Abstract
Objective
To examine whether early follow-up with primary care or neurology is associated with lower all-cause readmissions within 30 and 90 days after acute ischemic stroke admission.
Methods
We performed a retrospective cohort study of patients who were discharged home after acute ischemic stroke, identified by ICD-9 and ICD-10 codes, using PharMetrics, a nationally representative claims database of insured Americans from 2009 to 2015. The primary predictor was outpatient primary care or neurology follow-up within 30 and 90 days of discharge, and the primary outcome was all-cause 30- and 90-day readmissions. Multivariable Cox models were used with primary care and neurology visits specified as time-dependent covariates, with adjustment for patient demographics, comorbid conditions, and stroke severity measures.
Results
The cohort included 14,630 patients. Readmissions within 30 days occurred in 7.3% of patients, and readmissions within 90 days occurred in 13.7% of patients. By 30 days, 59.3% had a primary care visit, and 24.4% had a neurology visit. Primary care follow-up was associated with reduced 30-day readmissions (hazard ratio [HR] 0.84, 95% confidence interval [CI] 0.72–0.98). Primary care follow-up before 90 days did not reach significance (HR 0.92, 95% CI 0.83–1.03). Neurology follow-up was not associated with reduced readmissions within 30 or 90 days (HR 1.05, 95% CI; HR 1.00, 95% CI, respectively).
Conclusion
Early outpatient follow-up with primary care is associated with a reduction in 30-day hospital readmissions. Early outpatient follow-up may represent an important opportunity for intervention after acute stroke admissions.
Stroke affects ≈795,000 people in the United States each year and leaves up to half with lasting disability.1,2 Within 1 year after stroke, 5% to 14% of survivors will have a recurrent stroke, and 20% to 50% of patients will be readmitted to the hospital.3–5 Hospital readmission within 30 days is a quality metric established by the Centers for Medicare and Medicaid Services.6 Stroke readmissions within 30 days are common and associated with high morbidity, mortality, and cost.7–9 Studies have identified factors associated with readmission after stroke, including older age and longer length of stay.8,10–13 However, most risk factors are nonmodifiable, making targeted interventions challenging.
The transition between inpatient and outpatient care represents an especially vulnerable period for patients after stroke, and current guidelines provide little information on follow-up visits.14–16 Clinical studies in patients who were recently hospitalized for heart failure, various surgeries, and general medical conditions have found that early follow-up may improve outcomes and reduce readmissions.17–19
A recent study looking at the Medicare population found that early outpatient visits with either primary care or neurology after an acute ischemic stroke admission were associated with a small reduction (2%) in readmission at 30 days.20 However, that study20 looked only at readmission at 30 days, and the population was Medicare beneficiaries ≥65 years old. The objective of this study is to assess the association between early outpatient follow-up and readmission within both 30 and 90 days in a population of insured patients with stroke from 18 to 89 years old.
Methods
Study cohort
This is a retrospective cohort study of a large integrated commercial database, PharMetrics Plus, administrated by IMS Health, which includes all paid medical and pharmacy claims for >90 million members from >80 health plans. The dataset is considered representative of the US insured population with respect to age and sex.21 This dataset has previously been described in other studies.22–24
Patients were included if they were between 18 and 89 years old, diagnosed with an acute ischemic stroke as the primary diagnosis during an inpatient admission (using ICD-9 codes 433.x1, 434.x1 from 2009 until 2014 and ICD-9 code 436 or ICD-10 code I63 in 2015), and enrolled for at least 6 months before and 3 months after the initial stroke admission. Patients were excluded from the study if they were discharged to a postacute care facility (i.e., acute and subacute rehabilitation or long-term care hospital) or had an unknown discharge disposition, were transferred from another medical facility, or left against medical advice during the initial stroke admission. We chose to exclude patients who were discharged to postacute care facilities because we were unable to assess which patients had access to follow-up visits. Some facilities have physicians who monitor patients on a periodic basis, while other may provide transportation to follow-up care. This information cannot be captured in an administrative database and would introduce significant heterogeneity to the study sample.
All inpatient claims between January 1, 2009, and December 31, 2015, were used to identify the cohort of patients with acute ischemic stroke hospitalizations. Only the first inpatient admission for stroke for each patient during the study period was considered. This also includes 6 months of observation before the first stroke admission in which the patient could not have had a stroke admission.
Standard protocol approvals, registrations, and patient consents
This study protocol, which relies on a deidentified national database, was deemed exempt by the University of Colorado Institutional Review Board.
Covariates of interest
Separate binary primary predictor variables were used to determine whether patients had outpatient visits within 30 days to primary care and neurology in the case of 30-day readmissions. Similarly, binary primary predictor variables were used to determine primary care and neurology follow-up visits within 90 days in the case of 90-day readmissions. Primary care was defined as general practice, family medicine, internal medicine (excluding subspecialist visits), and geriatric medicine. Outpatient visits were defined from claims billing data as a visit that occurred after the date of discharge in a noninpatient and non–emergency department setting.
