prostanoids, prostaglandin-E2 (PGE2), prostaglandin-D2 (PGD2) prostaglandin-F2 (PGF2), prostacyclin (PGI2) and thromboxane (TXA2) by cell specific synthase enzymes depending on the need of environment (Fig 1). These prostanoid ligands will activate eleven receptors (including splice variants). PGE2 activates EP1, EP2, EP3 and EP4; PGD2 activates DP1 and DP2; PGF2 activates FPα and FPβ; PGI2 activates IP and TXA2 activates TPα and TPβ receptors. Functionally, EP2, EP4, DP1 and IP receptors mediate smooth muscle relaxation via intracellular cAMP signaling, whereas EP1, FP and TP mediate smooth muscle contraction by intracellular calcium signaling, and DP2 and EP3 inhibit the cAMP signaling (Rojas et al., 2019). Although some of these receptors share a common endogenous ligand for activation (e.g. EP1-EP4 share PGE2; DP1 and DP2 share PGD2), their downstream signaling mechanisms differ, suggesting the value of prostaglandins in various physiological and pathological functions. So far studies point to a proinflammatory role for EP2, EP4 and DP1, whereas the IP receptor acts as a cardioprotective receptor whose function must not be disrupted with any therapeutic agents (Egan et al., 2004). In view of the COX-2 inhibitor drug, Vioxx, experience (Grosser et al., 2010), future anti-inflammatory agents should target selectively the proinflammatory receptors, such as the EP2 receptor (Ganesh, 2014), rather than blocking the entire COX-2 cascade, to bypass the adverse effects on humans.
TBI in humans induced a sustained inflammation, including the activation of microglia and ongoing white matter degeneration for many years after single TBI (Johnson et al., 2013). Mice with TBI induced by a single episode of controlled cortical impact also exhibited persistent microglial activation in the injured cortex throughout 1 year after injury, and it was associated with progressive lesion expansion, hippocampal neurodegeneration, and loss of myelin (Loane et al., 2014). The prevailing hypothesis is that the cytokines, chemokines and COX-2, rapidly released by astrocytes and dying neurons, will trigger the inflammatory environment in the brain, leading to microglial activation. Once activated, the microglia further induce additional cytokines and chemokines, COX-2 and ROS. Animal models of TBI also present this neuroinflammatory environment (Bergold, 2016; Chiu et al., 2016; Simon et al., 2017). For example, Strauss et al. (2000), showed that COX-2 (mRNA and protein) peaks from around 6 h until 3 days post injury and returns to sham levels by 7 days in the ipsilateral cerebral cortex and in the ipsilateral and contralateral hippocampus in the cortical contusion and lateral fluid percussion injury models of TBI. Shojo et al. (2017), reported time-dependent increases in COX-1 and COX-2 in the cortex starting at 3h in a TBI model of lateral fluid percussion injury; and, COX-1 was specifically induced in degenerating neurons, whereas COX-2 was expressed in macrophages. Kunz et al. (2002), found that COX-2 mRNA was upregulated in cortex and dentate gyrus regions starting at 3h until 72 h in a another fluid percussion injury rat model of TBI.
The above data suggest that COX-2 will be a therapeutic target, and preclinical data underscore that the COX-2 inhibitors will have beneficial functional outcome in various models of TBI. Although it is not clear why the COX-2 selective drugs were not tested in clinical trials, it may be due to the fatal adverse cardiotoxic effects found with chronic use of COX-2 drugs in patients with other diseases (Egan et al., 2004; Funk and FitzGerald, 2007; Grosser et al., 2010).
A key question is how to intervene in the cross talk among the players of neuroinflammation (cytokines, chemokines, COX-2, gliosis) and oxidative burst and oxidative stress enzymes (NOX and INOS). It has been shown that conditional deletion of COX-2 in neurons blunted 34 out of 38 inflammatory cytokines and chemokines and gliosis in a status epilepticus brain injury model (Serrano et al., 2011). Moreover, it has been shown that a specific prostanoid receptor EP2 activation and inhibition will have an effect on expression levels of inflammatory mediators, ROS producing enzymes in vitro microglia cultures suggesting a cross-talk between prostanoid signaling and inflammatory mediators (Quan et al., 2013).
6. ROS, Inflammation and the Pathophysiology of TBI
Mechanical trauma to the brain produces a limited primary injury (e.g. disruption of cell membranes, blood vessels and blood-brain barrier, resulting in the immediate demise of neurons, glia and epithelial cells), and unleashes secondary injury processes that progress over time, expanding the volume of injured tissue to account for much of the injury-induced disability. Only the secondary injury, which is mediated by processes unleashed by the primary injury and may progress for weeks, months or even years before homeostasis is reestablished, can be effectively targeted by therapeutic measures.
TBI is a complex injury to a complex organ, and its pathophysiology has been the subject of many excellent reviews (Ray et al., 2002; Werner and Engelhard, 2007; Borgens and Liu-Snyder, 2012; Prins et al., 2013; Quillinan et al., 2016; Morganti-Kossmann et al., 2019). Here, some important pathophysiological pathways will be outlined, emphasizing those that are likely contributors to posttraumatic epileptogenesis. Membrane disruption induced by the mechanical injury results in widespread neuronal depolarization and massive release of glutamate, extravasation of blood components through a disrupted blood-brain barrier (BBB) into the brain parenchyma and release of damage associated molecular patterns (DAMPs; e.g. ATP, RNA, high-mobility group box-1) from damaged cells (Hirsiger et al., 2012). Glutamate release induces further depolarization of still-viable neurons, Ca++ influx, mitochondrial damage and associated energy deficits, increased generation of toxic ROS by damaged mitochondria, and neuronal excitotoxicity. ROS deplete cellular antioxidants, react with nucleotides and proteins and initiate peroxidation of cellular membranes, further damaging cells and organelles. DAMPs released from dead and damaged cells initiate cytokine signaling cascades that orchestrate the inflammatory response that results in the destruction and clearance of damaged cells and the eventual establishment of a new tissue homeostasis. The cellular inflammatory response involves further ROS generation due to the respiratory bursts of neutrophils, macrophages and activated microglia attracted to the site of injury. Thus the physiological processes required to reestablish homeostasis in the damaged brain also contribute to the widening of the injury and a progressive loss of function, and inflammation and ROS generation are thought to be the most important secondary injury processes operating after the acute period after injury.
Although we lack a detailed understanding of its role in the pathogenesis of TBI, inflammation is well accepted as an important pathway of secondary injury and inflammatory mechanisms and inflammation-related therapeutic targets have been recently reviewed (Ruppel et al., 2002; Cornelius et al., 2013 Rodriguez-Rodrigues et al., 2014; Hall et al., 2015; Toklu et al., 2015; Frati et al., 2017). Elevated expression of key pro-inflammmatory cytokines is consistently observed in human and animal brain tissue following TBI (Ott et al., 1994; Holmin and Hojeberg, 2004; Ziebell and Morganti-Kossmann, 2010; Helmy et al., 2011). In experimental models, injury-related endpoints are often improved by pharmacological inhibition of pro-inflammatory cytokine synthesis, knock-out or knock-down of pro-inflammatory cytokine expression or by inhibition of receptor binding (Fogal and Hewett, 2008). Conversely, overexpression or application of exogenous pro-inflammatory cytokines is frequently reported to exacerbate brain injury (Toulmond and Rothwell, 1995; Lloyd et al., 2008; Ziebell and Morganti-Kossmann, 2010; Helmy et al., 2011; Gyoneva and Ransohoff, 2015). While research in this area has been extensive, the roles of TNF-α, IL-1β and IL-6, and associated signaling pathways (particularly NFkB) have been particularly well studied, and the roles of high mobility group box 1 (HMGB1) and Toll-like receptor-4 (Laird et al., 2014; Parker et al., 2017; Paudel et al., 2018) in secondary injury have commanded considerable attention, recently.
ROS also have long been postulated to contribute importantly to the secondary injury following brain trauma. Trauma-induced hypoxia/ischemia and calcium fluxes both promote ROS generation from mitochondria, and mitochondrial ROS generation is stimulated by ROS (Zorov et al., 2014). While most ROS are short-lived and difficult to demonstrate directly, the products of their reactions with lipids, proteins and nucleic acids, are consistently elevated after experimental TBI (Inci et al., 1998; Tyurin et al., 2000; Mendez et al., 2004; Ansari et al., 2008) and in blood and postmortem tissue from TBI victims (Cristofori et al., 2001; Varma et al., 2003; Yen et al., 2015; Schiavone et al., 2017). In experimental TBI models, a wide range of antioxidant treatments have been reported to reduce injury-induced neurodegeneration and improve functional recovery (Slemmer et al., 2008). While early studies focused on treatments with small-molecule and catalytic antioxidants that metabolize or scavenge ROS, many recent investigations have focused on ROS generated by NOX. NOX expression is increased after experimental TBI (Dohi et al., 2010; Cooney et al., 2013) and in surgical specimens from contused human brain (Li et al., 2015). Many studies have shown that knockdown, knock-out or inhibition of NOX2 can reduce oxidative stress markers, cortical lesion volume, BBB disruption, neurodegeneration, and a range of neurological deficits in several different TBI models (Choi et al., 2012; Ferreira et al, 2013; Loane et al., 2013; Luo et al., 2013; Song et al., 2013; Lu et al., 2014). Thus NOX-derived ROS play a significant role in the secondary expansion of injury after brain trauma.
7. ROS and Inflammation in Epilepsy and Epileptogenesis
Over the past 25 years, a burgeoning literature has demonstrated neuroinflammation and ROS generation to have deleterious roles in epilepsy and epileptogenesis (Vezzani and Granata, 2005; Choi and Koh, 2008; Waldbaum and Patel, 2010; Aronica and Crino, 2011; Vezzani et al., 2011; Cardenas-Rodriguez et al., 2013; Devinsky et al., 2013; Rowley and Patel, 2013; Gorter et al., 2015; Vezzani et al., 2016; de Vries et al., 2016; Aronica et al., 2017; Pearson-Smith and Patel, 2017; Webster et al., 2017; Hiragi et al., 2018; Paudel et al., 2019), suggesting a broad overlap between the pathophysiological cascades unleashed by TBI and the inflammatory and oxidative processes that promote spontaneous seizures. Neuroinflammation, as indicated by glial reaction and increased expression of proinflammatory cytokines and other mediators, is a consistent feature of the epileptic brain regardless of etiology. Seizures induce inflammation and several inflammatory cytokines have been demonstrated exacerbate seizures. IL-1β, TNF-α and IL-6 have all been demonstrated to modulate neuronal excitability either directly or indirectly (Vezzani and Viviani, 2015; Iori et al., 2016). Studies have implicated many cytokines in epilepsy and epileptogenesis
Like inflammation, elevated ROS generation and oxidative stress appear to be consistent features of experimental epileptogenic insults (Liang et al., 2000; Waldbaum and Patel, 2010; Bhuyan et al., 2015) and of post-mortem tissue from TBI victims (Buritica et al., 2009) and surgical specimens from chronic epilepsy patients (Lopez et al., 2007; Rumia et al., 2013). Also similar to inflammation, increased ROS appear to be both a cause and consequence of seizures (Patel, 2004). In fact, inflammation and ROS generation appear to be inextricably linked. Inflammatory pathways modulate ROS generation and ROS, in turn, modulate inflammatory pathways (van der Vliet et al., 2014; Harijith et al., 2014; Singel and Segal, 2016; Forrester et al., 2018). Deleterious levels of ROS could be generated in critical compartments by a variety of sources including mitochondria, NOX enzymes and other enzymes that generate ROS as side-products, and contributing sources may change over time after an epileptogenic insult (Kovac et al., 2017). Historically, mitochondria have been considered to be the most important source of ROS both constitutively and in pathological conditions, and ROS regarded as intrinsically destructive. However, following the discoveries of enzymes, receptors, transport proteins and ion channels that are reversibly modulated by ROS (Valko et al., 2007; Lambeth and Neish, 2014; Scheiber and Chandel, 2014; Nordzieke and Medrano, 2018)), and the NOX family of enzymes whose sole activity is to generate ROS at the expense of biological reducing equivalents (Bedard and Krause, 2007; Nayernia et al., 2014), it is now apparent that ROS can modulate a wide range of physiological processes, and that NOX enzymes are an important source of ROS in many pathological conditions.
