Abstract
Objective
The goal of this survey was to determine factors associated with anxiety/depression among neurosurgeons during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
An online survey was performed of neurosurgeons worldwide, conducted over 3 weeks. Depression in neurosurgeons was assessed by Self-Reporting Questionnaire–20.
Results
A total of 375 responses were received from 52 countries. Among all neurosurgeons, 34% felt tense, 32.5% were unhappy, 25% experienced insomnia, almost 20% had headaches, and 5% had suicidal ideation during the pandemic. Of participants, 14% had a score on Self-Reporting Questionnaire–20 consistent with depression. The likelihood of depression was significantly higher among those who did not receive guidance about self-protection from their institutions (odds ratio [OR], 2.47), those who did not feel safe with provided personal protective equipments (OR, 3.13), and those whose families considered their workplace unsafe (OR, 2.29). Depression was less likely in neurosurgeons who had minor concerns, compared with those with significant health concerns for their families (OR, 0.36). In multivariate analysis after controlling for effects of other covariates, odds of depression were significantly higher among neurosurgeons who did not feel safe with the provided personal protective equipment (OR, 2.43) and who were exposed to a COVID-19–positive colleague (OR, 2.54). Participants who had moderate concerns for their families had lesser odds of anxiety/depression than did those with significant concerns (OR, 0.28).
Conclusions
Based on the modifiable risk factors of depression in this study, it is recommended that the safety of neurosurgeons be ensured by providing appropriate safety measures for them to regain their confidence and hence reduce the incidence of depression.
Key words: COVID-19, Depression/anxiety, Depression in neurosurgeons, Depression in surgeons, Depression scale, Global neurosurgery, Health care workers, Pandemic, PPE, Safety, Social media
Abbreviations and Acronyms: CI, Confidence interval; COVID-19, Coronavirus disease 2019; OR, Odds ratio; PPE, Personal protective equipment; SRQ-20, Self-Reporting Questionnaire–20; WHO, World Health Organization; WSCS, World Spinal Column Society
Introduction
The novel coronavirus initially originated in China and has rapidly spread globally. The increasing pandemic of severe acute respiratory syndrome coronavirus 2 diseases (coronavirus disease 2019 [COVID-19]) has become a significant public health liability worldwide. The COVID-19 pandemic has become one of the central health crises of a generation. It has affected people irrespective of nation, race, caste, and socioeconomic groups. On January 30, 2020, the World Health Organization (WHO) announced the emergence of the novel coronavirus. It declared a PHEIC (Public Health Emergency of International Concern), which is the sixth PHEIC under the International Health Regulations. The rapid increase in cases and evolving guidelines regarding protection and prevention of the spread of pandemic, with no confirmed treatment or approved vaccine, have caused apprehension and anxiety among health care workers. Unpredictability in the biological behavior of the virus, erratic changing instructions from WHO, and variable guidelines regarding quarantine and management of the pandemic have increased the uncertainty.
As of the first week of May 2020, 2,227,191 COVID-positive patients with 258,356 confirmed deaths had been reported worldwide and 212 countries were affected by the pandemic.1 More than 42,600 health care providers have been infected with COVID-19 in China, and more than 124 doctors have died in Italy.2 , 3 In the United States, approximately 9300 nurses, doctors, and other frontline health care workers have been infected by the disease, and dozens have died.4 Across Western Europe, nearly 14% of patients with confirmed coronavirus are medical professionals, which is the highest number of cases reported among doctors and nurses.5 Moreover according to the report on April 3, 2020, at least 35 doctors have died, and more than 4200 health workers have self-isolated in countries across the Asia and Pacific region, Therefore, concerns among health care professionals are well founded.6 The pandemic is serious and disruptive,7 yet, despite its widespread infectivity and higher mortality than the common influenza virus, little is known regarding management of critical cases, prevention, and optimal measures to reduce its spread. Scarce resources and an often inadequate availability of personal protective equipment (PPE) and lack of knowledge about their optimal use can further lead to apprehension, distress, panic, and anxiety in health care workers.8 The COVID-associated health crisis has disrupted working of all medical communities worldwide, including delivery of essential medical and neurosurgical services. The rapidly increasing number of COVID-positive patients not only presents a public health challenge but also has significant medical and ethical implications for the care of neurosurgical patients. There is a paucity of literature guiding neurosurgery practice. Neurosurgical societies have developed and reported guidelines to promote best practices for their patients. However, implementation of these guidelines is a challenge in many parts of the world where health care systems are not well established, but adjustments during an event such as the COVID-19 pandemic have been made. The crisis may provoke even more distress and depression within the neurosurgical fraternity.9
Objective
A survey was developed to assess the stressors affecting neurosurgeons as a result of the pandemic. The goal of this survey was to determine the prevalence and factors associated with anxiety and depression among neurosurgeons during the COVID-19 pandemic.
Although the full impact of the pandemic remains to be seen, this survey aimed to determine the frequency of depression among neurosurgeons during the pandemic and explore any modifiable factors that could be addressed to reduce the incidence of distress and mental illness among neurosurgeons.