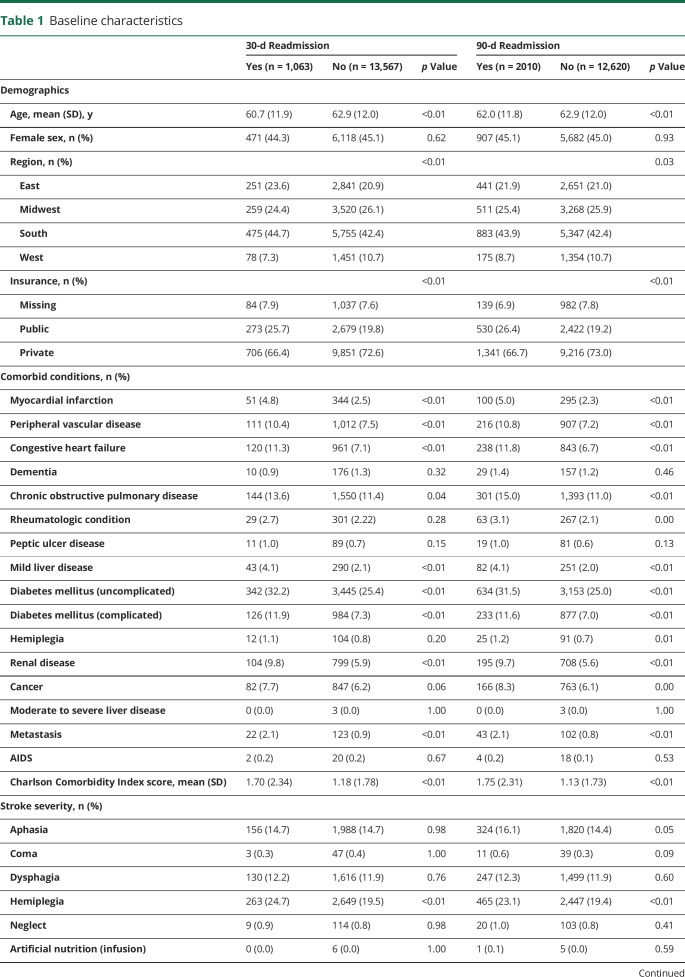
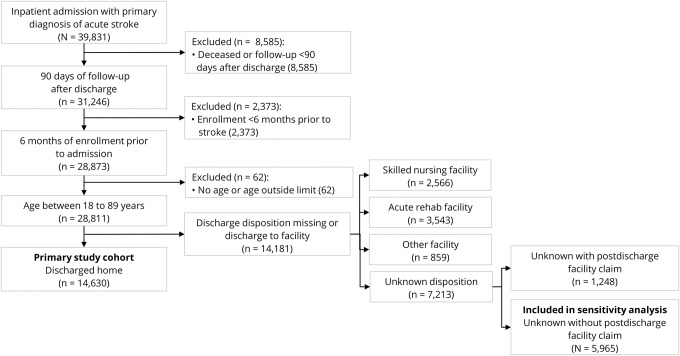
As many potential confounders were accounted for as possible, including patient demographics, comorbid conditions, length of stay of the stroke admission, and stroke severity using the Stroke Administrative Severity Index (SASI).25 These characteristics are listed in table 1. Patient demographics, including age, sex, region of residence, and insurance type, were extracted from the demographics file. Of note, race was not included in the demographics dataset, so this factor could not be used in the analysis. Comorbid conditions were identified with the Charlson Comorbidity Index on the basis of both inpatient and outpatient claims data in the 6 months before the index admission, using both ICD-9 and ICD-10 codes.26,27 Length of stay was determined by subtracting the discharge date from the admission date to determine the number of midnights the patient was admitted. Hence, a patient admitted and discharged on the same calendar day would yield a length of stay of 0 days. Stroke severity was determined with the SASI, which is a validated tool to control for stroke severity and is correlated to 30-day postdischarge outcomes.25 The SASI is a proxy variable constructed from symptoms (aphasia, coma, dysarthria, hemiplegia, and neglect) and procedures (infusion and tracheostomy) occurring during the index admission and predicts the NIH Stroke Scale score at hospital discharge (C statistic 0.83).25 The overall score was used to adjust for stroke severity in the Cox model.
Table 1.