Cytotoxicity is the best known effect of ROS generation. While the necessity of neurodegeneration for acquired epileptogenesis has not been firmly established, most epileptogenic insults are associated with significant loss of neurons, and abnormal network activity is a plausible consequence of widespread loss of neurons. Thus, neuroprotection is widely expected to oppose epileptogenesis. The particular vulnerability of neurons to ROS is well-known (Cobley et al., 2018), and antioxidant treatments (MacGregor et al., 1996; Marklund et al., 2001; Deng-Bryant et al., 2008; dos Santos et al., 2011; Zhang et al., 2012; Ambrogini et al., 2014; Pandya et al., 2014) and treatments that reduce NOX activity (Dohi et al., 2010; Ferriera et al., 2013; Pestana et al., 2010; Choi et al., 2012; Kim et al., 2013) are almost invariably reported to be neuroprotective after experimental TBI and other experimental insults that can result in epilepsy, including electrically or chemoconvulsant-induced status epilepticus. Pretreatment of animals with antioxidants has been reported to reduce or retard seizure activity after administration of convulsants such as kainate, pentylenetetrazole and pilocarpine (Devi et al., 2008; Shin et al., 2011). Such anticonvulsant effects are accompanied by decreases in indicators of oxidative stress, but it is not clear that protection from oxidative damage to cells is responsible. For instance, among the strongest anticonvulsant effects reported was that induced by α-lipoic acid pretreatment on pilocarpine induced seizures (de Freitas, 2010): the latency to first seizure was more than three times longer in α-lipoic acid-treated rats and only 25% of α-lipoic acid-treated rats developed seizures as compared to 100% of rats treated with pilocarpine alone. Pilocarpine is well known to induce ROS generation resulting in oxidative stress, and de Freitas (2010) measured a 50% depletion of reduced glutathione in brains of pilocarpine-treated animals that was reversed by the α-lipoic acid treatment, which also increased glutathione peroxidase activity. While oxidative stress was doubtless reduced by α-lipoic acid treatment, the treatment also reduced the activity of the sodium-potassium pump, which would likely promote neuronal hyperexcitability.
Although the neuroprotective effects of a variety of antioxidant treatments following TBI and electrically and chemoconvulsant-induced status epilepticus (SE), protocols that form the basis of most chronic epilepsy models, have been demonstrated, the effects of antioxidants on the development of spontaneous seizures have rarely been assessed in chronic epilepsy models. One group found melatonin treatment to decrease the frequency of spontaneous seizures in the chronic phase after kainate-induced SE in spontaneously hypertensive rats (Petkova et al., 2014) but not rats of the Wistar strain (Tchekalarova et al., 2013), and resveratrol, a natural compound with antioxidant and anti-inflammatory properties was found to decrease the incidence of spontaneous seizures in a kainate model (Wu et al., 2009). In contrast, a catalytic antioxidant failed to affect spontaneous seizures in the pilocarpine model (Pearson et al., 2015). More recently, Pauletti et al. (2017) showed that a transient treatment that increased brain glutathione levels markedly decreased the frequency of the spontaneous seizures that developed after electrically induced SE. These investigators also showed that treatment maintained HMGB1, a DAMP that is thought to promote epileptogenesis (Ravizza et al., 2018; Paudel et al., 2018; 2019).
In principle, ROS could contribute to epileptogenesis by exacerbating neuroinflammation, by disrupting the activities of redox-regulated cellular processes, or via their cytotoxic effects on neurons and other brain cells. Toxic or disruptive levels of ROS could be generated by a variety of sources including mitochondria, NOX enzymes and other enzymes that generate ROS as side-products, and contributing sources may change over time after an epileptogenic insult (Kovac et al., 2017).
8. NOX, Redox Regulation and Posttraumatic Epileptogenesis
While the details remain poorly delineated, roles for inflammation in ictogenesis and epileptogenesis are now well established, and the interaction of ROS with inflammation provide multiple avenues for ROS modulation of epileptogenesis. For example, signaling through interleukin-1 β (IL-1β), tumor necrosis factor-α (TNF-α) and HMGB1 – all under active investigation for their contributions to epilepsy and epileptogenesis (van Vliet et al., 2018; Webster et al., 2017; Ravizza et al., 2018; Paudel et al., 2018; 2019) – is subject to redox modulation. HMGB1 is a DAMP with chemokine-like and cytokine-like activities that depend on the redox state of 2 cysteine residues. HMGB1 exhibits leukocyte chemoattractant properties when these are in their reduced states, and promotes proinflammatory cytokine (including IL-1β and TNF-α) secretion when these cysteine residues are oxidized (Venereau et al., 2012; Yang et al., 2013; Paudel et al., 2019). ROS also promote activation of nuclear factor-)κB (NFκB; Kaur et al., 2015), a transcription factor required for maximal transcription of many pro-inflammatory mediators, including TNF-α and IL-1β (Christman et al., 2000), both of which signal, in part, via NFkB activation (Allan et al., 2005; Schutze et al., 1995). As a result, ROS can influence both the magnitude of expression of these important inflammatory mediators and downstream effects of IL-1β and TNF-α receptor ligation, and NOX-derived ROS are frequently implicated. For example, NOX inhibition has been found to attenuate TNF-α-evoked BBB dysfunction (Abdullah and Bayraktutan, 2014) and IL-1-induced astrocyte migration (Yang et al., 2015). NOX activity is also a potent modulator of the cellular component of inflammation. NOX activity generates the cytotoxic respiratory burst of activated microglia and macrophages (Haslund-Vinding et al., 2017), and NOX derived ROS promote both microglial proliferation (Mander et al., 2006) and their pro-inflammatory M1-like polarization (Kumar et al., 2016; Wang et al 2017). Thus, ROS generated by NOX and other sources potently modulate a number of the postulated inflammatory substrates of epilepsy and epileptogenesis.
Redox regulation is not restricted to inflammatory pathways, and quite a number of proteins with epilepsy-relevant functions are known to be directly or indirectly modulated by ROS. These include various ion channels (Annunziato et al., 2002), transporters (Sorg et al., 1997) and neurotransmitter receptors (Peterson and Weir, 2002). The effects of ROS on N-methyl-D- aspartate (NMDA) receptors and the sodium-potassium pump are of particular interest in the context of epilepsy. NOX is the predominant source NMDA-receptor mediated ROS generation (Brennan et al., 2009) and NOX activation, in tandem with phosphorylation of extracellular signal-related kinases 1 and 2, induce upregulation of NR1 and NR2B subunits and enhanced neuronal excitability after pilocarpine-induced status epilepticus (Di Miao et al., 2011;2013). In addition, a recent study has provided evidence that NMDA receptor induced ROS generation by NOX is required for seizure initiation in several models (Malkov et al., 2019). The sodium-potassium pump, which is critical to the maintenance of cellular membrane potential, is also well-known to be subject to redox modulation (Bogdonova et al., 2016). Accordingly, the activity of the sodium-potassium pump was reported to be diminished after experimental TBI in parallel with increased oxidative stress markers (Lima et al., 2008), and NOX inhibition prevented reductions in sodium-potassium pump activity induced by both TBI (Ferreira et al., 2013) and pilocarpine-induced status epilepticus (de Freitas et al., 2010).
The most compelling evidence implicating NOX-derived ROS in posttraumatic epileptogenesis involves the role of NOX in the death of parvalbumin expressing γ-aminobutyric acid (GABA)ergic inhibitory interneurons (PVINs). In rodents, PVINs account for 40–50% of GABAergic interneurons in the neocortex and up to 30% in the hippocampus (Jiang et al., 2016). These cells make abundant synapses on the somas and proximal dendrites of pyramidal cells and typically emit high frequency spike trains upon depolarization, providing potent inhibition (Jiang et al., 2016). They have thus been of great interest to epilepsy research, and hypofunction of these interneurons due to loss of excitatory drive formed the basis of the “dormant basket cell” hypothesis of acquired temporal lobe epilepsy (Sloviter, 1991). A progressive loss of PVINs in rodents after experimental brain trauma or status epilepticus has been reported by many groups (Toth et al., 1997; Dinocourt et al., 2003; Pavlov et al., 2011; Marx et al. 2013; van der Hel et al., 2014; Wang et al. 2018a), and PVINS appear to be depleted with respect to reference tissue in surgical specimens from epileptic patients and postmortem brain tissue from TBI victims (Leifer et al., 1991; Zhu et al., 1997; Andrioli et al., 2007; Buritica et al., 2009). Recently diverse studies have bolstered the case for a causal link between the loss or disfunction of PVINs and epileptic activity. Drexel and colleagues (2017) used genetic and DREADD (designer receptors exclusively activated by designer drugs) techniques to permanently or transiently silence PVINs in the subiculum of adult mice to demonstrate that prolonged silencing of subicular PVINs results in the development of clustered spike and wave discharges and spontaneous recurrent seizures. Two groups have demonstrated amelioration of pro-epileptic effects of brain injuries by using either focal administration of a partial tropomyosin receptor kinase B (TrkB) agonist (Gu et al., 2018) or a pharmacogenetic approach (Wang et al., 2018b) to activate PVINS after injury. In the cortical undercut model of TBI, treatment with a partial TrkB receptor agonist increased immunoreactivity for parvalbumin and a GABAergic marker, decreased the frequency of spontaneous and evoked epileptoform discharges in vitro and increased the frequency of pyramidal cell miniature inhibitory postsynaptic currents. In vivo, the treatment reduced the incidence of pentylenetetrazole-induced electrographic seizures. Targeted pharmacogenetic activation of PVINs increased the latency to seizure and shortened the duration of the first generalized seizure after kainate administration and, when administered during the chronic phase after kainate-induced status epilepticus, reduced the frequency and duration of spontaneous seizures. A third group used paired pulse transcranial magnetic stimulation to noninvasively monitor GABA-mediated neocortical inhibition after experimental TBI in rats (Hsieh et al. 2017). This demonstrated a progressive loss of paired-pulse inhibition, indicative of a loss GABAergic inhibitory activity over the course of 6 weeks after injury. Immunohistochemical studies revealed a parallel decrease in parvalbumin-positive interneurons and a marker for their associated perineuronal nets in the perilesional neocortex over the same time period. Further, elevated levels of oxidative stress markers in that study implicate ROS in the loss of PVINs.
PVINs are vulnerable to a wide range of stresses besides epileptogenic insults, and in many instances the loss or phenotypic alteration of PVINs has been shown to be mediated by NOX-derived ROS. In rodents IL-6, ketamine exposure, intermittent hypoxia and sepsis all induce loss of PVINs (Behrens et al., 2007; 2008; Ji et al., 2015; Yuan et al. 2015; Liang et al. 2016, Zhang et al., 2016a), and PVIN loss is also observed in models of post-operative cognitive decline, posttraumatic stress disorder and social stress (Schiavone et al., 2009; Liu et al., 2016; Qiu et al., 2016; Sun et al., 2016). In all of these studies, the loss of PVIN phenotype was prevented by treatment with the NOX inhibitor apocyanin. A study comparing postmortem brain tissue from human subjects who died from blunt force TBI and spontaneous intracerebral hemorrhage (Schiavone et al., 2017) found that both oxidative stress markers and NOX2 immunoreactivity were elevated in TBI sections compared to reference specimens and that NOX2 mainly colocalized with immunoreactivity for parvalbumin and GAD67, markers for PVINs. Based on their data these investigators conclude that NOX2 is a crucial and specific molecular agent mediating the trauma-induced loss of PVINs. Thus, there is a substantial body of evidence indicating that NOX-derived ROS mediate the trauma-induced death or dysfunction of a specific subpopulation of neocortical and hippocampal neurons whose loss or impaired function has been linked to the development of spontaneous seizures.