Methods
Study Design
This was a cross-sectional study design conducted through an anonymous online questionnaire with information only about the city and no contact information to address ethical implications of the survey. The study duration was 3 weeks (until the requisite sample size was achieved). The questionnaire was modified based on suggestions from World Spinal Column Society (WSCS) executive board members. Most members of the WSCS are neurosurgeons, who also perform spinal surgery. The survey was designed on Google Forms and sent to neurosurgeons who were members of scientific societies globally through the WSCS Executive Committee. The survey was circulated to members of WSCS on their social media, WhatsApp groups, and e-mails and through a snowballing technique locally and internationally. The neurosurgeons identified through these media were asked to forward the survey to other neurosurgeons in their professional circle and so on. Of 800 neurosurgeons who were approached, 375 responded. A recent Chinese study9 showed a 40.77% (201/493) prevalence of mild to moderate depression among physicians during the COVID pandemic.
Depression was assessed through a WHO validated questionnaire (Self-Reporting Questionnaire–20 [SRQ-20]).10 A cutoff score ≥8 was considered as positive for depression.
Study Variables
The dependent variable was depression graded on WHO SRQ -20 with a cutoff score ≥8 for a positive case of anxiety/depression.
Independent variables were age (years), country, continent, consultant/resident self-rating of COVID-19 knowledge, level of practice, experience, size of the department, number of consultants/staff, number of trainees, level of awareness regarding self-protection provided by current workplace, provision of adequate PPE at the workplace, training courses conducted for PPE use, safe practice with the provided PPE by institution, presence of COVID-positive colleagues, redeployment to COVID-affected area, perception about redeployment, concerns regarding the health of the family, and perception of the family regarding work place safety.
Data Analysis
All study variables were categorical including age, designation, departmental size, number of trainees, self-rating of knowledge, feeling safe with provided PPE, family concerns, deployment in different areas, perception of family about workplace safety, enough knowledge to deal if deployed, presence of COVID-positive colleagues, and SRQ-20 questions expressed as frequencies and percentages. A χ2 test was applied to compare study variables among depressed and nondepressed individuals. A McNemar test was applied to see the difference in proportions of neurosurgeons performing elective surgeries before and after the COVID-19 pandemic.
Univariate binary logistic regression was applied to determine association of each independent variable with the outcome (anxiety/depression). Multivariate logistic regression was used to measure the association of multiple independent variables with the outcome (anxiety/depression) by computing adjusted odds ratios (ORs) and their 95% confidence intervals (CIs). Variables with a P value <0.25 in univariate analysis were subsequently included in the multivariate logistic regression model. Statistical significance was assumed for P < 0.05 in the multivariate model.
Ethical Consideration
Consent was obtained from all those who filled the online questionnaire. The participant’s identity and name of the institution were not disclosed. All data were kept confidential in a password-protected computer. There was no financial compensation for participation or any penalty for not participating.
Results
Sociodemographic Distribution of Participants
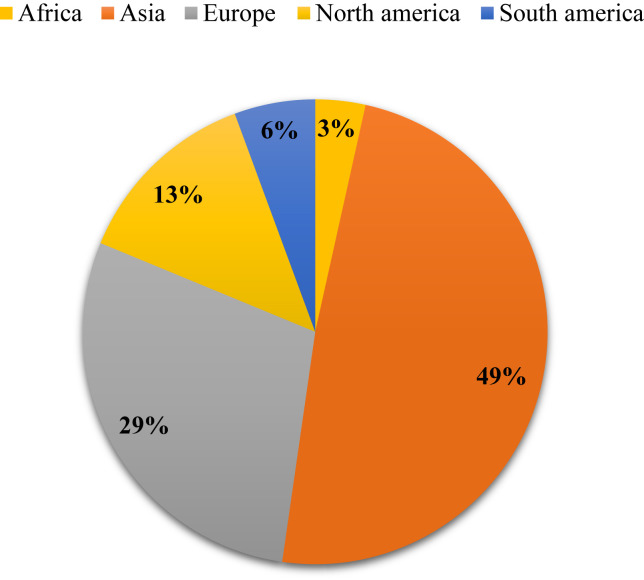
A total of 375 neurosurgery trainees and consultants from 52 countries and 5 continents participated in the survey (Figure 1 ). Most respondents were from Asia (n = 181, 48.5%) (Figure 1). Table 1 shows the distribution of sociodemographic factors among participants. Most participants were consultants (79%) from low to middle-income countries (66%). More than half were younger than 40 years. Among all participants, 84% worked in departments with ≥4 staff (83%), and more than half of the respondents reported having <10 trainees in their departments (53.3%).
Figure 1.
Responses by continent.
Table 1.