Baseline characteristics
Primary outcome
Stratified analysis was done for readmissions within 30 and 90 days. The 2 binary primary outcome variables analyzed were all-cause readmission within 30 and 90 days. Readmission was defined as any inpatient visit in a short-term acute care hospital with an admission date greater than the discharge date of the index hospitalization, regardless of the length of stay. All patients with a readmission within 30 days also satisfied readmission within 90 days. Time to readmission was calculated on the basis of the discharge date from the initial stroke admission. To determine the most common causes for readmission, all ICD-9 and ICD-10 admission diagnostic codes with a frequency of ≥10 were analyzed. The frequency of the equivalent ICD-9 or ICD-10 code and any closely related diagnostic codes was grouped together to come up with a unifying readmission diagnosis. Readmission diagnoses and their related ICD-9 and ICD-10 codes are noted in table 2.
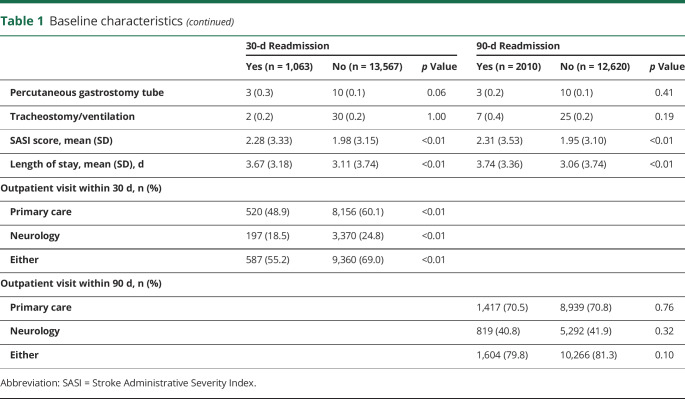
Table 2.
Readmission diagnoses
Statistical analysis
Descriptive statistics were used to summarize the patient cohort for readmissions within both 30 and 90 days. The relationship between outpatient visits and readmissions was analyzed with Cox models with time and type of follow-up visits specified as time-dependent variables. The follow-up visit should affect only the hazard of readmission between the time it occurs and the readmission event, so outpatient visit is a time-varying variable. Separate models were constructed for 30- and 90-day readmissions. Patient demographics, comorbid conditions, length of stay, and stroke severity are previously noted. Because the Charlson Comorbidity Index and SASI scores were ordinal variables with a large number of levels, their levels were collapsed into a smaller number of categories. Length of stay was logarithmically transformed because of skew and adjusted for in the model. All variables were used regardless of statistical significance, and no model-based variable selection procedures were used.
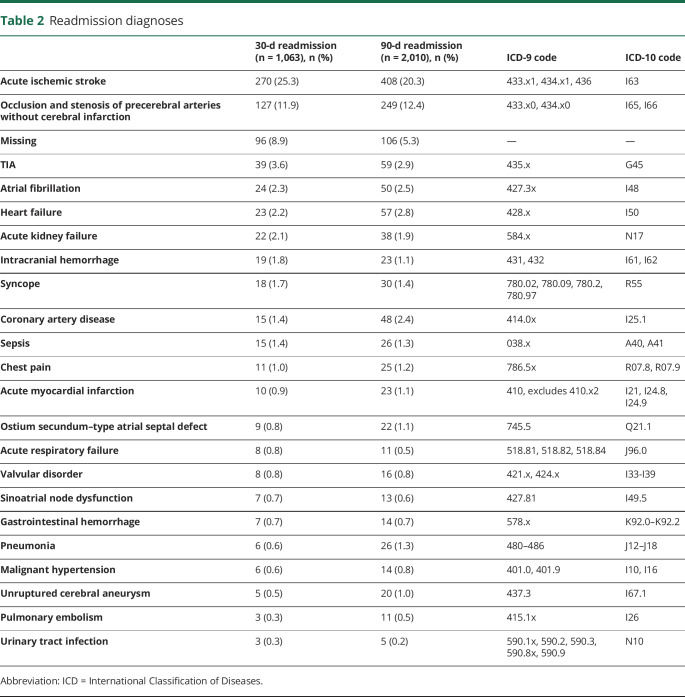
An additional sensitivity analysis was conducted due to the high proportion of patients who were missing disposition (n = 7,213 or 25.0%) on discharge from the index stroke admission. Among the patients without a discharge disposition, we excluded those with any claims to a facility (excluding inpatient admissions) within 2 days of discharge that lasted for ≥1 days. Sensitivity analyses also partitioned patients into <65 and >65 years of age. Separate models were fitted for each age group, as well as a model with an age group effect modifier to test for interactions. This remaining population was included in a sensitivity analysis using the model described previously with the addition of the population that was discharged home (figure 1). We used a significance level of 0.05 and 2-sided tests for all hypotheses. All analyses were performed with SAS software, release 9.4 (SAS Institute, Inc, Cary, NC).
Figure 1. Patient inclusion flowchart.
Exclusions and number excluded are displayed. Rehab = rehabilitation.