There is also limited evidence pointing to a role for myeloperoxidase in epileptogenesis. Zhang et al. (2016b) demonstrated MPO immunostaining throughout the resected temporal lobe of a refractory epilepsy patient but not in the temporal lobe of a non-epileptic patient, and found increased numbers of MPO-positive cells in the hippocampi of mice during pilocarpine-induced epileptogenesis. Selectively inhibiting MPO delayed the appearance of spontaneous seizures and reduced their frequency. These data are in accord with a previous report that the frequency of spontaneous seizures in the chronic phase after pilocarpine-induced SE was reduced in neutrophil-depleted mice (Fabene et al., 2008). Interestingly MPO has been detected in cells other than neutrophils in several neurodegenerative disorders (Gellhaar et al., 2017), and Zhang et al. (2016b) found that the MPO immunoreactivity detected in mouse hippocampus after pilocarpine treatment colocalized with both neutrophil and microglia/macrophage markers.
9. Conclusions
The main lines of evidence supporting inhibition of NOX-mediated ROS generation for the treatment of posttraumatic epilepsy are summarized in Table 1. The roles of ROS, COX, and inflammation, and their interactions, offer opportunities to develop novel treatments for acute TBI and to prevent or modify posttraumatic epileptogenesis. TBI and posttraumatic epileptogenesis are complex disease processes involving multiple pathways and multi-targeted combination therapies have recently been promoted for both (Loscher et al., 2013; White and Loscher, 2014; Kline et al., 2016; Somayaji et al., 2018). NOX and COX inhibitors are likely to affect both inflammation and epileptogenesis after head injury, and, together may act synergistically to improve outcomes after head injury. Because the pathophysiology of head injury evolves over time, and drug targets may be exposed and disappear as secondary injury and repair progress (Somayaji et al., 2018; Mohamadpour et al., 2019), it cannot be assumed that the highest tolerated doses administered as early as possible and for as long as possible will be most effective. NOX and COX inhibitors and their therapeutic time windows should be systematically investigated with etiologically realistic models of PTE and head injury.
Table 1.
Lines of evidence supporting the development of NOX inhibitors to prevent or modify PTE.
| Summary of evidence indicating potential benefit of NOX inhibition for PTE | References |
|---|---|
| NOX expression and oxidative stress are both increased after experimental TBI. | Inci et al., 1998; Tyurin et al., 2000; Mendez et al., 2004; Ansari et al., 2008 |
| Elevated NOX expression and oxidative stress are observed in surgical specimens and post-mortem brain tissue from human TBI victims and chronic epilepsy patients. | Cristofori et al., 2001; Varma et al., 2003; Yen et al., 2015; Li et al., 2015; Schiavone et al., 2017 |
| Antioxidant treatments often reduce neurodegeneration and improve functional recovery after experimental TBI | Slemmer et al., 2008 |
| Knock-out, knock-down or pharmacological inhibition of NOX reduces oxidative stress markers, cortical lesion volume, BBB disruption, neurodegeneration, and a range of neurological deficits in diverse TBI models | Choi et al., 2012; Ferreira et al, 2013; Loane et al., 2013; Luo et al., 2013; Song et al., 2013; Lu et al., 2014 |
| ROS generation and oxidative stress are increased after experimental epileptogenic brain insults | Liang et al., 2000; Waldbaum and Patel, 2010; Bhuyan et al., 2015 |
| ROS generation, oxidative stress and NOX are increased in brain tissue from chronic epileptic patients. | Lopez et al., 2007; Rumia et al., 2013; Pecorelli et al.,2015 |
| NOX activation participates in pro-epileptogenic upregulation of NMDA receptor NR1 and NR2B subunits after pilocarpine induced status epilepticus – a model epileptogenic injury. | DiMaio et al., 2011; 2013 |
| Many ion channels/transporters, including the neuronal Na+/K+ pump, are redox modulated. Experimental TBI- and pilocarpine-induced decreases in Na+/K+ pump activity are diminished by NOK inhibition | Bogdonova et al., 2016; Lima et al., 2008; Ferreira et al., 2013;de Freitas et al., 2010 |
| NOX activity both modulates inflammatory signaling that is thought to contribute to epileptogenesis and is modulated by inflammatory mediators. | van der Vliet et al., 2014; Singel and Segal, 2016; Forrester et al., 2018 |
| NOX-derived ROS stimulate microglial activation and promote a proepileptogenic M1-like activation state | Mander et al., 2006; Kumar et al., 2016; Wang et al., 2017 |
| NOX-derived ROS have been implicated in the death or dysfunction of PVINs - a subpopulation of GABAergic interneurons long postulated to play a role in epileptogenesis - after a variety of - epileptogenic experimental brain insults. | Behrens et al., 2007; Ji et al., 2015; Yuan et al. 2015; Liang et al. 2016, Zhang et al., 2016a Schiavone et al., 2009; Liu et al., 2016; Qiu et al., 2016 |
| NOX2 and oxidative stress markers elevated in brain section from human subjects who died from blunt force TBI, and NOX2 immunoreactivity mainly colocalized with PVIN markers. | Schiavone et al., 2017 |
Highlights.
Reactive oxygen species (ROS) and neuroinflammation have been identified as important contributors to both epileptogenesis and the evolving secondary injury after traumatic brain injury (TBI).
After TBI, ROS may contribute to secondary injury and epileptogenesis via both their well-known cytotoxic properties and their effects on a wide range of redox-regulated processes, enzymes and pathways.
Inflammation and oxidative stress/ROS generation are highly interdependent and mutually reinforcing after TBI. Thus, inhibitors targeting either pathway are likely to affect both, and, combination therapies targeting elements of both pathways may exhibit synergistic effects on posttraumatic epileptogenesis and other sequelae of TBI.
The multi-prong approach to target inflammation with prostanoid receptor antagonists and oxidative stress/ROS generation with inhibitors of NADPH oxidase enzymes and myeloperoxidase is a promising strategy to prevent epileptogenesis and reduce secondary injury after TBI.
Acknowledgements
This work was supported by NIH/NINDS grants R21 NS101167 (T.G.& R.D.) and R21 NS085459 (R.D.), NIH/NIA grant U01 AG052460 (T.G.), and CURE Prevention of Acquired Epilepsies Award (R.D.)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest
Authors have no competing and financial interests associated with this article to disclose.
References
- Abdullah Z, Bayraktutan U. NADPH oxidase mediates TNF-α-evoked in vitro brain barrier dysfunction: roles of apoptosis and time. Mol Cell Neurosci. 2014; 61:72–84. doi: 10.1016/j.mcn.2014.06.002. [DOI] [PubMed] [Google Scholar]
- Allan SM, Tyrrell PJ, Rothwell NJ. Interleukin-1 and neuronal injury. Nat Rev Immunol. 2005; 5(8):629–40. [DOI] [PubMed] [Google Scholar]
- Ambrogini P, Minelli A, Galati C, Betti M, Lattanzi D, Ciffolilli S, Piroddi M, Galli F, Cuppini R. Post-seizure α-tocopherol treatment decreases neuroinflammation and neuronal degeneration induced by status epilepticus in rat hippocampus. Mol Neurobiol. 2014; 50(1):246–56. doi: 10.1007/s12035-014-8648-2. [DOI] [PubMed] [Google Scholar]
- Andrioli A, Alonso-Nanclares L, Arellano JI, DeFelipe J. Quantitative analysis of parvalbumin-immunoreactive cells in the human epileptic hippocampus. Neuroscience. 2007; 149(1):131–43. [DOI] [PubMed] [Google Scholar]
- Angeloni C; Prata C; Dalla Sega FV; Piperno R; Hrelia S Traumatic brain injury and NADPH oxidase: a deep relationship. Oxid Med Cell Longev 2015; 2015:370312. doi: 10.1155/2015/370312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annegers JF. The Epidemiology of Epilepsy In: Wyllie E, editors. The Treatment of Epilepsy: Principles and Practice. Baltimore: Williams and Wilkins; 1996:165–172. [Google Scholar]
- Annegers JF, Hauser WA, Coan SP, Rocca WA (1998) A population-based study of seizures after traumatic brain injuries. New Engl J Med 338:20–24. [DOI] [PubMed] [Google Scholar]
- Annunziato L, Pannaccione A, Cataldi M, Secondo A, Castaldo P, Di Renzo G, Taglialatela M. Modulation of ion channels by reactive oxygen and nitrogen species: a pathophysiological role in brain aging? Neurobiol Aging. 2002; 23(5):819–34. [DOI] [PubMed] [Google Scholar]
- Ansari MA, Roberts KN, Scheff SW. Oxidative stress and modification of synaptic proteins in hippocampus after traumatic brain injury. Free Radic Biol Med. 2008;45(4):443–52. doi: 10.1016/j.freeradbiomed.2008.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronica E, Bauer S, Bozzi Y, Caleo M, Dingledine R, Gorter JA, Henshall DC, Kaufer D, Koh S, Löscher W, Louboutin JP, Mishto M, Norwood BA, Palma E, Poulter MO, Terrone G, Vezzani A, Kaminski RM. Neuroinflammatory targets and treatments for epilepsy validated in experimental models. Epilepsia. 2017; 58 Suppl 3:27–38. doi: 10.1111/epi.13783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronica E, Crino PB. Inflammation in epilepsy: clinical observations. Epilepsia. 2011; 52 Suppl 3:26–32. doi: 10.1111/j.1528-1167.2011.03033.x. [DOI] [PubMed] [Google Scholar]
- Aronica E, Ravizza T, Zurolo E, Vezzani A. Astrocyte immune responses in epilepsy. Glia. 2012; 60(8):1258–68. doi: 10.1002/glia.22312. [DOI] [PubMed] [Google Scholar]
- Bedard K, Krause KH. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007; 87(1):245–313 [DOI] [PubMed] [Google Scholar]
- Behrens MM, Ali SS, Dao DN, Lucero J, Shekhtman G, Quick KL, Dugan LL. Ketamine-induced loss of phenotype of fast-spiking interneurons is mediated by NADPH-oxidase. Science. 2007; 318(5856):1645–7 [DOI] [PubMed] [Google Scholar]
- Behrens MM, Ali SS, Dugan LL. Interleukin-6 mediates the increase in NADPH-oxidase in the ketamine model of schizophrenia. J Neurosci. 2008; 28(51):13957–66. doi: 10.1523/JNEUROSCI.4457-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergold PJ Treatment of traumatic brain injury with anti-inflammatory drugs. Exp Neurol 2016; 275 Pt 3: 367–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhuyan P, Patel DC, Wilcox KS, Patel M. Oxidative stress in murine Theiler’svirus-induced temporal lobe epilepsy. Exp Neurol. 2015; 271:329–34. doi: 10.1016/j.expneurol.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biemond P; Swaak AJG; Penders JMA; Beindorff CM; Koster JF Superoxide Production by Polymorphonuclear Leukocytes in Rheumatoid-Arthritis and Osteoarthritis - Invivo Inhibition by the Antirheumatic Drug Piroxicam Due to Interference with the Activation of the Nadph-Oxidase. Annals of the Rheumatic Diseases 1986; 45: 249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdanova A, Petrushanko IY, Hernansanz-Agustín P, Martínez-Ruiz A. “Oxygen Sensing” by Na,K-ATPase: These Miraculous Thiols. Front Physiol. 2016; 7:314. doi: 10.3389/fphys.2016.00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgens RB, Liu-Snyder P. Understanding secondary injury. Q Rev Biol. 2012; 87(2):89–127. [DOI] [PubMed] [Google Scholar]