Responses Distribution and Participants Characteristics
| Variables | Groups | Frequency | % |
|---|---|---|---|
| Age | <40 years | 202 | 55.0 |
| ≥40 years | 165 | 45.0 | |
| Missing | 8 | 2.1 | |
| Designation | Resident | 77 | 20.7 |
| Consultant | 295 | 79.3 | |
| Number of staff/consultants in department | <4 | 58 | 15.5 |
| ≥4 | 314 | 83.7 | |
| Missing | 3 | 0.8 | |
| Number of trainees | <10 | 200 | 53.3 |
| ≥10 | 172 | 45.9 | |
| Missing | 3 | 0.8 | |
| Practice area | Both private and government | 87 | 24.3 |
| Private setup | 60 | 16.8 | |
| University hospital | 143 | 39.9 | |
| Government | 68 | 19.0 | |
| Missing | 17 | 4.5 | |
| Self-rating of knowledge about COVID-19 | Basic | 116 | 30.9 |
| Moderate | 209 | 55.7 | |
| Extensive | 50 | 13.3 | |
| Is your hospital providing enough information and guidance for your protection? | No | 119 | 31.7 |
| Yes | 256 | 68.3 | |
| Provision of PPE by hospital | No | 117 | 31.2 |
| Yes | 258 | 68.8 | |
| Did you get training (courses)? | No | 171 | 45.6 |
| Yes | 204 | 54.4 | |
| Do you feel safe to practice with the provided PPE by your hospital? | No | 171 | 45.6 |
| Yes | 204 | 54.4 | |
| Do you have concerns regarding the health of your family? | Minor | 40 | 10.7 |
| Moderate | 64 | 17.1 | |
| Major | 271 | 72.3 | |
| Do you have colleagues in your department that are COVID-19 positive? | No | 295 | 78.7 |
| Yes | 80 | 21.3 | |
| When exposed, what was the action taken? | Self-isolation | 46 | 57.5 |
| Quarantine | 22 | 27.5 | |
| Admitted | 7 | 8.8 | |
| Continue work | 4 | 5.0 | |
| No action | 1 | 1.3 | |
| What is your biggest concern(s) regarding the COVID-19 and your safe practice? | Lack of enough information | 48 | 12.8 |
| Lack of adequate organization at your workplace | 79 | 21.1 | |
| Lack of adequate PPE | 156 | 41.6 | |
| Lack of adequate training for PPE usage | 56 | 14.9 | |
| Other | 36 | 9.6 | |
| Average no. of surgeries/week in your department before COVID-19 | ≤10 | 47 | 12.5 |
| >10 | 328 | 87.5 | |
| Average no. of surgeries/week in your department after COVID-19 | ≤10 | 317 | 84.5 |
| >10 | 58 | 15.5 | |
| Elective surgeries before COVID-19 | <75% elective surgeries (NO) | 39 | 10.4 |
| ≥75% elective surgeries (YES) | 336 | 89.6 | |
| Elective surgeries after COVID-19 | <25% elective surgeries (YES) | 303 | 80.8 |
| ≥25% elective surgeries (NO) | 72 | 19.2 | |
| Does your family feel safe for you to go to work? | No | 251 | 66.9 |
| Yes | 124 | 33.1 | |
| Have you been asked a redeployment to COVID-19 affected area? | No | 270 | 72.0 |
| Yes | 105 | 28.0 | |
| Do you think your knowledge and expertise would be useful and your work meaningful if you are redeployed out of your specialty? | No | 223 | 59.5 |
| Yes | 152 | 40.5 | |
| In your opinion, when will this pandemic end? | Within 2 months | 64 | 17.1 |
| >2 months or not sure | 311 | 82.9 | |
| Depression score in categories | <8 | 323 | 86.1 |
| ≥8 | 52 | 13.9 |
PPE, personal protective equipment.
Responses Regarding COVID-19 Pandemic
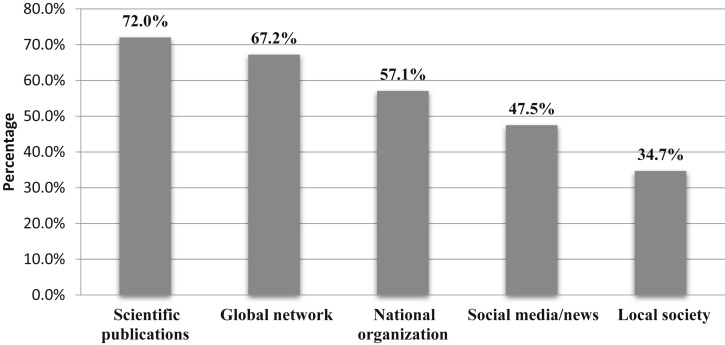
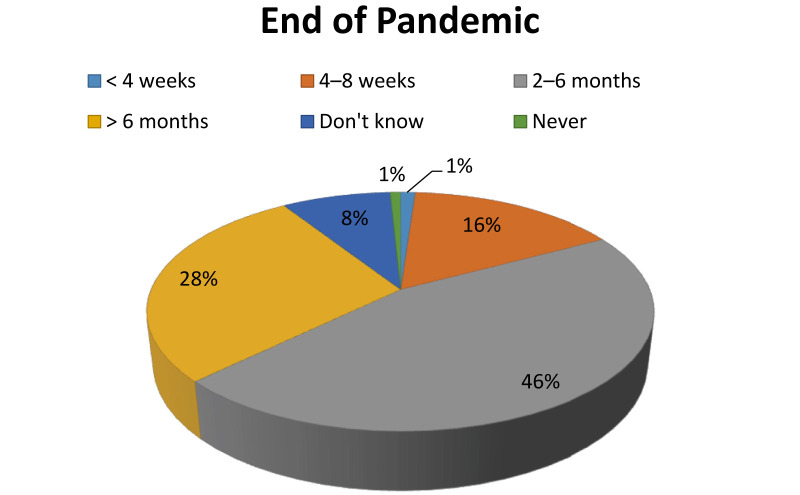
Table 2 shows the distribution of responses regarding the COVID-19 pandemic. Almost 69% reported basic to moderate knowledge about the pandemic. Sources of information are shown in Figure 2 . The most common source of information was scientific publications, and almost half also used social media as a source for information. Most of the participants (74%) believed that it would take more than 2 months for the pandemic to end (Figure 3 ).