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Results
There were 39,831 patients (50.2% male, mean age 65 years) with an acute stroke admission during the study period (figure 1). After application of the exclusion criteria for the follow-up period, enrollment before stroke, and age, 28,811 patients remained. Of these, 14,630 (50.8%) were discharged to home, 2,566 (8.9%) to a skilled nursing facility, 3,543 (12.3%) to acute rehabilitation, 111 (0.4%) to a long-term acute care facility, and 748 (2.6%) to another facility; 7,213 (25.0%) had an unknown disposition.
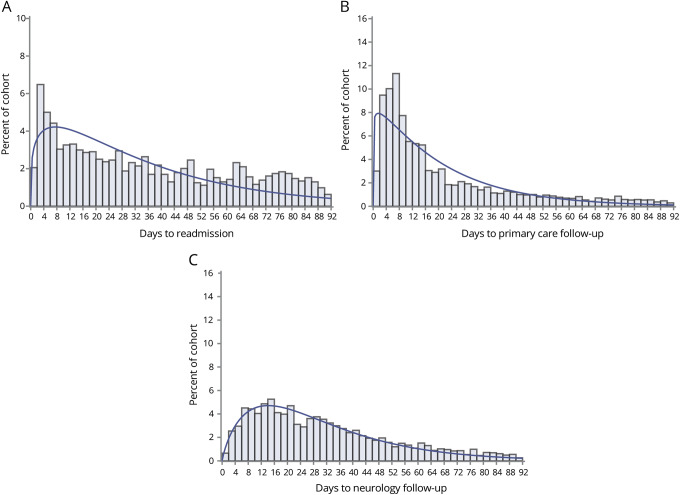
Patient demographics are displayed in table 1. Of the 14,630 patients discharged home, the overall readmission risk at 30 days was 7.3%, and the readmission risk at 90 days was 13.7%. Of the 1,063 patients who were readmitted within 30 days, the median number of days to readmission was 11 (interquartile range [IQR] 5–19) days. Of the 2,010 patients who were readmitted within 90 days, the median number of days to readmission was 28 (IQR 10–56, figure 2, A). Primary care visits within 30 and 90 days occurred in 8,676 (59.3%) and 10,356 (70.8%) patients at a median of 7 (IQR 4–14) and 9 (IQR 5–20) days, respectively, among patients who had a primary care visit within the time window (figure 2, B). Neurology follow-up within 30 and 90 days occurred in 3,567 (24.4%) and 6,111 (41.8%) patients at a median of 15 (IQR 9–22) and 26 (IQR 14–42) days, respectively, among patients who had a neurology visit within the time window (figure 2, C).
Figure 2. Time distribution to readmission, primary care follow-up, and neurology follow-up.
Denominator is the entire cohort. (A) Days to first readmission (curve is gamma distribution with theta 0, alpha 1.2, and sigma 28.8). (B) Days to primary care follow-up (curve is gamma distribution with theta 0, alpha 1.1, sigma 15.2). (C) Days to neurology follow-up (curve is gamma distribution with theta 0, alpha 1.9, sigma 16.3).
The majority of follow-ups within both 30 and 90 days occurred first with primary care. Follow-up at 30 days with either primary care or neurology occurred in 9,947 of 14,630 (68.0%). Among patients who had had a primary or neurology follow-up, 8,118 of 9,947 (81.6%) were seen first by their primary care provider, while 1737 of 9,947 (17.5%) were first seen by a neurologist and 92 of 9,947 (0.9%) were seen on the same day by their primary care provider and neurologist. The median time to first 30-day follow-up was 8 (IQR 4–14) days. Follow-up at 90 days with either primary care or neurology occurred in 11,870 of 14,630 (81.1%), with 9,283 of 11,870 (78.2%) first seen by primary care, 2,485 of 11,870 (20.9%) first seen by neurology, and 102 of 11,870 (0.9%) seen on the same day by primary care and neurology. In the first 90 days after hospitalization, the median time to first 90-day follow-up was 10 (IQR 5–21) days.
Various factors were associated with unadjusted readmission at 30 and 90 days, as listed in table 1. Patients with 30- and 90-day readmissions tended to be younger and less likely to have private insurance. Patients with 30- and 90-day readmissions had a higher Charlson Comorbidity Index score (p < 0.01). Comorbid conditions such as liver, renal, or heart disease and cancer were associated with readmissions at both 30 and 90 days. Patients with 30- and 90-day readmissions had higher SASI scores (p < 0.01) and were more likely to be hemiplegic and to have a longer length of stay during the index stroke admission. Fewer patients with 30-day readmissions had a follow-up with primary care or neurology compared to those who were not readmitted (p < 0.01 for both). There were no differences between the proportion of primary care or neurology follow-up between patients with or without 90-day readmissions (p = 0.76 and p = 0.32, respectively).