- Bos A; Wever R; Roos D Characterization and quantification of the peroxidase in human monocytes. Biochim Biophys Acta 1978; 525:37–44. [DOI] [PubMed] [Google Scholar]
- Brennan AM, Suh SW, Won SJ, Narasimhan P, Kauppinen TM, Lee H, Edling Y, Chan PH, Swanson RA. NADPH oxidase is the primary source of superoxide induced by NMDA receptor activation. Nat Neurosci. 2009; 12(7):857–63. doi: 10.1038/nn.2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buriticá E, Villamil L, Guzmán F, Escobar MI, García-Cairasco N, Pimienta HJ. Changes in calcium-binding protein expression in human cortical contusion tissue. J Neurotrauma. 2009; 26(12):2145–55. doi: 10.1089/neu.2009.0894. [DOI] [PubMed] [Google Scholar]
- Cardenas-Rodriguez N, Huerta-Gertrudis B, Rivera-Espinosa L, Montesinos-Correa H, Bandala C, Carmona-Aparicio L, Coballase-Urrutia E. Role of oxidative stress in refractory epilepsy: evidence in patients and experimental models. Int J Mol Sci. 2013; 14(1):1455–76. doi: 10.3390/ijms14011455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhari N; Talwar P; Parimisetty A; Lefebvre d’Hellencourt C; Ravanan P A molecular web: endoplasmic reticulum stress, inflammation, and oxidative stress. Front Cell Neurosci 2014; 8:213. doi: 10.3389/fncel.2014.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H; Kim GS; Okami N; Narasimhan P; Chan PH NADPH oxidase is involved in post-ischemic brain inflammation. Neurobiol Dis 2011; 42:341–8. doi: 10.1016/j.nbd.2011.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu CC; Liao YE; Yang LY; Wang JY; Tweedie D; Karnati HK; Greig NH; Wang JY Neuroinflammation in animal models of traumatic brain injury. J Neurosci Methods 2016; 272:38–49. doi: 10.1016/j.jneumeth.2016.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi BY, Jang BG, Kim JH, Lee BE, Sohn M, Song HK, Suh SW. Prevention of traumatic brain injury-induced neuronal death by inhibition of NADPH oxidase activation. Brain Res. 2012; 1481:49–58. doi: 10.1016/j.brainres.2012.08.032. [DOI] [PubMed] [Google Scholar]
- Choi J, Koh S. Role of brain inflammation in epileptogenesis. Yonsei Med J. 2008; 49(1):1–18. doi: 10.3349/ymj.2008.49.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christman JW, Blackwell TS, Juurlink BH. Redox regulation of nuclear factor kappa B: therapeutic potential for attenuating inflammatory responses. Brain Pathol. 2000; 10(1):153–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Circu ML; Aw TY Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic Biol Med 2010; 48:749–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobley JN, Fiorello ML, Bailey DM. 13 reasons why the brain is susceptible to oxidative stress. Redox Biol. 2018; 15:490–503. doi: 10.1016/j.redox.2018.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooney SJ, Bermudez-Sabogal SL, Byrnes KR. Cellular and temporal expression of NADPH oxidase (NOX) isotypes after brain injury. J Neuroinflammation. 2013; 10:155. doi: 10.1186/1742-2094-10-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius C, Crupi R, Calabrese V, Graziano A, Milone P, Pennisi G, Radak Z, Calabrese EJ, Cuzzocrea S. Traumatic brain injury: oxidative stress and neuroprotection. Antioxid Redox Signal. 2013; 19(8):836–53. doi: 10.1089/ars.2012.4981. [DOI] [PubMed] [Google Scholar]
- Cristofori L, Tavazzi B, Gambin R, Vagnozzi R, Vivenza C, Amorini AM, Di Pierro D, Fazzina G, Lazzarino G. Early onset of lipid peroxidation after human traumatic brain injury: a fatal limitation for the free radical scavenger pharmacological therapy? J Investig Med. 2001; 49(5):450–8. doi: 10.2310/6650.2001.33790. [DOI] [PubMed] [Google Scholar]
- Curia G, Eastman CL, Miller JW, D’Ambrosio R. Modeling Post-Traumatic Epilepsy for Therapy Development In: Laskowitz D, Grant G, editors. Translational Research in Traumatic Brain Injury. Boca Raton (FL): CRC Press/Taylor and Francis Group; 2016. Chapter 10. [PubMed] [Google Scholar]
- D’Ambrosio R, Fairbanks JP, Fender JS, Born DE, Doyle DL, Miller JW. Post-traumatic epilepsy following fluid percussion injury in the rat. Brain. 2004; 127(Pt 2):304–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Ambrosio R, Fender JS, Fairbanks JP, Simon EA, Born DE, Doyle DL, Miller JW. Progression from frontal-parietal to mesial-temporal epilepsy after fluid percussion injury in the rat. Brain. 2005; 128(Pt 1):174–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Freitas RM. Lipoic acid alters delta-aminolevulinic dehydratase, glutathione peroxidase and Na+,K+-ATPase activities and glutathione-reduced levels in rat hippocampus after pilocarpine-induced seizures. Cell Mol Neurobiol. 2010; 30(3):381–7. doi: 10.1007/s10571-009-9460-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng-Bryant Y, Singh IN, Carrico KM, Hall ED. Neuroprotective effects of tempol, a catalytic scavenger of peroxynitrite-derived free radicals, in a mouse traumatic brain injury model. J Cereb Blood Flow Metab. 2008; 28(6):1114–26. doi: 10.1038/jcbfm.2008.10. [DOI] [PubMed] [Google Scholar]
- Devi PU, Manocha A, Vohora D. Seizures, antiepileptics, antioxidants and oxidative stress: an insight for researchers. Expert Opin Pharmacother. 2008; 9(18):3169–77. doi: 10.1517/14656560802568230 [DOI] [PubMed] [Google Scholar]
- Devinsky O, Vezzani A, Najjar S, De Lanerolle NC, Rogawski MA. Glia and epilepsy: excitability and inflammation. Trends Neurosci. 2013; 36(3):174–84. doi: 10.1016/j.tins.2012.11.008. [DOI] [PubMed] [Google Scholar]
- de Vries EE, van den Munckhof B, Braun KP, van Royen-Kerkhof A, de Jager W, Jansen FE. Inflammatory mediators in human epilepsy: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2016; 63:177–90. doi: 10.1016/j.neubiorev.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Diebold BA; Smith SM; Li Y; Lambeth JD NOX2 As a Target for Drug Development: Indications, Possible Complications, and Progress. Antioxid Redox Signal 2015; 23: 375–405. doi: 10.1089/ars.2014.5862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Maio R, Mastroberardino PG, Hu X, Montero L, Greenamyre JT. Pilocapine alters NMDA receptor expression and function in hippocampal neurons: NADPH oxidase and ERK1/2 mechanisms. Neurobiol Dis. 2011; 42(3):482–95. doi: 10.1016/j.nbd.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Di Maio R, Mastroberardino PG, Hu X, Montero LM, Greenamyre JT. Thiol oxidation and altered NR2B/NMDA receptor functions in in vitro and in vivo pilocarpine models: implications for epileptogenesis. Neurobiol Dis. 2013; 49:87–98. doi: 10.1016/j.nbd.2012.07.013. [DOI] [PubMed] [Google Scholar]
- Dinocourt C, Petanjek Z, Freund TF, Ben-Ari Y, Esclapez M. Loss of interneurons innervating pyramidal cell dendrites and axon initial segments in the CA1 region of the hippocampus following pilocarpine-induced seizures. J Comp Neurol. 2003; 459(4):407–25. [DOI] [PubMed] [Google Scholar]
- dos Santos PS, Feitosa CM, Saldanha GB, Tomé Ada R, Feng D, de Freitas RM. Lipoic acid inhibits caspase-dependent and -independent cell death pathways and is neuroprotective against hippocampal damage after pilocarpine-induced seizures. Pharmacol Biochem Behav. 2011; 97(3):531–6. doi: 10.1016/j.pbb.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Dohi K, Ohtaki H, Nakamachi T, Yofu S, Satoh K, Miyamoto K, Song D, Tsunawaki S, Shioda S, Aruga T. Gp91phox (NOX2) in classically activated microglia exacerbates traumatic brain injury. J Neuroinflammation. 2010; 7:41. doi: 10.1186/1742-2094-7-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drexel M, Romanov RA, Wood J, Weger S, Heilbronn R, Wulff P, Tasan RO, Harkany T, Sperk G. Selective Silencing of Hippocampal Parvalbumin Interneurons Induces Development of Recurrent Spontaneous Limbic Seizures in Mice. J Neurosci. 2017; 37(34):8166–8179. doi: 10.1523/JNEUROSCI.3456-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubé C, Richichi C, Bender RA, Chung G, Litt B, Baram TZ. Temporal lobe epilepsy after experimental prolonged febrile seizures: prospective analysis. Brain. 2006; 129(Pt 4):911–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan KM; Lawson JA; Fries S; Koller B; Rader DJ; Smyth EM; Fitzgerald GA COX-2-derived prostacyclin confers atheroprotection on female mice. Science 2004; 306:1954–7. [DOI] [PubMed] [Google Scholar]
- Eyo UB, Murugan M, Wu LJ. Microglia-Neuron Communication in Epilepsy. Glia. 2017; 65(1):5–18. doi: 10.1002/glia.23006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabene PF, Navarro Mora G, Martinello M, Rossi B, Merigo F, Ottoboni L, Bach S, Angiari S, Benati D, Chakir A, Zanetti L, Schio F, Osculati A, Marzola P, Nicolato E, Homeister JW, Xia L, Lowe JB, McEver RP, Osculati F, Sbarbati A, Butcher EC, Constantin G. A role for leukocyte-endothelial adhesion mechanisms in epilepsy. Nat Med. 2008; 14(12):1377–83. doi: 10.1038/nm.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y, Cui C, Liu X, Wu Q, Hu F, Zhang H, Ma Z, Wang L. Protective Role of Apocynin via Suppression of Neuronal Autophagy and TLR4/NF-κB Signaling Pathway in a Rat Model of Traumatic Brain Injury. Neurochem Res. 2017; 42(11):3296–3309. doi: 10.1007/s11064-017-2372-z. [DOI] [PubMed] [Google Scholar]
- Ferreira AP, Rodrigues FS, Della-Pace ID, Mota BC, Oliveira SM, Velho Gewehr Cde C, Bobinski F, de Oliveira CV, Brum JS, Oliveira MS, Furian AF, de Barros CS, Ferreira J, Santos AR, Fighera MR, Royes LF. The effect of NADPH-oxidase inhibitor apocynin on cognitive impairment induced by moderate lateral fluid percussion injury: role of inflammatory and oxidative brain damage. Neurochem Int. 2013; 63(6):583–93. doi: 10.1016/j.neuint.2013.09.012. [DOI] [PubMed] [Google Scholar]
- Fogal B, Hewett SJ. Interleukin-1beta: a bridge between inflammation and excitotoxicity? J Neurochem. 2008; 106(1):1–23. doi: 10.1111/j.1471-4159.2008.05315.x. [DOI] [PubMed] [Google Scholar]
- Forrester SJ, Kikuchi DS, Hernandes MS, Xu Q, Griendling KK. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ Res. 2018; 122(6):877–902. doi: 10.1161/CIRCRESAHA.117.311401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frati A, Cerretani D, Fiaschi AI, Frati P, Gatto V, La Russa R, Pesce A, Pinchi E, Santurro A, Fraschetti F, Fineschi V. Diffuse Axonal Injury and Oxidative Stress: A Comprehensive Review. Int J Mol Sci. 2017; 18(12). pii: E2600. doi: 10.3390/ijms18122600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk CD; FitzGerald GA COX-2 inhibitors and cardiovascular risk. J Cardiovasc Pharmacol 2007; 50:470–9. [DOI] [PubMed] [Google Scholar]