Table 2.
Comparison of Participants' Characteristics and Perception Among Depression Groups
| Depressed Frequency (%) | Nondepressed Frequency (%) | Total Frequency (%) | P Value | |
|---|---|---|---|---|
| Age | ||||
| <40 years | 33 (16.3) | 169 (83.7) | 202 (100) | 0.188 |
| ≥40 years | 19 (11.5) | 146 (88.5) | 165 (100) | |
| Socioeconomic status of countries | ||||
| Middle/low | 35 (14.2) | 211 (85.8) | 246 (100) | 0.664 |
| High income | 16 (12.6) | 111 (87.4) | 127 (100) | |
| Continents | ||||
| Africa | 2 (15.4) | 11 (84.6) | 13 (100) | 0.679 |
| Asia | 27 (14.8) | 155 (85.2) | 182 (100) | |
| Europe | 11 (10.2) | 97 (89.8) | 108 (100) | |
| North America | 7 (14.3) | 42 (85.7) | 49 (100) | |
| South America | 4 (19) | 17 (81) | 21 (100) | |
| Designation | ||||
| Trainee | 10 (13) | 67 (87) | 77 (100) | 0.778 |
| Consultant | 42 (14.2) | 253 (85.8) | 295 (100) | |
| Department size | ||||
| <40 beds | 16 (12) | 117 (88) | 133 (100) | 0.446 |
| >40 beds | 36 (14.9) | 206 (85.1) | 242 (100) | |
| Number of staff/consultants in the department | ||||
| <4 | 8 (13.8) | 50 (86.2) | 58 (100) | 0.965 |
| ≥4 | 44 (14) | 270 (86) | 314 (100) | |
| Number of trainees | ||||
| <10 | 30 (15) | 170 (85) | 200 (100) | 0.540 |
| ≥10 | 22 (12.8) | 150 (87.2) | 172 (100) | |
| Area of practice | ||||
| Combined | 15 (17.2) | 72 (82.8) | 87 (100) | 0.594 |
| Private | 6 (10) | 54 (90) | 60 (100) | |
| University hospital | 21 (14.7) | 122 (85.3) | 143 (100) | |
| Government | 8 (11.8) | 60 (88.2) | 68 (100) | |
| Rating of self-knowledge | ||||
| Basic | 20 (17.2) | 96 (82.8) | 116 (100) | 0.206 |
| Moderate/extensive | 32 (12.4) | 227 (87.6) | 259 (100) | |
| Is your hospital providing enough information and guidance for your protection? | ||||
| No | 26 (21.8) | 93 (78.2) | 119 (100) | ∗0.002 |
| Yes | 26 (10.2) | 230 (89.8) | 256 (100) | |
| Are you provided with PPE by your hospital? | ||||
| No | 19 (16.2) | 98 (83.8) | 117 (100) | 0.371 |
| Yes | 33 (12.8) | 225 (87.2) | 258 (100) | |
| Did you get training (courses)? | ||||
| No | 25 (14.6) | 146 (85.4) | 171 (100) | 0.699 |
| Yes | 27 (13.2) | 177 (86.8) | 204 (100) | |
| Do you feel safe to practice with the provided PPE by your hospital? | ||||
| No | 36 (21.1) | 135 (78.9) | 171 (100) | ∗<0.001 |
| Yes | 16 (7.8) | 188 (92.2) | 204 (100) | |
| Concerns regarding the health of your family | ||||
| Minor | 4 (10.0) | 36 (90.0) | 40 (100) | ∗0.035 |
| Moderate | 3 (4.7) | 61 (95.3) | 64 (100) | |
| Major | 45 (16.6) | 226 (83.4) | 271 (100) | |
| Do you have colleagues in your department that are COVID-19 positive? | ||||
| No | 36 (12.2) | 259 (87.8) | 295 (100) | 0.074 |
| Yes | 16 (20) | 64 (80) | 80 (100) | |
| Average no. of surgeries/week in your department before COVID-19 | ||||
| ≤10 | 6 (12.8) | 41 (87.2) | 47 (100) | 0.815 |
| >10 | 46 (14.0) | 282 (86.0) | 328 (100) | |
| Average no. of surgeries/week in your department after COVID-19 | ||||
| ≤10 | 41 (12.9) | 276 (87.1) | 317 (100) | 0.222 |
| >10 | 11 (19.0) | 47 (81.0) | 58 (100) | |
| Elective surgeries before COVID-19 | ||||
| <75% elective surgeries | 5 (12.8) | 34 (87.2) | 39 (100) | 0.842 |
| >75% elective surgeries | 47 (14) | 289 (86) | 336 (100) | |
| Elective surgeries after COVID-19 | ||||