The most common reasons for readmissions were categorized by evaluating all ICD-9 and ICD-10 codes (and closely related codes) with a frequency >10 (table 2). The most common reason for readmission was recurrent stroke (ICD-9 codes 433.x1, 434.x1, 436; ICD-10 code I63) and occlusion of a precerebral artery without ischemia (ICD-9 codes 433.x0, 434.x0; ICD-10 codes I65, I66) for both 30 and 90-day readmissions. Of the readmissions for occlusions of a precerebral artery without stroke, some of these patients likely had a planned readmission for a symptomatic carotid stenosis. Hence, of this population, carotid endarterectomy or carotid stenting occurred in 32 of 127 readmissions within 30 days and 78 of 249 readmissions within 90 days.
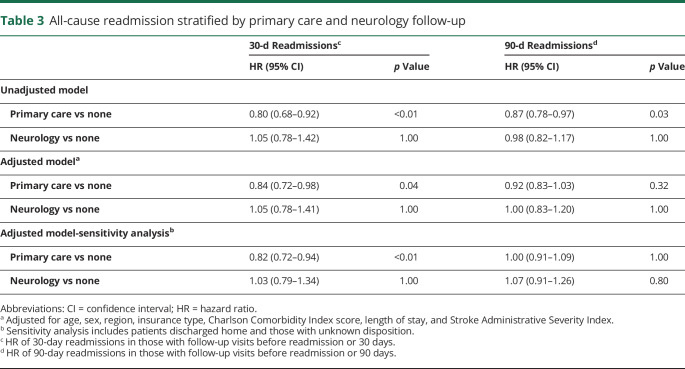
Table 3 describes 30- and 90-day readmission risk, according to whether patients had a follow-up visit with either primary care or neurology. The follow-up visit variables were time varying. The adjusted model includes Cox proportional hazard regressions adjusted for age, sex, region, insurance type, Charlson Comorbidity Index score, SASI score, and length of stay. The Bonferroni correction was used for multiple comparisons. For the first 30-day period, having a primary care visit significantly reduced the hazard of readmission (hazard ratio [HR] 0.84, 95% confidence interval [CI] 0.72–0.98, p = 0.04). In other words, the hazard of readmission for the first 30-day period decreased by an estimated 16% after patients visited a primary care doctor. The same benefit was not seen with 30-day neurology follow-up (HR 1.05, 95% CI 0.78–1.41, p = 1.00). Follow-up with either primary care or neurology within 30 days did not reach significance (HR 0.87, 95% CI 0.76–1.01 p = 0.07). There was no association between primary care or neurology follow-up at 90 days and readmission at 90 days (HR 0.92, 95% CI 0.83–1.03, p = 0.32; and HR 1.00, 95% CI 0.83–1.20, p = 1.00, respectively).
Table 3.
All-cause readmission stratified by primary care and neurology follow-up
Given that 25% of patients have an unknown discharge disposition, many of them could potentially have been discharged home, creating a significant source of bias for the study. After the exclusion of patients who were missing a discharge disposition but had claims for a facility-based admission (other than acute inpatient stay) within 2 days of discharge and lasting for ≥1 days, the number of patients with unknown disposition went down to 5,965 or 20.7%. In the sensitivity analysis, the cohort included all patients discharged to home or with an unknown discharge disposition (n = 20,595, table 3). The association between primary care follow-up and reduced readmissions within 30 days remained stable (HR 0.82, 95% CI 0.72–0.94, p < 0.01). There was still no association between neurology follow-up and readmissions within 30 days. Neither primary care nor neurology follow-up was associated with a change in readmissions at 90 days.
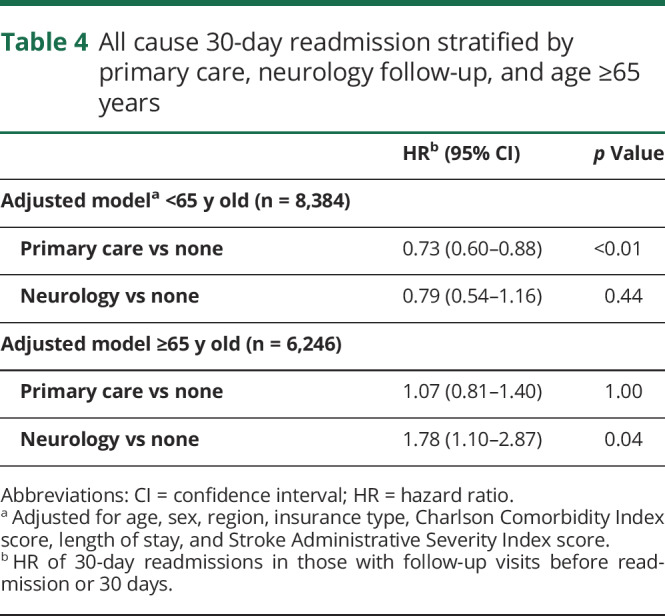
In the primary cohort of patients who discharged home, we investigated the effect of age and geography on the association of follow-up visits within 30-day readmissions (table 4). When separate models were fitted by age group (<65 and ≥65 years), we found that for patients <65 years of age, there was a stronger association with primary care follow-up and reduced 30-day readmissions (HR 0.73, 95% CI 0.60–0.88, p < 0.01). In the <65-year-old cohort, for 30-day readmissions, the estimated HR for neurology follow up was similar (0.79), but because the CI was wide, there was no statistically significant association (p = 0.44). In those patients ≥65 years of age, there was no association between primary care follow-up and 30-day readmissions, but neurology follow-up was associated with increased 30-day readmissions (HR 1.78, 95% CI 1.10–2.87, p = 0.04). The omnibus χ2 tests for geographic region found significant differences based on geography for the <65-year-old group only. Univariate pair-wise comparisons among regions found increased readmission hazard for the East and South compared to the Midwest (HR 1.44, 95% CI 1.10–1.88, p < 0.01; and HR 1.27, 95% CI 1.06–1.54, p = 0.01) respectively. Readmission hazard in the East was marginally statistically nonsignificantly greater than in the West (HR 1.44, 95% CI 1.00–2.07, p = 0.05).