- Ganesh T Prostanoid receptor EP2 as a therapeutic target. J Med Chem 2014; 57: 4454–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gellhaar S, Sunnemark D, Eriksson H, Olson L, Galter D. Myeloperoxidase-immunoreactive cells are significantly increased in brain areas affected by neurodegeneration in Parkinson’s and Alzheimer’s disease. Cell Tissue Res. 2017; 369(3):445–454. doi: 10.1007/s00441-017-2626-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorter JA, van Vliet EA, Aronica E. Status epilepticus, blood-brain barrier disruption, inflammation, and epileptogenesis. Epilepsy Behav. 2015; 49:13–6. doi: 10.1016/j.yebeh.2015.04.047. [DOI] [PubMed] [Google Scholar]
- Grosser T; Yu Y; Fitzgerald GA Emotion recollected in tranquility: lessons learned from the COX-2 saga. Annu Rev Med 2010; 61:17–33. [DOI] [PubMed] [Google Scholar]
- Gu F, Parada I, Yang T, Longo FM, Prince DA. Partial TrkB receptor activation suppresses cortical epileptogenesis through actions on parvalbumin interneurons. Neurobiol Dis. 2018;113:45–58. doi: 10.1016/j.nbd.2018.01.018. [DOI] [PubMed] [Google Scholar]
- Gyoneva S, Ransohoff RM. Inflammatory reaction after traumatic brain injury: therapeutic potential of targeting cell-cell communication by chemokines. Trends Pharmacol Sci. 2015; 36(7):471–80. doi: 10.1016/j.tips.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall ED. The Contributing Role of Lipid Peroxidation and Protein Oxidation in the Course of CNS Injury Neurodegeneration and Neuroprotection: An Overview In: Kobeissy FH, editor. Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Boca Raton (FL): CRC Press/Taylor & Francis; 2015. Chapter 6. [PubMed] [Google Scholar]
- Hampton MB; Kettle AJ; Winterbourn CC Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood 1998; 92:3007–17. [PubMed] [Google Scholar]
- Harijith A, Ebenezer DL, Natarajan V. Reactive oxygen species at the crossroads of inflammasome and inflammation. Front Physiol. 2014; 5:352. doi: 10.3389/fphys.2014.00352. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslund-Vinding J, McBean G, Jaquet V, Vilhardt F. NADPH oxidases in oxidant production by microglia: activating receptors, pharmacology and association with disease. Br J Pharmacol. 2017; 174(12):1733–1749. doi: 10.1111/bph.13425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinemann U, Kaufer D, Friedman A. Blood-brain barrier dysfunction, TGFβ signaling, and astrocyte dysfunction in epilepsy. Glia. 2012; 60(8):1251–7. doi: 10.1002/glia.22311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmy A, De Simoni MG, Guilfoyle MR, Carpenter KL, Hutchinson PJ. Cytokines and innate inflammation in the pathogenesis of human traumatic brain injury. Prog Neurobiol. 2011; 95(3):352–72. doi: 10.1016/j.pneurobio.2011.09.003. [DOI] [PubMed] [Google Scholar]
- Hiragi T, Ikegaya Y, Koyama R. Microglia after Seizures and in Epilepsy. Cells. 2018; 7(4). pii: E26. doi: 10.3390/cells7040026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsiger S, Simmen HP, Werner CM, Wanner GA, Rittirsch D. Danger signals activating the immune response after trauma. Mediators Inflamm. 2012; 2012:315941. doi: 10.1155/2012/315941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hole PS; Darley RL; Tonks A Do reactive oxygen species play a role in myeloid leukemias? Blood 2011; 117:5816–26. [DOI] [PubMed] [Google Scholar]
- Holmin S, Höjeberg B. In situ detection of intracerebral cytokine expression after human brain contusion. Neurosci Lett. 2004; 369(2):108–14. [DOI] [PubMed] [Google Scholar]
- Hsieh TH, Lee HHC, Hameed MQ, Pascual-Leone A, Hensch TK, Rotenberg A. Trajectory of Parvalbumin Cell Impairment and Loss of Cortical Inhibition in Traumatic Brain Injury. Cereb Cortex. 2017; 27(12):5509–5524. doi: 10.1093/cercor/bhw318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inci S, Ozcan OE, Kilinç K. Time-level relationship for lipid peroxidation and the protective effect of alpha-tocopherol in experimental mild and severe brain injury. Neurosurgery. 1998; 43(2):330–5 [DOI] [PubMed] [Google Scholar]
- Iori V, Frigerio F, Vezzani A. Modulation of neuronal excitability by immune mediators in epilepsy. Curr Opin Pharmacol. 2016; 26:118–23. doi: 10.1016/j.coph.2015.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji MH, Qiu LL, Tang H, Ju LS, Sun XR, Zhang H, Jia M, Zuo ZY, Shen JC, Yang JJ. Sepsis-induced selective parvalbumin interneuron phenotype loss and cognitive impairments may be mediated by NADPH oxidase 2 activation in mice. J Neuroinflammation. 2015; 12:182. doi: 10.1186/s12974-015-0401-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang F, Zhang Y, Dusting GJ. NADPH oxidase-mediated redox signaling: roles in cellular stress response, stress tolerance, and tissue repair. Pharmacol Rev. 2011; 63(1):218–42. doi: 10.1124/pr.110.002980. [DOI] [PubMed] [Google Scholar]
- Jiang X, Lachance M, Rossignol E. Involvement of cortical fast-spiking parvalbumin-positive basket cells in epilepsy. Prog Brain Res. 2016; 226:81–126. doi: 10.1016/bs.pbr.2016.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson VE; Stewart JE; Begbie FD; Trojanowski JQ; Smith DH; Stewart W Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Brain 2013; 136:28–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahles T, Brandes RP. NADPH oxidases as therapeutic targets in ischemic stroke. Cell Mol Life Sci. 2012l; 69(14):2345–63. doi: 10.1007/s00018-012-1011-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminski RM, Rogawski MA, Klitgaard H. The potential of antiseizure drugs and agents that act on novel molecular targets as antiepileptogenic treatments. Neurotherapeutics. 2014; 11(2):385–400. doi: 10.1007/s13311-014-0266-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur U, Banerjee P, Bir A, Sinha M, Biswas A, Chakrabarti S. Reactive oxygen species, redox signaling and neuroinflammation in Alzheimer’s disease: the NF-κB connection. Curr Top Med Chem. 2015; 15(5):446–57. [DOI] [PubMed] [Google Scholar]
- Kelly KM, Kharlamov A, Hentosz TM, Kharlamova EA, Williamson JM, Bertram EH 3rd, Kapur J, Armstrong DM. Photothrombotic brain infarction results in seizure activity in aging Fischer 344 and Sprague Dawley rats. Epilepsy Res. 2001; 47(3):189–203. [DOI] [PubMed] [Google Scholar]
- Keyer K; Gort AS; Imlay JA Superoxide and the production of oxidative DNA damage. J Bacteriol 1995; 177:6782–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Jang BG, Choi BY, Kim HS, Sohn M, Chung TN, Choi HC, Song HK, Suh SW. Post-treatment of an NADPH oxidase inhibitor prevents seizure-induced neuronal death. Brain Res. 2013; 1499:163–72. doi: 10.1016/j.brainres.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Klebanoff SJ Myeloperoxidase: friend and foe. J Leukoc Biol 2005, 77, 598–625. [DOI] [PubMed] [Google Scholar]
- Kleinschnitz C, Grund H, Wingler K, Armitage ME, Jones E, Mittal M, Barit D, Schwarz T, Geis C, Kraft P, Barthel K, Schuhmann MK, Herrmann AM, Meuth SG, Stoll G, Meurer S, Schrewe A, Becker L, Gailus-Durner V, Fuchs H, Klopstock T, de Angelis MH, Jandeleit-Dahm K, Shah AM, Weissmann N, Schmidt HH. Post-stroke inhibition of induced NADPH oxidase type 4 prevents oxidative stress and neurodegeneration. PLoS Biol. 2010. September 21;8(9):e1000479. doi: 10.1371/journal.pbio.1000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline AE, Leary JB, Radabaugh HL, Cheng JP, Bondi CO. Combination therapies for neurobehavioral and cognitive recovery after experimental traumatic brain injury: Is more better? Prog Neurobiol. 2016; 142:45–67. doi: 10.1016/j.pneurobio.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kontos HA; Povlishock JT Oxygen radicals in brain injury. Cent Nerv Syst Trauma 1986; 3:257–63. [DOI] [PubMed] [Google Scholar]
- Kontos HA; Wei EP Superoxide production in experimental brain injury. J Neurosurg 1986; 64: 803–7. [DOI] [PubMed] [Google Scholar]
- Kovac S, Dinkova Kostova AT, Herrmann AM, Melzer N, Meuth SG, Gorji A. Metabolic and Homeostatic Changes in Seizures and Acquired Epilepsy-Mitochondria, Calcium Dynamics and Reactive Oxygen Species. Int J Mol Sci. 2017; 18(9). pii: E1935. doi: 10.3390/ijms18091935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A, Barrett JP, Alvarez-Croda DM, Stoica BA, Faden AI, Loane DJ. NOX2 drives M1-like microglial/macrophage activation and neurodegeneration following experimental traumatic brain injury. Brain Behav Immun. 2016; 58:291–309. doi: 10.1016/j.bbi.2016.07.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunz T; Marklund N; Hillered L; Oliw EH Cyclooxygenase-2, prostaglandin synthases, and prostaglandin H2 metabolism in traumatic brain injury in the rat. J Neurotrauma 2002; 19:1051–64. [DOI] [PubMed] [Google Scholar]
- Laird MD, Shields JS, Sukumari-Ramesh S, Kimbler DE, Fessler RD, Shakir B, Youssef P, Yanasak N, Vender JR, Dhandapani KM. High mobility group box protein-1 promotes cerebral edema after traumatic brain injury via activation of toll-like receptor 4. Glia. 2014; 62(1):26–38. doi: 10.1002/glia.22581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambeth JD NOX enzymes and the biology of reactive oxygen. Nat Rev Immunol 2004; 4:181–9. [DOI] [PubMed] [Google Scholar]
- Lambeth JD Nox enzymes, ROS, and chronic disease: An example of antagonistic pleiotropy. Free Radical Biology and Medicine 2007; 43:332–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambeth JD, Neish AS. Nox enzymes and new thinking on reactive oxygen: a double-edged sword revisited. Annu Rev Pathol. 2014; 9:119–45. doi: 10.1146/annurevpathol-012513-104651. [DOI] [PubMed] [Google Scholar]
- Leifer D, Cole DG, Kowall NW. Neuropathologic asymmetries in the brain of a patient with a unilateral status epilepticus. J Neurol Sci. 1991; 103(2):127–35. [DOI] [PubMed] [Google Scholar]
- Leo P, McCrea M. Epidemiology In: Laskowitz D, Grant G, editors. Translational Research in Traumatic Brain Injury. Boca Raton (FL): CRC Press/Taylor and Francis Group; 2016. Chapter 1. [PubMed] [Google Scholar]
- Li Z, Tian F, Shao Z, Shen X, Qi X, Li H, Wang Z, Chen G. Expression and clinical significance of non-phagocytic cell oxidase 2 and 4 after human traumatic brain injury. Neurol Sci. 2015; 36(1):61–71. doi: 10.1007/s10072-014-1909-z. [DOI] [PubMed] [Google Scholar]
- Liang D, Li G, Liao X, Yu D, Wu J, Zhang M. Developmental loss of parvalbumin-positive cells in the prefrontal cortex and psychiatric anxiety after intermittent hypoxia exposures in neonatal rats might be mediated by NADPH oxidase-2. Behav Brain Res. 2016; 296:134–140. doi: 10.1016/j.bbr.2015.08.033. [DOI] [PubMed] [Google Scholar]