| <25% elective surgeries | 39 (12.9) | 264 (87.1) | 303 (100) | 0.253 |
| >25% elective surgeries | 13 (18.1) | 59 (81.9) | 72 (100) | |
| Does your family feel safe for you to go to work? | ||||
| No | 42 (16.7) | 209 (83.3) | 251 (100) | ∗0.022 |
| Yes | 10 (8.1) | 114 (91.9) | 124 (100) | |
| Have you been asked redeployment to COVID-19 affected area? | ||||
| No | 37 (13.7) | 233 (86.3) | 270 (100) | 0.884 |
| Yes | 15 (14.3) | 90 (85.7) | 105 (100) | |
| Do you think your knowledge and expertise would be useful and your work meaningful if you are redeployed out of your specialty? | ||||
| No | 32 (14.3) | 191 (85.7) | 223 (100) | 0.743 |
| Yes | 20 (13.2) | 132 (86.8) | 152 (100) | |
| Opinion regarding the end of the pandemic | ||||
| <2 months | 5 (7.8) | 59 (92.2) | 64 (100) | 0.124 |
| >2 months or not sure | 47 (15.1) | 264 (84.9) | 311 (100) | |
PPE, personal protective equipment.
Significant at P < 0.05.
Figure 2.
Frequency of sources of knowledge for COVID-19 among neurosurgeons.
Figure 3.
Speculations about end of this pandemic, in the opinion of neurosurgeons.
Most participants (68%) said that enough information had been provided by their institutions regarding the COVID pandemic. Of respondents, 31% reported that they had not been provided with PPE by their hospital, although more than half had attended training courses arranged by their institutions. Among consultants and trainees, 45.6% reported that they did not feel safe during the pandemic. Most (72%) had severe concerns regarding the safety of their families at home. Of respondents, 21% reported that they had been exposed to a COVID-positive colleague. Of these respondents, 85% had been quarantined or self-isolated themselves and 8.8% were admitted for quarantine. Surprisingly, 5% continued work, whereas 1.3% took no action at all on being exposed. Of the respondents, 41.6% reported that their primary concern during this pandemic was the inadequate provision of PPE.
Most (n = 328; 87.5%) of the neurosurgeons said that as a routine, their weekly surgery volumes were >10 cases. In comparison, during the pandemic, 270 (72%) said that they were performing <10 surgeries/week (P < 0.001). Similarly, most (n = 336, 89.6%) reported performing >75% elective surgeries before the pandemic, whereas 272 (72.5%) said that the number of elective surgeries during the COVID-19 pandemic had reduced to 25% or less (P < 0.001).
Families of 67% of neurosurgeons did not feel it was safe for them to go to work. About a quarter (28%) of the participants were redeployed to a COVID-affected area for work during the pandemic, and most (60%) believed that redeployment would not be useful considering their knowledge and expertise.
Depression and Anxiety Among Participants and the Distribution of Factors
A 13.9% prevalence of anxiety/depression was found among neurosurgery trainees and consultants in this study. Among all participants, 34% felt tense; 32.5% were unhappy; 25% experienced insomnia; almost 20% had headaches, were easily fatigued or tired, and believed that they were unable to play a useful part in their life; 10% had difficulty in decision making, 5% cried more than usual; and 5% had suicidal ideation during the pandemic (Table 3 ).
Table 3.