Table 4.
All cause 30-day readmission stratified by primary care, neurology follow-up, and age ≥65 years
Discussion
Among patients discharged home after stroke, early outpatient follow-up with primary care, but not neurology, was associated with a reduction in readmissions at 30 days. An association was not seen with primary care or neurology follow-up and readmission at 90 days. These data suggest that early follow-up with primary care could help to prevent readmissions at 30 days. One-third of 30-day readmissions in this study were due to recurrent stroke and occlusion or stenosis of precerebral arteries. Because the risk of recurrent stroke is highest in the first 30 days after an index stroke (rate per month ≈0.1 in the first month and 0.01 in the first year),5 early follow-up with primary care may be reinforcing risk factor modifications such as blood pressure control, thereby preventing readmissions.28–30 The recent Platelet-Oriented Inhibition in New TIA and Minor Stroke Trial (POINT) found that most recurrent strokes occurred during the first week after the initial minor stroke or TIA and that the higher frequency of events during the first week and 30 days made the benefit of treatment (dual antiplatelet vs aspirin alone) during this period of time more significant than in the first 90 days 31 Similarly, our study found that early follow-up is more effective at preventing readmissions in the first 30 days compared with the first 90 days. This is consistent with previous studies suggesting that inadequate care coordination or medication-related adverse reactions are strong contributors to 30-day readmissions.32,33 These factors, which can often be addressed at an early follow-up visit, would be much less likely to contribute to 90-day readmissions.
It is not completely clear why primary care follow-up had a stronger association than neurology follow-up in reduced 30-day readmissions. It is possible that primary care providers are better at addressing outstanding medical problems, whereas neurology follow-up may be more focused, addressing only pertinent neurologic issues. However, a more likely explanation for this finding is that primary care follow-up occurred earlier than neurology follow-up. The median time to primary care follow-up was 7 (IQR 4–14) days, which is earlier than the median time to readmissions, which was 11 (IQR 5–19) days. The median time to neurology follow-up was not until 15 (IQR 9–22) days and would have occurred after the majority of readmissions. The number of patients who had follow-up with neurology was less than half of those with primary care follow-up. Furthermore, there were very few early neurology follow-ups (i.e., <6 days after discharge). Hence, even after controlling for time to follow-up visits in our model, the benefit of an earlier neurology follow-up visit is difficult to tease out. In addition, the information from an administrative database is limited. There may be aspects of the content of the primary care visit that are crucial to avoiding readmissions, and this issue warrants further investigation.
The results of the sensitivity analysis, which also included patients whose discharge disposition was unknown, were consistent with the observations in the primary analysis of patients who were known to be discharged home. Patients who were discharged to a facility are less like to receive outpatient follow-up and more likely to be readmitted. Hence, we excluded patients with an unknown disposition and subsequent claim for facility-based care. We cannot account for patients with an unknown disposition whose initial admission was paid for with their commercial insurance but who were discharged to a facility that was paid for with an alternate payer (e.g., Medicare or Medicaid). These patients would be unintentionally captured in the sensitivity analysis.
Early follow-up after a stroke admission could represent an important, low-cost opportunity for intervention. In our study of insured Americans, only 59.3% had follow-up with primary care and 24.4% had follow-up with neurology within 30 days of their stroke. Other transitions of care models have been investigated in stroke with some success. For example, Andersen et al.4 investigated home visits by a physician or physical therapist compared to standard of care after stroke and found reduced readmissions in both intervention arms (p = 0.03). Implementing new transitional care models can be highly effective but would require additional resources.34 Meanwhile, early follow-up with primary care in patients who are already insured may be implemented quickly.
