To the editor:
During COVID-19 pandemic, health care systems have suffered a tremendous impact, due to the huge number of patients needing hospitalization. This has led to more restrictive indications for invasive procedures and to defer elective procedures [1], contributing to a reduction on the activity at catheterization laboratories.
More striking is the ≈40% reduction in the number of patients with ST-segment elevation myocardial infarction (STEMI) [2,3]. This is surprising because the incidence of cardiovascular events usually increases with respiratory infections [4]. Potential explanations may include reduction of STEMI due to physical inactivity, reluctance of patients for seeking medical assistance due to the possibility of SARS-CoV-2 contamination, attribution of symptoms to COVID-19 infection, health system failures and diagnostic errors in attending patients with chest pain, delay in diagnosis losing the benefit of early coronary reperfusion, increased use of thrombolysis, and cardiac death before medical attendance.
Among patients with STEMI, women and elderly are associated with longer delay of accessing medical care [5], and reduction of STEMI patients during COVID-19 pandemic could affect mainly to women and older patients.
In the region of Madrid (Spain, 6.7 million inhabitants), STEMI care is organized in a network including 11 hospitals with percutaneous coronary intervention facilities 24 h a day, 365 days per year. During COVID-19 pandemic, reperfusion protocols were not changed, and all except one (whose activity was absorbed by the closest hospitals) STEMI centers maintained their capability to attend patients with STEMI.
On March the 11st 2020, World Health Organization considered COVID-19 as a pandemic. We studied the influence of this pandemic on the number of STEMI patients attended at the STEMI centers, and particularly the influence of age and gender on the potential changes. We compared the number patients attended by the STEMI network during pandemic (40 days, from 12 March to 20 April 2020), with the weeks before the pandemic (40 days, from 1 February to 11 March 2020).
During both periods (80 days), 313 patients with STEMI were attended, 68 (21.7%) of them being women, and 245 (78.3%) men; mean age was 64.2 ± 13.2, and 109 (34.8%) were over 70.
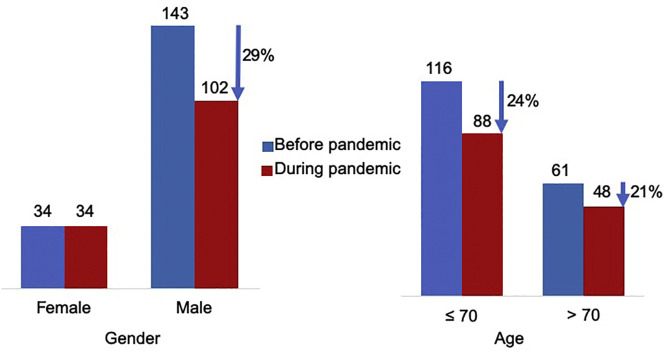
During pandemic, the number of patients was reduced in 23.2% (from 177 to 136). This reduction, however, took place only in male gender patients: from 143 to 102 (28.7% reduction), whereas the number of women was exactly the same in both periods (34).
The reduction in the number of STEMI patients was similar in patients ≤ 70 vs >70: 24.1% (from 116 to 88) and 21.3% (from 61 to 48) reduction, respectively (Fig. 1 ). Mean age was not statistically different in both periods (63.4 ± 13.4 before, and 65.1 ± 13.1 during pandemic, p = 0.3769).
Fig. 1.
Influence of age and gender on arrival of STEMI patients to tertiary centers in Madrid, Spain, during COVID-19 pandemic.
Therefore, the reduction in the number of patients with STEMI attended in tertiary hospitals only was found in men. Male gender is associated with higher mortality rates among patients with COVID-19 disease, and this could partially explain that men are more reluctant to ask for medical assistance in presence of chest pain. Also, coexistence with COVID-19 symptoms might have been more frequent among men, thus making more difficult the correct attribution of symptoms to heart attack. Additionally, lack of physical activity could have reduced STEMI more clearly in men. Finally, men have higher treatment-seeking threshold than women, some studies having pointed towards men's sense of stoicism and self-reliance. Because of these reasons, COVID-19 pandemic might have impacted clearly on STEMI treatment only in male patients, and counterbalanced the classical advantage of more typical symptoms in male gender. Age was not associated with the reduction on STEMI patients. That suggests that, although COVID-19 pandemic is mainly impacting on the elderly, the reduction of STEMI patients could be related more on patient decisions than on medical reasons and health care deficiencies.
Several public campaigns have been driven to encourage patients with chest pain to ask for medical advice during COVID-19 pandemic. Our findings could be of help in the design these campaigns and for similar pandemic we could suffer in the future.
References
- 1.Romaguera R., Cruz-Gonzalez I., Jurado-Roman A., et al. Considerations on the invasive management of ischemic and structural heart disease during the COVID-19 coronavirus outbreak. Consensus statement of the Interventional Cardiology Association and the Ischemic Heart Disease and Acute Cardiac Care Association of the Spanish Society of Cardiology. REC Interv Cardiol. 2020;2:112–117. [Google Scholar]
- 2.Rodríguez-Leor O., Cid-Álvarez B., Ojeda S., et al. Impact of COVID-19 pandemic over activity of interventional cardiology in Spain. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 3.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Musher D.M., Abers M.S., Corrales-Medina V.F. Acute infection and myocardial infarction. N Engl J Med. 2019;380:171–176. doi: 10.1056/NEJMra1808137. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen H.L., Saczynski J.S., Gore J.M., Goldberg R.J. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2010;3:82–92. doi: 10.1161/CIRCOUTCOMES.109.884361. [DOI] [PMC free article] [PubMed] [Google Scholar]