Distribution of Different Symptoms Among Participants During the COVID Pandemic
| Self-Reporting Questionnaire-20 Items | Responses | Frequency | % |
|---|---|---|---|
| Often have headaches? | No | 300 | 80.0 |
| Yes | 75 | 20.0 | |
| Is your appetite poor? | No | 349 | 93.1 |
| Yes | 26 | 6.9 | |
| Do you sleep badly? | No | 282 | 75.2 |
| Yes | 93 | 24.8 | |
| Do your hands shake? | No | 352 | 93.9 |
| Yes | 23 | 6.1 | |
| Are you easily fatigued? | No | 303 | 80.8 |
| Yes | 72 | 19.2 | |
| Do you feel nervous, tense, or worried? | No | 248 | 66.1 |
| Yes | 127 | 33.9 | |
| Is your digestion poor? | No | 340 | 90.7 |
| Yes | 35 | 9.3 | |
| Do you have trouble thinking clearly? | No | 335 | 89.3 |
| Yes | 40 | 10.7 | |
| Do you feel unhappy? | No | 253 | 67.5 |
| Yes | 122 | 32.5 | |
| Do you cry more than usual? | No | 356 | 94.9 |
| Yes | 19 | 5.1 | |
| Difficult to enjoy daily activities? | No | 258 | 68.8 |
| Yes | 117 | 31.2 | |
| Difficulty in decision making? | No | 341 | 90.9 |
| Yes | 34 | 9.1 | |
| Is your daily work suffering? | No | 254 | 67.7 |
| Yes | 121 | 32.3 | |
| Are you unable to play a useful part in life? | No | 296 | 78.9 |
| Yes | 79 | 21.1 | |
| Have you lost interest in things? | No | 316 | 84.3 |
| Yes | 59 | 15.7 | |
| Do you feel you are a worthless person? | No | 353 | 94.1 |
| Yes | 22 | 5.9 | |
| Has the thought of ending your life been on your mind? | No | 356 | 94.9 |
| Yes | 19 | 5.1 | |
| Do you have uncomfortable feeling in the stomach? | No | 323 | 86.1 |
| Yes | 52 | 13.9 | |
| Do you feel tired all the time? | No | 322 | 85.9 |
| Yes | 53 | 14.1 | |
| Are you easily tired? | No | 298 | 79.5 |
| Yes | 77 | 20.5 |
Table 4 shows the univariate and multivariate analysis for the association of different factors with anxiety and depression among neurosurgical trainees and consultants. The likelihood of depression was higher among those who did not receive information or self-protection from their institutions to combat the situation than in those who received it (OR, 2.47; 95% CI, 1.37–4.48). Those who reported that they did not feel safe with provided PPE were also at a higher risk of depression (OR, 3.13; 95% CI, 1.67–5.88). Anxiety and depression were less likely among those who had minor (n = 4; 10%) and moderate concerns (n = 3; 4.7%) for the health of their families compared with participants who were more concerned for their families during the current pandemic situation (n = 45; 16.6%). Univariate ORs showed that the likelihood of depression was significantly lower in neurosurgeons who had minor concerns compared with those with significant health concerns for their families (OR, 0.36; 95% CI, 0.16–0.83). The prevalence of depression was also significantly higher in participants whose families considered their workplace unsafe (OR, 2.29; 95% CI, 1.11–4.73).
Table 4.
Univariate and Multivariate Analysis for Crude and Adjusted Odds Ratios for Depression
| Univariate |
Multivariate |
|||
|---|---|---|---|---|
| OR (95% CI) | P Value | Adjusted OR (95% CI) | P Value | |
| Age | ||||
| <40 years | 1.50 (0.82–2.75) | 0.190 | 1.23 (0.63–2.41) | 0.543 |
| ≥40 years | Reference | Reference | ||
| Rating of self-knowledge | ||||
| Basic | 1.48 (0.81–2.71) | 0.208 | 1.48 (0.78–2.84) | 0.232 |
| Moderate/extensive | Reference | Reference | ||
| Is your hospital providing enough information and guidance for your protection? | ||||
| No | 2.47 (1.37–4.48) | ∗0.003 | 1.44 (0.71–2.92) | 0.314 |
| Yes | Reference | Reference | ||
| Do you feel safe to practice with the provided PPE by your hospital? | ||||
| No | 3.13 (1.67–5.88) | ∗<0.001 | 2.43 (1.13–5.22) | ∗0.023 |
| Yes | Reference | Reference | ||
| Concerns regarding the health of family | ||||
| Minor | 0.56 (0.19–1.65) | 0.290 | 0.83 (0.25–2.76) | 0.764 |
| Moderate | 0.25 (0.07–0.82) | ∗0.023 | 0.28 (0.08–0.99) | ∗0.048 |
| Major | Reference | Reference | ||
| Do you have colleagues in your department that are COVID positive? | ||||
| No | Reference | Reference | ||
| Yes | 1.80 (0.94–3.44) | 0.076 | 2.54 (1.24–5.19) | ∗0.011 |
| Does your family feel safe for you to go to work? | ||||
| No | 2.29 (1.11–4.73) | ∗0.025 | 1.27 (0.54–2.98) | 0.588 |
| Yes | Reference | — | — | |
OR, odds ratio; CI, confidence interval; PPE, personal protective equipment.
Significant at P < 0.05.