One recent study by Terman et al.20 also investigated the utility of early primary care and neurology follow-up among Medicare recipients (≥65 years old) who were hospitalized for stroke. They found that patients who had a primary care or neurology follow-up had a slightly lower adjusted hazard of readmission (HR 0.98, 95% CI 0.97–0.98 for both). In this study, when the cohort was stratified by age ≥65 years, we found that primary care visits were not associated with reduced readmissions within 30 days. In addition, neurology follow-up in those ≥65 years of age was associated with increased readmissions within 30 days. The latter finding is disconcerting, but there are likely several confounding factors. First, elderly patients with a specialist visit within 30 days are more likely to be sicker and to have acute outstanding medical issues and hence are at higher risk for readmission. The neurologist is also more likely to recognize focal neurologic symptoms that would warrant readmission, because the most common reason for readmissions was recurrent strokes. Second, because the majority of patients ≥65 years of age also have access to Medicare, some readmissions may have been billed directly to Medicare and missed by this study. Missing some readmissions in the ≥65-year-old group may also explain our finding that there were more readmissions in adults <65 than those ≥65 years of age, while previous studies found that readmissions rates increased with age.35 Lastly, all patients ≥65 years of age in this database also have commercial insurance or had Medicare administered through a commercial insurance. This may represent a different population than patients ≥65 years of age using primarily Medicare, as in the Terman et al. study. However, we do not know in which direction confounding may have been introduced by these last 2 factors. More investigation is necessary to look at the potential association between neurology follow-up and readmissions in this population. Although early follow-up with neurology for the ≥65-year-old group may not reduce readmissions, in patients <65 years of age, follow-up with primary care was associated with a 25% reduction in readmissions within 30 days, underscoring the potential benefit of early primary care follow-up.
This study has several limitations. First, not all potential confounders were controlled for such as socioeconomic, racial, or hospital factors measuring the quality of stroke care. Therefore, an underlying causative relationship between early follow-up and readmission cannot definitively be established. Second, although this study can be generalized in the sense that the sample was nationwide and included a large number of patients, these results are limited to patients with insurance who survived at least 90 days and were discharged home. Readmission rates are higher among uninsured Americans and those with more disability or discharged to a facility.35 Consequently, more research needs to be directed toward the relationship between early follow-up and readmission in these populations. Third, we did not consider the competing risk of death, because mortality could prevent outpatient follow-up and readmissions. We do not have reliable data on why enrollment was dropped, which could be due to either death or changes in insurance. The previous study on the Medicare population did not find an effect from competing risk of death. Because all patients were discharged home, death resulting from stroke is not likely to represent a significant source of bias.20 Lastly, although early follow-up is associated with lower rates of readmission at 30 days, the time frame during which this follow-up should occur is unclear. The median time to readmissions was 11 days, whereas the median primary care follow-up occurred at 7 days. Given that most recurrent strokes occur in the first week, early follow-up should likely occur within the first week after stroke, but more research is necessary to clarify this question.
Thirty-day outpatient follow-up with primary care was associated with a significant reduction in 30-day hospital readmissions among insured American adults who were discharged from hospital to home. This study identifies a potential opportunity for future interventions aimed at reducing the cost and burden of readmissions after acute stroke. However, more work is needed to determine the optimal timing and content of early follow-up visits.
Glossary
- CI
confidence interval
- HR
hazard ratio
- ICD
International Classification of Diseases
- IQR
interquartile range
- POINT
Platelet-Oriented Inhibition in New TIA and Minor Stroke Trial
- SASI
Stroke Administrative Severity Index
Appendix. Authors
Footnotes
Editorial, page 509
Study funding
Funding provided by American Stroke Association Bugher Foundation Grant (14BFSC17680001) (Drs. Leppert and Poisson).