- Liang LP, Ho YS, Patel M. Mitochondrial superoxide production in kainate-induced hippocampal damage. Neuroscience. 2000;101(3):563–70. [DOI] [PubMed] [Google Scholar]
- Lima FD, Souza MA, Furian AF, Rambo LM, Ribeiro LR, Martignoni FV, Hoffmann MS, Fighera MR, Royes LF, Oliveira MS, de Mello CF. Na+,K+-ATPase activity impairment after experimental traumatic brain injury: relationship to spatial learning deficits and oxidative stress. Behav Brain Res. 2008; 193(2):306–10. doi: 10.1016/j.bbr.2008.05.013. [DOI] [PubMed] [Google Scholar]
- Liu FF, Yang LD, Sun XR, Zhang H, Pan W, Wang XM, Yang JJ, Ji MH, Yuan HM. NOX2 Mediated-Parvalbumin Interneuron Loss Might Contribute to Anxiety-Like and Enhanced Fear Learning Behavior in a Rat Model of Post-Traumatic Stress Disorder. Mol Neurobiol. 2016; 53(10):6680–6689. [DOI] [PubMed] [Google Scholar]
- Lloyd E, Somera-Molina K, Van Eldik LJ, Watterson DM, Wainwright MS. Suppression of acute proinflammatory cytokine and chemokine upregulation by post-injury administration of a novel small molecule improves long-term neurologic outcome in a mouse model of traumatic brain injury. J Neuroinflammation. 2008; 5:28. doi: 10.1186/1742-2094-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loane DJ; Kumar A; Stoica BA; Cabatbat R; Faden AI Progressive neurodegeneration after experimental brain trauma: association with chronic microglial activation. J Neuropathol Exp Neurol 2014; 73:14–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loane DJ, Stoica BA, Byrnes KR, Jeong W, Faden AI. Activation of mGluR5 and inhibition of NADPH oxidase improves functional recovery after traumatic brain injury. J Neurotrauma. 2013; 30(5):403–12. doi: 10.1089/neu.2012.2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López J, González ME, Lorigados L, Morales L, Riverón G, Bauzá JY. Oxidative stress markers in surgically treated patients with refractory epilepsy. Clin Biochem. 2007; 40(5–6):292–8. [DOI] [PubMed] [Google Scholar]
- Löscher W, Klitgaard H, Twyman RE, Schmidt D. New avenues for anti-epileptic drug discovery and development. Nat Rev Drug Discov. 2013; 12(10):757–76. doi: 10.1038/nrd4126. [DOI] [PubMed] [Google Scholar]
- Löscher W, Schmidt D. Modern antiepileptic drug development has failed to deliver: ways out of the current dilemma. Epilepsia. 2011; 52(4):657–78. doi: 10.1111/j.1528-1167.2011.03024.x. [DOI] [PubMed] [Google Scholar]
- Lu XY, Wang HD, Xu JG, Ding K, Li T. NADPH oxidase inhibition improves neurological outcome in experimental traumatic brain injury. Neurochem Int. 2014; 69:14–9. doi: 10.1016/j.neuint.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Luo T, Wu J, Kabadi SV, Sabirzhanov B, Guanciale K, Hanscom M, Faden J, Cardiff K, Bengson CJ, Faden AI. Propofol limits microglial activation after experimental brain trauma through inhibition of nicotinamide adenine dinucleotide phosphate oxidase. Anesthesiology. 2013;119(6):1370–88. doi: 10.1097/ALN.0000000000000020. [DOI] [PubMed] [Google Scholar]
- Ma MW; Wang J; Dhandapani KM; Wang R; Brann DW NADPH oxidases in traumatic brain injury - Promising therapeutic targets? Redox Biol 2018; 16:285–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma MW; Wang J; Zhang Q; Wang R; Dhandapani KM; Vadlamudi RK; Brann DW NADPH oxidase in brain injury and neurodegenerative disorders. Mol Neurodegener 2017; 12:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGregor DG, Higgins MJ, Jones PA, Maxwell WL, Watson MW, Graham DI, Stone TW. Ascorbate attenuates the systemic kainate-induced neurotoxicity in the rat hippocampus. Brain Res. 1996; 727(1–2):133–44. [DOI] [PubMed] [Google Scholar]
- Malkov A, Ivanov AI, Latyshkova A, Bregestovski P, Zilberter M, Zilberter Y. Activation of nicotinamide adenine dinucleotide phosphate oxidase is the primary trigger of epileptic seizures in rodent models. Ann Neurol. 2019; 85(6):907–920. doi: 10.1002/ana.25474. [DOI] [PubMed] [Google Scholar]
- Malle E; Marsche G; Arnhold J; Davies MJ Modification of low-density lipoprotein by myeloperoxidase-derived oxidants and reagent hypochlorous acid. Biochim Biophys Acta 2006; 1761:392–415. [DOI] [PubMed] [Google Scholar]
- Malle E; Woenckhaus C; Waeg G; Esterbauer H; Grone EF; Grone HJ Immunological evidence for hypochlorite-modified proteins in human kidney. Am J Pathol 1997; 150:603–15. [PMC free article] [PubMed] [Google Scholar]
- Mander PK, Jekabsone A, Brown GC. Microglia proliferation is regulated by hydrogen peroxide from NADPH oxidase. J Immunol. 2006; 176(2):1046–52. [DOI] [PubMed] [Google Scholar]
- Maraldi T Natural compounds as modulators of NADPH oxidases. Oxid Med Cell Longev 2013; 2013:271602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marklund N, Clausen F, McIntosh TK, Hillered L. Free radical scavenger posttreatment improves functional and morphological outcome after fluid percussion injury in the rat. J Neurotrauma. 2001; 18(8):821–32. [DOI] [PubMed] [Google Scholar]
- Marx M, Haas CA, Häussler U. Differential vulnerability of interneurons in the epileptic hippocampus. Front Cell Neurosci. 2013; 7:167. doi: 10.3389/fncel.2013.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez DR, Cherian L, Moore N, Arora T, Liu PK, Robertson CS. Oxidative DNA lesions in a rodent model of traumatic brain injury. J Trauma. 2004; 56(6):1235–40. [DOI] [PubMed] [Google Scholar]
- Mesenge C; Charriaut-Marlangue C; Verrecchia C; Allix M; Boulu RR; Plotkine M Reduction of tyrosine nitration after N(omega)-nitro-L-arginine-methylester treatment of mice with traumatic brain injury. Eur J Pharmacol 1998; 353:53–7. [DOI] [PubMed] [Google Scholar]
- Mohamadpour M, Whitney K, Bergold PJ. The Importance of Therapeutic Time Window in the Treatment of Traumatic Brain Injury. Front Neurosci. 2019; 13:07. doi: 10.3389/fnins.2019.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morganti-Kossmann MC, Semple BD, Hellewell SC, Bye N, Ziebell JM. The complexity of neuroinflammation consequent to traumatic brain injury: from research evidence to potential treatments. Acta Neuropathol. 2019; 137(5):731–755. doi: 10.1007/s00401-018-1944-6. [DOI] [PubMed] [Google Scholar]
- Mustafa AG; Singh IN; Wang J; Carrico KM; Hall ED Mitochondrial protection after traumatic brain injury by scavenging lipid peroxyl radicals. J Neurochem 2010; 114:271–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayernia Z, Jaquet V, Krause KH. New insights on NOX enzymes in the central nervous system. Antioxid Redox Signal. 2014; 20(17):2815–37. doi: 10.1089/ars.2013.5703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisimoto Y, Diebold BA, Cosentino-Gomes D, Lambeth JD. Nox4: a hydrogen peroxide-generating oxygen sensor. Biochemistry. 2014. August 12;53(31):5111–20. doi: 10.1021/bi500331y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordzieke DE, Medraño-Fernandez I. The Plasma Membrane: A Platform for Intra- and Intercellular Redox Signaling. Antioxidants (Basel). 2018; 7(11). pii: E168. doi: 10.3390/antiox7110168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott L, McClain CJ, Gillespie M, Young B. Cytokines and metabolic dysfunction after severe head injury. J Neurotrauma. 1994; 11(5):447–72. [DOI] [PubMed] [Google Scholar]
- Pandya JD, Readnower RD, Patel SP, Yonutas HM, Pauly JR, Goldstein GA, Rabchevsky AG, Sullivan PG. N-acetylcysteine amide confers neuroprotection, improves bioenergetics and behavioral outcome following TBI. Exp Neurol. 2014; 257:106–13. doi: 10.1016/j.expneurol.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker TM, Nguyen AH, Rabang JR, Patil AA, Agrawal DK. The danger zone: Systematic review of the role of HMGB1 danger signalling in traumatic brain injury. Brain Inj. 2017; 31(1):2–8. doi: 10.1080/02699052.2016.1217045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel M Mitochondrial dysfunction and oxidative stress: cause and consequence of epileptic seizures. Free Radic Biol Med. 2004; 37(12):1951–62 [DOI] [PubMed] [Google Scholar]
- Pecorelli A, Natrella F, Belmonte G, Miracco C, Cervellati F, Ciccoli L, Mariottini A, Rocchi R, Vatti G, Bua A, Canitano R, Hayek J, Forman HJ, Valacchi G. NADPH oxidase activation and 4-hydroxy-2-nonenal/aquaporin-4 adducts as possible new players in oxidative neuronal damage presents in drug-resistant epilepsy. Biochim Biophys Acta. 2015. March;1852(3):507–19. doi: 10.1016/j.bbadis.2014.11.016. [DOI] [PubMed] [Google Scholar]
- Paudel YN, Shaikh MF, Chakraborti A, Kumari Y, Aledo-Serrano Á, Aleksovska K, Alvim MKM, Othman I. HMGB1: A Common Biomarker and Potential Target for TBI, Neuroinflammation, Epilepsy, and Cognitive Dysfunction. Front Neurosci. 2018; 12:628. doi: 10.3389/fnins.2018.00628. eCollection 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paudel YN, Semple BD, Jones NC, Othman I, Shaikh MF. High mobility group box 1 (HMGB1) as a novel frontier in epileptogenesis: from pathogenesis to therapeutic approaches. J Neurochem. 2019. January 15. doi: 10.1111/jnc.14663. [DOI] [PubMed] [Google Scholar]
- Pauletti A, Terrone G, Shekh-Ahmad T, Salamone A, Ravizza T, Rizzi M, Pastore A, Pascente R, Liang LP, Villa BR, Balosso S, Abramov AY, van Vliet EA, Del Giudice E, Aronica E, Antoine DJ, Patel M, Walker MC, Vezzani A. Targeting oxidative stress improves disease outcomes in a rat model of acquired epilepsy. Brain. 2017; 140(7):1885–1899. doi: 10.1093/brain/awx117. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Pavlov I, Huusko N, Drexel M, Kirchmair E, Sperk G, Pitkänen A, Walker MC. Progressive loss of phasic, but not tonic, GABAA receptor-mediated inhibition in dentate granule cells in a model of post-traumatic epilepsy in rats. Neuroscience. 2011; 194:208–19. doi: 10.1016/j.neuroscience.2011.07.074. [DOI] [PubMed] [Google Scholar]
- Pearson JN, Rowley S, Liang LP, White AM, Day BJ, Patel M. Reactive oxygen species mediate cognitive deficits in experimental temporal lobe epilepsy. Neurobiol Dis. 2015; 82:289–297. doi: 10.1016/j.nbd.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson-Smith JN, Patel M. Metabolic Dysfunction and Oxidative Stress in Epilepsy. Int J Mol Sci. 2017; 18(11). pii: E2365. doi: 10.3390/ijms18112365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pestana RR, Kinjo ER, Hernandes MS, Britto LR. Reactive oxygen species generated by NADPH oxidase are involved in neurodegeneration in the pilocarpine model of temporal lobe epilepsy. Neurosci Lett. 2010; 484(3):187–91. doi: 10.1016/j.neulet.2010.08.049. [DOI] [PubMed] [Google Scholar]