In multivariate analysis (Table 4), effects of the following variables were controlled; age, self-rating of COVID-19 knowledge, information regarding protection provided by hospital, feeling safe with provided protective equipment, degree of concern for family health, presence of COVID-19–positive colleagues, and families considering the workplace safe. After controlling for the effects of other covariates, the odds of depression were significantly higher in individuals who did not feel safe with the PPE provided to them than in those who were satisfied with provided PPE (OR, 2.43; 95% CI, 1.13–5.22). Participants who had moderate concerns for their families had lesser odds of anxiety and depression than did those with significant concerns (OR, 0.28; 95% CI, 0.08–0.99). Being exposed to a COVID-19–positive colleague significantly increased the likelihood of anxiety/depression, even after adjusting for other covariates (OR, 2.54; 95% CI, 1.24–5.19).
Discussion
The COVID-19 pandemic is spreading across the globe at an exponential rate, creating apprehension and distress among all health care professionals.8 Neurosurgeons, who are an essential part of the health care community, are also affected in a major way. Belonging to a fundamental surgical specialty, tackling emergencies and performing complex operations requiring significant dexterity, hypothetically enables them to deal with stressful situations, making them less prone to develop anxiety and depression.11 This may only be an assumption because we did not find any study to determine the frequency of anxiety/depression among this specialty before the pandemic. This is the first time that depression has been found among 14% of neurosurgeons. It cannot be said with conviction if this frequency is higher than that before the pandemic but a study performed in 2003 among surgeons12 showed an increase in prevalence of depression after the severe acute respiratory syndrome outbreak, with a 30% increase in suicide. Poor mental health is a social stigma13; moreover, a fear of being judged may explain why neurosurgeons have a lower depression score, as found in another study assessing level of stress among surgeons.11 This may be one of the reasons that despite mental health problems and psychosocial issues among health care workers, most do not often seek mental health care.14
Most participants were consultants (79%), and almost half were 40 years old and older. The senior neurosurgeons were less likely to be anxious and depressed, although the results were not statistically significant. In relation to this finding, a recent United Kingdom National Health Service survey also indicated that 70% of young physicians had mental health issues, whereas retired physicians and surgeons were more enthusiastic to volunteer for COVID duties.15 , 16
There was no difference in the frequency of depression among neurosurgeons working in private or government/university hospitals. Although a significant decrease in workload may be a potential risk factor leading to psychological distress, a nondifferential change between workload of private and public sector explains our finding, as confirmed by a recent survey by Jean.17
The COVID-19 pandemic has a global impact, irrespective of race, caste, color, or creed, with widespread xenophobia especially among the medical fraternity regarding their families’ and their own health (unpublished data). Despite trying times, this survey showed no difference in depression among the neurosurgeons, whether they belonged to high-income (12.6%) or middle-/lower-income countries (14.2%) or European (10.4%) or non-European (15%) countries. However, a recent Chinese study16 reported a higher prevalence of depression (50.4%), anxiety (44.6%), and insomnia (34%) among frontline health care workers. This finding shows that more than the income, specialty, or region, the area of practice influences mental health, predisposing to an increased sense of insecurity and hence psychological distress.
The requirement for quarantine, social distancing, and shelter-in-place orders has led to an abrupt change in lifestyles and may be causing increased apprehension among families, especially of health care workers. Not only families of neurosurgeons believed that it was unsafe for them to go to work, but the surgeons themselves reported concerns for the safety of their families at home. Therefore, a feeling of self-protection with provided PPE had a significant negative association with anxiety/depression whereas a COVID-positive colleague increased the likelihood of depression among neurosurgeons. A recent survey in United Kingdom reported that half of health workers had stress because of inadequate availability of PPE.15
This pandemic has disturbed functioning of all medical and surgical specialties. Selected emergency neurosurgery cases are being performed in special circumstances only such as trauma, severe acute functional impairment, and tumors causing impending disability. Neurosurgical approaches through the nose and sinuses are being postponed because of the high risk of viral transmission and updated neurosurgical guidelines for the treatment of COVID-positive patients or patients with suspected COVID have been circulated.8 The COVID crisis has hence led to a considerable decrease in elective cases (P < 0.001). Jean also reported a decrease of >50% operative volume during the present pandemic.17 Although our study did not find a significant association between this decrease in elective cases and anxiety/depression among neurosurgeons, if this status quo is further extended, it may lead to depression, because one third of our participants were unhappy, felt tensed, experienced insomnia and headaches, or and felt fatigued and tired. Moreover, 1 in 20 respondents cried more than usual and had suicidal ideation. This hypothesis is confirmed by another study conducted at Liaquat National Hospital on frontline physicians (unpublished data), which found that there was more depression in physicians who were working <20 hours a week compared with those who were working >20 hours during the pandemic.
Although the potential shortage of ventilators and intensive care unit beds necessary to care for the surge of critically ill patients has been well described, additional supplies and beds will not be helpful unless there is an adequate workforce. According to our data, about 28% of the participants were redeployed to a COVID-affected area during the pandemic. Nevertheless, 60% of neurosurgeons believed that their knowledge and expertise in an unknown environment would not be useful, and their work will not be meaningful if redeployed out of their specialty.