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Yang Q, Tong X, Schieb L, et al. Vital signs: recent trends in stroke death rates—United States, 2000–2015. MMWR Morb Mortal Wkly Rep 2017;66:933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics–2017 update: a report from the American Heart Association. Circulation 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sacco RL, Hauser WA, Mohr JP, Foulkes MA. One-year outcome after cerebral infarction in whites, blacks, and Hispanics. Stroke 1991;22:305–311. [DOI] [PubMed] [Google Scholar]
- 4.Andersen HE, Schultz-Larsen K, Kreiner S, Forchhammer BH, Eriksen K, Brown A. Can readmission after stroke be prevented? Results of a randomized clinical study: a postdischarge follow-up service for stroke survivors. Stroke 2000;31:1038–1045. [DOI] [PubMed] [Google Scholar]
- 5.Sacco RL. Risk factors, outcomes, and stroke subtypes for ischemic stroke. Neurology 1997;49:S39–S44. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP) [online]. Available at: cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed March 27, 2019. [Google Scholar]
- 7.Kind AJ, Smith MA, Liou JI, Pandhi N, Frytak JR, Finch MD. The price of bouncing back: one-year mortality and payments for acute stroke patients with 30-day bounce-backs. J Am Geriatr Soc 2008;56:999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin HJ, Chang WL, Tseng MC. Readmission after stroke in a hospital-based registry: risk, etiologies, and risk factors. Neurology 2011;76:438–443. [DOI] [PubMed] [Google Scholar]
- 9.Bambhroyliya ABDJ, Thomas EJ, Tyson JE, et al. Estimates and temporal trends for US nationwide 30-day hospital readmission among patients with ischemic and hemorrhagic stroke. JAMA Netw Open 2018;1:e181190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burke JF, Skolarus LE, Adelman EE, Reeves MJ, Brown DL. Influence of hospital-level practices on readmission after ischemic stroke. Neurology 2014;82:2196–2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fehnel CR, Lee Y, Wendell LC, Thompson BB, Potter NS, Mor V. Post-acute care data for predicting readmission after ischemic stroke: a nationwide cohort analysis using the minimum data set. J Am Heart Assoc 2015;4:e002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhattacharya P, Khanal D, Madhavan R, Chaturvedi S. Why do ischemic stroke and transient ischemic attack patients get readmitted? J Neurol Sci 2011;307:50–54. [DOI] [PubMed] [Google Scholar]
- 13.Lichtman JH, Leifheit-Limson EC, Jones SB, et al. Predictors of hospital readmission after stroke: a systematic review. Stroke 2010;41:2525–2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51:549–555. [DOI] [PubMed] [Google Scholar]
- 15.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med 2004;141:533–536. [DOI] [PubMed] [Google Scholar]
- 16.Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016;47:e98–e169. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA 2010;303:1716–1722. [DOI] [PubMed] [Google Scholar]
- 18.Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med 2010;5:392–397. [DOI] [PubMed] [Google Scholar]
- 19.Brooke BS, Stone DH, Cronenwett JL, et al. Early primary care provider follow-up and readmission after high-risk surgery. JAMA Surg 2014;149:821–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Terman SW, Reeves MJ, Skolarus LE, Burke JF. Association between early outpatient visits and readmissions after ischemic stroke. Circ Cardiovasc Qual Outcomes 2018;11:e004024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.QuintilesIMS. Pharmetrics Health Plan Claims Data User Guide & Data Dictionary. Plymouth Landing: IMS Health; 2014. [Google Scholar]
- 22.Dilokthornsakul P, Valuck RJ, Nair KV, Corboy JR, Allen RR, Campbell JD. Multiple sclerosis prevalence in the United States commercially insured population. Neurology 2016;86:1014–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kalilani L, Faught E, Kim H, et al. Assessment and effect of a gap between new-onset epilepsy diagnosis and treatment in the US. Neurology 2019;92:e2197–e2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Culbertson VL, Rahman SE, Bosen GC, Caylor ML, Xu D. Use of a bioinformatics-based toxicity scoring system to assess serotonin burden and predict population-level adverse drug events from concomitant serotonergic drug therapy. Pharmacotherapy 2019;39:171–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simpson AN, Wilmskoetter J, Hong I, et al. Stroke Administrative Severity Index: using administrative data for 30-day poststroke outcomes prediction. J Comp Eff Res 2018;7:293–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson Comorbidity Index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676–682. [DOI] [PubMed] [Google Scholar]
- 27.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson Comorbidity Index predicted in-hospital mortality. J Clin Epidemiol 2004;57:1288–1294. [DOI] [PubMed] [Google Scholar]
- 28.Post-stroke antihypertensive treatment study: a preliminary result. Chin Med J 1995;108:710–717. [PubMed] [Google Scholar]
- 29.PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 2001;358:1033–1041. [DOI] [PubMed] [Google Scholar]
- 30.Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke 2003;34:2741–2748. [DOI] [PubMed] [Google Scholar]
- 31.Johnston SC, Easton JD, Farrant M, et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med 2018;379:215–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nahab F, Takesaka J, Mailyan E, et al. Avoidable 30-day readmissions among patients with stroke and other cerebrovascular disease. Neurohospitalist 2012;2:7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crispo JAG, Thibault DP, Fortin Y, Krewski D, Willis AW. Association between medication-related adverse events and non-elective readmission in acute ischemic stroke. BMC Neurol 2018;18:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Condon C, Lycan S, Duncan P, Bushnell C. Reducing readmissions after stroke with a structured nurse practitioner/registered nurse transitional stroke program. Stroke 2016;47:1599–1604. [DOI] [PubMed] [Google Scholar]
- 35.Vahidy FS, Donnelly JP, McCullough LD, et al. Nationwide estimates of 30-day readmission in patients with ischemic stroke. Stroke 2017;48:1386–1388. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author on reasonable request.