- Peterson D, Weir EK. Redox signal transduction: reductive reasoning. J Lab Clin Med. 2002; 140(2):73–8. [DOI] [PubMed] [Google Scholar]
- Petkova Z, Tchekalarova J, Pechlivanova D, Moyanova S, Kortenska L, Mitreva R,Popov D, Markova P, Lozanov V, Atanasova D, Lazarov N, Stoynev A. Treatment with melatonin after status epilepticus attenuates seizure activity and neuronal damage but does not prevent the disturbance in diurnal rhythms and behavioral alterations in spontaneously hypertensive rats in kainate model of temporal lobe epilepsy. Epilepsy Behav. 2014; 31:198–208. doi: 10.1016/j.yebeh.2013.12.013. [DOI] [PubMed] [Google Scholar]
- Ping X, Jin X. Chronic Posttraumatic Epilepsy following Neocortical Undercut Lesion in Mice. PLoS One. 2016; 11(6):e0158231. doi: 10.1371/journal.pone.0158231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisoschi AM, Pop A. The role of antioxidants in the chemistry of oxidative stress: A review. Eur J Med Chem. 2015. June 5;97:55–74. doi: 10.1016/j.ejmech.2015.04.040. [DOI] [PubMed] [Google Scholar]
- Prins M, Greco T, Alexander D, Giza CC. The pathophysiology of traumatic brain injury at a glance. Dis Model Mech. 2013; 6(6):1307–15. doi: 10.1242/dmm.011585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu LL, Luo D, Zhang H, Shi YS, Li YJ, Wu D, Chen J, Ji MH, Yang JJ. Nox-2-Mediated Phenotype Loss of Hippocampal Parvalbumin Interneurons Might Contribute to Postoperative Cognitive Decline in Aging Mice. Front Aging Neurosci. 2016; 8:234 eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan Y; Jiang J; Dingledine R EP2 receptor signaling pathways regulate classical activation of microglia. J Biol Chem 2013; 288:9293–302. doi: 10.1074/jbc.M113.455816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quillinan N, Herson PS, Traystman RJ. Neuropathophysiology of Brain Injury. Anesthesiol Clin. 2016; 34(3):453–64. doi: 10.1016/j.anclin.2016.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rada B, Leto TL. Oxidative Innate Immune Defenses by Nox/Duox Family NADPH Oxidases. Trends in Innate Immunity. Contrib Microbiol. 2008; 15:164–187. doi: 10.1159/000136357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakhade SN, Klein PM, Huynh T, Hilario-Gomez C, Kosaras B, Rotenberg A, Jensen FE. Development of later life spontaneous seizures in a rodent model of hypoxia-induced neonatal seizures. Epilepsia. 2011; 52(4):753–65. doi: 10.1111/j.1528-1167.2011.02992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravizza T, Terrone G, Salamone A, Frigerio F, Balosso S, Antoine DJ, Vezzani A. High Mobility Group Box 1 is a novel pathogenic factor and a mechanistic biomarker for epilepsy. Brain Behav Immun. 2018; 72:14–21. doi: 10.1016/j.bbi.2017.10.008. [DOI] [PubMed] [Google Scholar]
- Ray SK, Dixon CE, Banik NL. Molecular mechanisms in the pathogenesis of traumatic brain injury. Histol Histopathol. 2002; 17(4):1137–52. doi: 10.14670/HH-17.1137. [DOI] [PubMed] [Google Scholar]
- Reid AY, Bragin A, Giza CC, Staba RJ, Engel J Jr. The progression of electrophysiologic abnormalities during epileptogenesis after experimental traumatic brain injury. Epilepsia. 2016; 57(10):1558–1567. doi: 10.1111/epi.13486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robel S Astroglial Scarring and Seizures: A Cell Biological Perspective on Epilepsy. Neuroscientist. 2017; 23(2):152–168. doi: 10.1177/1073858416645498. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Rodríguez A, Egea-Guerrero JJ, Murillo-Cabezas F, Carrillo-Vico A. Oxidative stress in traumatic brain injury. Curr Med Chem. 2014; 21(10):1201–11. [DOI] [PubMed] [Google Scholar]
- Rojas A; Chen D; Ganesh T; Varvel NH; Dingledine R The COX-2/prostanoid signaling cascades in seizure disorders. Expert Opin Ther Targets 2019; 23:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowley S, Patel M. Mitochondrial involvement and oxidative stress in temporal lobe epilepsy. Free Radic Biol Med. 2013; 62:121–131. doi: 10.1016/j.freeradbiomed.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumià J, Marmol F, Sanchez J, Giménez-Crouseilles J, Carreño M, Bargalló N, Boget T, Pintor L, Setoain X, Donaire A, Saez GT, Ribalta T, Ferrer E, Puig-Parellada P. Oxidative stress markers in the neocortex of drug-resistant epilepsy patients submitted to epilepsy surgery. Epilepsy Res. 2013; 107(1–2):75–81. doi: 10.1016/j.eplepsyres.2013.08.020. [DOI] [PubMed] [Google Scholar]
- Ruppel RA, Clark RS, Bayir H, Satchell MA, Kochanek PM. Critical mechanisms of secondary damage after inflicted head injury in infants and children. Neurosurg Clin N Am. 2002. April;13(2):169–82. [DOI] [PubMed] [Google Scholar]
- Ryu JK; Tran KC; McLarnon JG Depletion of neutrophils reduces neuronal degeneration and inflammatory responses induced by quinolinic acid in vivo. Glia 2007; 55:439–51. [DOI] [PubMed] [Google Scholar]
- Schiavone S, Neri M, Trabace L, Turillazzi E. The NADPH oxidase NOX2 mediates loss of parvalbumin interneurons in traumatic brain injury: human autoptic immunohistochemical evidence. Sci Rep. 2017; 7(1):8752. doi: 10.1038/s41598-017-09202-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiavone S, Sorce S, Dubois-Dauphin M, Jaquet V, Colaianna M, Zotti M, Cuomo V, Trabace L, Krause KH. Involvement of NOX2 in the development of behavioral and pathologic alterations in isolated rats. Biol Psychiatry. 2009; 66(4):384–92. doi: 10.1016/j.biopsych.2009.04.033. [DOI] [PubMed] [Google Scholar]
- Schieber M, Chandel NS. ROS function in redox signaling and oxidative stress. Curr Biol. 2014. May 19; 24(10):R453–62. doi: 10.1016/j.cub.2014.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schütze S, Wiegmann K, Machleidt T, Krönke M. TNF-induced activation of NF-kappa B. Immunobiology. 1995; 193(2–4):193–203. [DOI] [PubMed] [Google Scholar]
- Segal AW The NADPH oxidase and chronic granulomatous disease. Mol Med Today 1996; 2:129–35. [DOI] [PubMed] [Google Scholar]
- Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, Steiner C. Incidence of long-term disability following traumatic brain injury hospitalization, United States, 2003. J Head Trauma Rehabil. 2008; 23(2):123–31. doi: 10.1097/01.HTR.0000314531.30401.39. [DOI] [PubMed] [Google Scholar]
- Serrano GE; Lelutiu N; Rojas A; Cochi S; Shaw R; Makinson CD; Wang D; FitzGerald GA; Dingledine R Ablation of cyclooxygenase-2 in forebrain neurons is neuroprotective and dampens brain inflammation after status epilepticus. J Neurosci 2011; 31:14850–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin EJ, Jeong JH, Chung YH, Kim WK, Ko KH, Bach JH, Hong JS, Yoneda Y, Kim HC. Role of oxidative stress in epileptic seizures. Neurochem Int. 2011; 59(2):122–37. doi: 10.1016/j.neuint.2011.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shojo H; Borlongan CV; Mabuchi T Genetic and Histological Alterations Reveal Key Role of Prostaglandin Synthase and Cyclooxygenase 1 and 2 in Traumatic Brain Injury-Induced Neuroinflammation in the Cerebral Cortex of Rats Exposed to Moderate Fluid Percussion Injury. Cell Transplant 2017; 26:1301–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon DW; McGeachy MJ; Bayir H; Clark RSB; Loane DJ; Kochanek PM The far-reaching scope of neuroinflammation after traumatic brain injury. Nat Rev Neurol 2017; 13:572. [DOI] [PubMed] [Google Scholar]
- Singel KL, Segal BH. NOX2-dependent regulation of inflammation. Clin Sci (Lond). 2016; 130(7):479–90. doi: 10.1042/CS20150660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh IN; Gilmer LK; Miller DM; Cebak JE; Wang JA; Hall ED Phenelzine mitochondrial functional preservation and neuroprotection after traumatic brain injury related to scavenging of the lipid peroxidation-derived aldehyde 4-hydroxy-2-nonenal. J Cereb Blood Flow Metab 2013; 33:593–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirokmány G, Donkó Á, Geiszt M. Nox/Duox Family of NADPH Oxidases: Lessons from Knockout Mouse Models. Trends Pharmacol Sci. 2016. April;37(4):318–327. doi: 10.1016/j.tips.2016.01.006. [DOI] [PubMed] [Google Scholar]
- Slemmer JE, Shacka JJ, Sweeney MI, Weber JT. Antioxidants and free radical scavengers for the treatment of stroke, traumatic brain injury and aging. Curr Med Chem. 2008;15(4):404–14. [DOI] [PubMed] [Google Scholar]
- Sloviter RS. Permanently altered hippocampal structure, excitability, and inhibition after experimental status epilepticus in the rat: the “dormant basket cell” hypothesis and its possible relevance to temporal lobe epilepsy.Hippocampus. 1991; 1(1):41–66. [DOI] [PubMed] [Google Scholar]
- Somayaji MR, Przekwas AJ, Gupta RK. Combination Therapy for Multi-Target Manipulation of Secondary Brain Injury Mechanisms. Curr Neuropharmacol. 2018;16(4):484–504. doi: 10.2174/1570159X15666170828165711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song SX, Gao JL, Wang KJ, Li R, Tian YX, Wei JQ, Cui JZ. Attenuation of brain edema and spatial learning deficits by the inhibition of NADPH oxidase activity using apocynin following diffuse traumatic brain injury in rats. Mol Med Rep. 2013; 7(1):327–31. doi: 10.3892/mmr.2012.1147. [DOI] [PubMed] [Google Scholar]
- Sorce S; Krause KH NOX Enzymes in the Central Nervous System: From Signaling to Disease. Antioxidants & Redox Signaling 2009; 11:2481–2504. [DOI] [PubMed] [Google Scholar]
- Sorce S, Stocker R, Seredenina T, Holmdahl R, Aguzzi A, Chio A, Depaulis A, Heitz F, Olofsson P, Olsson T, Duveau V, Sanoudou D, Skosgater S, Vlahou A, Wasquel D, Krause KH, Jaquet V. NADPH oxidases as drug targets and biomarkers in neurodegenerative diseases: What is the evidence? Free Radic Biol Med. 2017; 112:387–396. doi: 10.1016/j.freeradbiomed.2017.08.006. [DOI] [PubMed] [Google Scholar]
- Sorg O, Horn TF, Yu N, Gruol DL, Bloom FE. Inhibition of astrocyte glutamate uptake by reactive oxygen species: role of antioxidant enzymes. Mol Med. 1997; 3(7):431–40. [PMC free article] [PubMed] [Google Scholar]
- Stewart KA, Wilcox KS, Fujinami RS, White HS. Development of postinfection epilepsy after Theiler’s virus infection of C57BL/6 mice. J Neuropathol Exp Neurol. 2010; 69(12):1210–9. doi: 10.1097/NEN.0b013e3181ffc420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stocchetti N, Zanier ER. Chronic impact of traumatic brain injury on outcome and quality of life: a narrative review. Crit Care. 2016; 20(1):148. doi: 10.1186/s13054-016-1318-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss KI, Barbe MF, Marshall RM, Raghupathi R, Mehta S, and Narayan RK Prolonged cyclooxygenase-2 induction in neurons and glia following traumatic brain injury in the rat. J Neurotrauma 2000; 17:695–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun XR, Zhang H, Zhao HT, Ji MH, Li HH, Wu J, Li KY, Yang JJ. Amelioration of oxidative stress-induced phenotype loss of parvalbumin interneurons might contribute to the beneficial effects of environmental enrichment in a rat model of post-traumatic stress disorder. Behav Brain Res. 2016; 312:84–92. doi: 10.1016/j.bbr.2016.06.016. [DOI] [PubMed] [Google Scholar]
- Tchekalarova J, Petkova Z, Pechlivanova D, Moyanova S, Kortenska L, Mitreva R, Lozanov V, Atanasova D, Lazarov N, Stoynev A. Prophylactic treatment with melatonin after status epilepticus: effects on epileptogenesis, neuronal damage, and behavioral changes in a kainate model of temporal lobe epilepsy. Epilepsy Behav. 2013; 27(1):174–87. doi: 10.1016/j.yebeh.2013.01.009. [DOI] [PubMed] [Google Scholar]
- Toklu HZ, Tümer N. Oxidative Stress, Brain Edema, Blood–Brain Barrier Permeability, and Autonomic Dysfunction from Traumatic Brain Injury In: Kobeissy FH, editor. Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Boca Raton (FL): CRC Press/Taylor & Francis; 2015. Chapter 5. [Google Scholar]
- Toth Z, Hollrigel GS, Gorcs T, Soltesz I. Instantaneous perturbation of dentate interneuronal networks by a pressure wave-transient delivered to the neocortex. J Neurosci. 1997; 17(21):8106–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toulmond S, Rothwell NJ. Interleukin-1 receptor antagonist inhibits neuronal damage caused by fluid percussion injury in the rat. Brain Res. 1995; 671(2):261–6. [DOI] [PubMed] [Google Scholar]
- Tyurin VA, Tyurina YY, Borisenko GG, Sokolova TV, Ritov VB, Quinn PJ, Rose M, Kochanek P, Graham SH, Kagan VE. Oxidative stress following traumatic brain injury in rats: quantitation of biomarkers and detection of free radical intermediates. J Neurochem. 2000; 75(5):2178–89. [DOI] [PubMed] [Google Scholar]
- Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007; 39(1):44–84. [DOI] [PubMed] [Google Scholar]
- van der Hel WS, Hessel EV, Bos IW, Mulder SD, Verlinde SA, van Eijsden P, de Graan PN. Persistent reduction of hippocampal glutamine synthetase expression after status epilepticus in immature rats. Eur J Neurosci. 2014; 40(12):3711–9. doi: 10.1111/ejn.12756. [DOI] [PubMed] [Google Scholar]
- van der Vliet A, Janssen-Heininger YM. Hydrogen peroxide as a damage signal in tissue injury and inflammation: murderer, mediator, or messenger? J Cell Biochem. 2014; 115(3):427–35. doi: 10.1002/jcb.24683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Vliet EA, Aronica E, Gorter JA. Blood-brain barrier dysfunction, seizures and epilepsy. Semin Cell Dev Biol. 2015; 38:26–34. doi: 10.1016/j.semcdb.2014.10.003. [DOI] [PubMed] [Google Scholar]
- van Vliet EA, Aronica E, Vezzani A, Ravizza T. Review: Neuroinflammatory pathways as treatment targets and biomarker candidates in epilepsy: emerging evidence from preclinical and clinical studies. Neuropathol Appl Neurobiol. 2018; 44(1):91–111. doi: 10.1111/nan.12444. [DOI] [PubMed] [Google Scholar]
- Varma S, Janesko KL, Wisniewski SR, Bayir H, Adelson PD, Thomas NJ, Kochanek PM. F2-isoprostane and neuron-specific enolase in cerebrospinal fluid after severe traumatic brain injury in infants and children. J Neurotrauma. 2003; 20(8):781–6. [DOI] [PubMed] [Google Scholar]
- Venereau E, Casalgrandi M, Schiraldi M, Antoine DJ, Cattaneo A, De Marchis F, Liu J, Antonelli A, Preti A, Raeli L, Shams SS, Yang H, Varani L, Andersson U, Tracey KJ, Bachi A, Uguccioni M, Bianchi ME. Mutually exclusive redox forms of HMGB1 promote cell recruitment or proinflammatory cytokine release. J Exp Med. 2012; 209(9):1519–28. doi: 10.1084/jem.20120189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venereau E, De Leo F, Mezzapelle R, Careccia G, Musco G, Bianchi ME. HMGB1 as biomarker and drug target. Pharmacol Res. 2016; 111:534–544. doi: 10.1016/j.phrs.2016.06.031. [DOI] [PubMed] [Google Scholar]
- Vezzani A, French J, Bartfai T, Baram TZ. The role of inflammation in epilepsy. Nat Rev Neurol. 2011; 7(1):31–40. doi: 10.1038/nrneurol.2010.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezzani A, Friedman A, Dingledine RJ. The role of inflammation in epileptogenesis. Neuropharmacology. 2013; 69:16–24. doi: 10.1016/j.neuropharm.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezzani A, Fujinami RS, White HS, Preux PM, Blümcke I, Sander JW, Löscher W. Infections, inflammation and epilepsy. Acta Neuropathol. 2016; 131(2):211–234. doi: 10.1007/s00401-015-1481-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vezzani A, Granata T. Brain inflammation in epilepsy: experimental and clinical evidence. Epilepsia. 2005; 46(11):1724–43. [DOI] [PubMed] [Google Scholar]
- Vezzani A, Viviani B. Neuromodulatory properties of inflammatory cytokines and their impact on neuronal excitability. Neuropharmacology. 2015; 96(Pt A):70–82. doi: 10.1016/j.neuropharm.2014.10.027. [DOI] [PubMed] [Google Scholar]
- Wada K; Chatzipanteli K; Kraydieh S; Busto R; Dietrich WD Inducible nitric oxide synthase expression after traumatic brain injury and neuroprotection with aminoguanidine treatment in rats. Neurosurgery 1998; 43: 1427–36. [DOI] [PubMed] [Google Scholar]
- Waldbaum S, Patel M. Mitochondrial dysfunction and oxidative stress: a contributing link to acquired epilepsy? J Bioenerg Biomembr. 2010; 42(6):449–55. doi: 10.1007/s10863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Ma MW, Dhandapani KM, Brann DW. Regulatory role of NADPH oxidase 2 in the polarization dynamics and neurotoxicity of microglia/macrophages after traumatic brain injury. Free Radic Biol Med. 2017; 113:119–131. doi: 10.1016/j.freeradbiomed.2017.09.017. [DOI] [PubMed] [Google Scholar]
- Wang W, Zinsmaier AK, Firestone E, Lin R, Yatskievych TA, Yang S, Zhang J, Bao S. Blocking Tumor Necrosis Factor-Alpha Expression Prevents Blast-Induced Excitatory/Inhibitory Synaptic Imbalance and Parvalbumin-Positive Interneuron Loss in the Hippocampus. J Neurotrauma. 2018a; 35(19):2306–2316. doi: 10.1089/neu.2018.5688. [DOI] [PubMed] [Google Scholar]
- Wang Y, Liang J, Chen L, Shen Y, Zhao J, Xu C, Wu X, Cheng H, Ying X, Guo Y, Wang S, Zhou Y, Wang Y, Chen Z. Pharmaco-genetic therapeutics targeting parvalbumin neurons attenuate temporal lobe epilepsy. Neurobiol Dis. 2018b; 117:149–160. doi: 10.1016/j.nbd.2018.06.006. [DOI] [PubMed] [Google Scholar]
- Webster KM, Sun M, Crack P, O’Brien TJ, Shultz SR, Semple BD. Inflammation in epileptogenesis after traumatic brain injury. J Neuroinflammation. 2017; 14(1):10. doi: 10.1186/s12974-016-0786-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss SJ; Reddy VY Tissue Destruction by Neutrophils - Reply. New England Journal of Medicine 1989; 321:329–329. [DOI] [PubMed] [Google Scholar]
- Werner C, Engelhard K. Pathophysiology of traumatic brain injury. Br J Anaesth. 2007; 99(1):4–9. [DOI] [PubMed] [Google Scholar]
- White HS, Löscher W. Searching for the ideal antiepileptogenic agent in experimental models: single treatment versus combinatorial treatment strategies. Neurotherapeutics. 2014; 11(2):373–84. doi: 10.1007/s13311-013-0250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HS, Smith MD, Wilcox KS. Mechanisms of action of antiepileptic drugs. Int Rev Neurobiol. 2007; 81:85–110. [DOI] [PubMed] [Google Scholar]
- Williams S, Hamil N, Abramov AY, Walker MC, Kovac S. Status epilepticus results in persistent overproduction of reactive oxygen species, inhibition of which is neuroprotective. Neuroscience. 2015. September 10;303:160–5. doi: 10.1016/j.neuroscience.2015.07.005. [DOI] [PubMed] [Google Scholar]
- Wu Z, Xu Q, Zhang L, Kong D, Ma R, Wang L. Protective effect of resveratrol against kainate-induced temporal lobe epilepsy in rats. Neurochem Res. 2009; 34(8):1393–400. doi: 10.1007/s11064-009-9920-0. [DOI] [PubMed] [Google Scholar]
- Yang CM, Hsieh HL, Yu PH, Lin CC, Liu SW. IL-1β Induces MMP-9-Dependent Brain Astrocytic Migration via Transactivation of PDGF Receptor/NADPH Oxidase 2-Derived Reactive Oxygen Species Signals. Mol Neurobiol. 2015; 52(1):303–17. doi: 10.1007/s12035-014-8838-y. [DOI] [PubMed] [Google Scholar]
- Yang H, Antoine DJ, Andersson U, Tracey KJ. The many faces of HMGB1: molecular structure-functional activity in inflammation, apoptosis, and chemotaxis. J Leukoc Biol. 2013; 93(6):865–73. doi: 10.1189/jlb.1212662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen HC, Chen TW, Yang TC, Wei HJ, Hsu JC, Lin CL. Levels of F2-isoprostanes,F4-neuroprostanes, and total nitrate/nitrite in plasma and cerebrospinal fluid of patients with traumatic brain injury. Free Radic Res. 2015; 49(12):1419–30. doi: 10.3109/10715762.2015.1080363. [DOI] [PubMed] [Google Scholar]
- Yuan L, Wu J, Liu J, Li G, Liang D. Intermittent Hypoxia-Induced Parvalbumin-Immunoreactive Interneurons Loss and Neurobehavioral Impairment is Mediated by NADPH-Oxidase-2. Neurochem Res. 2015; 40(6):1232–42. doi: 10.1007/s11064-015-1586-1. [DOI] [PubMed] [Google Scholar]
- Zhang H, Sun XR, Wang J, Zhang ZZ, Zhao HT, Li HH, Ji MH, Li KY, Yang JJ. Reactive Oxygen Species-mediated Loss of Phenotype of Parvalbumin Interneurons Contributes to Long-term Cognitive Impairments After Repeated Neonatal Ketamine Exposures. Neurotox Res. 2016a; 30(4):593–605. [DOI] [PubMed] [Google Scholar]
- Zhang L, Liu J, Cheng C, Yuan Y, Yu B, Shen A, Yan M. The neuroprotective effect of pyrroloquinoline quinone on traumatic brain injury. J Neurotrauma. 2012; 29(5):851–64. doi: 10.1089/neu.2011.1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang QG, Laird MD, Han D, Nguyen K, Scott E, Dong Y, Dhandapani KM, Brann DW. Critical role of NADPH oxidase in neuronal oxidative damage and microglia activation following traumatic brain injury. PLoS One. 2012;7(4):e34504. doi: 10.1371/journal.pone.0034504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Seeburg DP, Pulli B, Wojtkiewicz GR, Bure L, Atkinson W, Schob S, Iwamoto Y, Ali M, Zhang W, Rodriguez E, Milewski A, Keliher EJ, Wang C, Pan Y, Swirski FK, Chen JW. Myeloperoxidase Nuclear Imaging for Epileptogenesis.Radiology. 2016b; 278(3):822–30. doi: 10.1148/radiol.2015141922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu ZQ, Armstrong DL, Hamilton WJ, Grossman RG. Disproportionate loss of CA4 parvalbumin-immunoreactive interneurons in patients with Ammon’s horn sclerosis. J Neuropathol Exp Neurol. 1997; 56(9):988–98. [DOI] [PubMed] [Google Scholar]
- Ziebell JM, Morganti-Kossmann MC. Involvement of pro- and anti-inflammatory cytokines and chemokines in the pathophysiology of traumatic brain injury. Neurotherapeutics. 2010; 7(1):22–30. doi: 10.1016/j.nurt.2009.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorov DB, Juhaszova M, Sollott SJ. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev. 2014; 94(3):909–50. doi: 10.1152/physrev.00026.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]