Limitations of the Study
To our knowledge, this is the first study to determine the frequency and factors associated with anxiety and depression among 375 neurosurgeons from 52 countries. The prevalence of depression and anxiety among neurosurgeons was found to be lower than the frequency reported among other frontline workers during the COVID pandemic. Yet, it is difficult to conclude the magnitude of the problem attributable to the pandemic, because there is a paucity of data regarding mental illness among neurosurgeons before the catastrophe. In a recent survey among neurosurgery residents, the risk of burnout was found to be 20.7% and higher working hours was one of the drivers for burnout, whereas another survey found a 56.7% burnout among neurosurgeons. Because both these surveys did not explore depression or anxiety, results of our study are not comparable, yet, because working hours during the pandemic have considerably reduced, it can be extrapolated that the frequency of burnout would be consequentially less.17 , 18
Mental illness is a social stigma worldwide, which may be more of an issue among fraternities who are considered resilient such as the neurosurgical specialty, hence leading to an underreporting of symptoms. Only 1 scale (SRQ-20) was used to screen for anxiety/depression, because asking too many questions on an online survey was inconvenient and would have led to missing data. Moreover, in online surveys, there is always a high probability of participation bias because the participants, based on their state of mind at the time of the study, may or may not choose to participate in the study. However, this situation may lead to nondifferential participation bias. With the evolving pandemic, the situation is still dynamic in various countries worldwide. Circumstances have varied from day to day, and hence, the response of participants may be different according to their changing situation. Therefore, the survey being completed readily by participants having more concerns regarding the ongoing pandemic may have introduced a bias. Although we tried to control for confounders during recruitment as well as during analysis through multivariate analysis, there is a possibility that we may have missed potential confounders, which may have exaggerated or masked the associations. Yet, the factors associated with anxiety/depression among neurosurgeons in the multivariate analysis are all biologically plausible.
Conclusions
The world is going through an unprecedented crisis, which has caused turmoil in all the countries worldwide. The health system has not dealt with such a disaster in decades. Neurosurgeons, like all other specialties, are affected and experiencing challenges in their work and daily living. Colleagues becoming infected, feelings of being unprotected, and concerns for the health of their families were factors found to be associated with anxiety/depression. We therefore recommend that the safety of health care workers is ensured by providing standard PPE and having optimum safety measures for them to regain confidence and hence reduce the incidence of mental ailments.
CRediT authorship contribution statement
Salman Sharif: Writing - original draft, Writing - review & editing. Faridah Amin: Writing - original draft, Writing - review & editing. Mehak Hafiz: Writing - original draft, Writing - review & editing. Edward Benzel: Conceptualization, Data curation, Writing - review & editing. Nikolay Peev: Conceptualization, Data curation, Writing - review & editing. Rully Hanafi Dahlan: Conceptualization, Data curation, Writing - review & editing. Yavor Enchev: Conceptualization, Data curation, Writing - review & editing. Paulo Pereira: Conceptualization, Data curation, Writing - review & editing. Sandeep Vaishya: Conceptualization, Data curation, Writing - review & editing.
Acknowledgments
We thank Ms. Noureen Durrani for statistical analysis of the data and Mr. Imad Ullah for helping throughout the study.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Mamoon N., Rasskin G. COVID-19. https://www.covidvisualizer.com/ Carnegie Mellon University. 2020. Available at: Accessed May 05,2020.
- 2.Zhan M., Qin Y., Xue X., Zhu S. Death from Covid-19 of 23 health care workers in China. N Engl J Med. 2020;382:2267–2268. doi: 10.1056/NEJMc2005696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nearly 17,000 Italian health workers infected with virus: Study. https://www.straitstimes.com/world/europe/nearly-17000-italian-health-workers-infected-with-virus-study Singapore: The Straits Times. 2020. Available at: Accessed May 05,2020.
- 4.At least 9,000 U.S. health care workers sickened with COVID-19, CDC data shows. https://www.npr.org/sections/health-shots/2020/04/15/834920016/at-least-9-000-u-s-health-care-workers-sickened-with-covid-19-cdc-data-shows Nashville public Radio. 2020. Available at: Accessed May 05,2020.
- 5.‘It’s like being a war medic.’ A Madrid doctor speaks out about grave shortages in protective gear. https://time.com/5813848/spain-coronavirus-outbreak-doctor Time USA. 2020. Available at: Accessed May 05,2020.
- 6.Asia-Pacific health workers risk all to fight COVID-19. https://www.aa.com.tr/en/asia-pacific/asia-pacific-health-workers-risk-all-to-fight-covid-19/1791014 Anadolu Agency. 2020. Available at: Accessed May 05,2020.
- 7.Misra A. Doctors and healthcare workers at frontline of COVID 19 epidemic: admiration, a pat on the back, and need for extreme caution. Diabetes Metab Syndr. 2020;14:255–256. doi: 10.1016/j.dsx.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guidelines of spine practice during COVID19 pandemic. http://www.wfns-spine.org/pdf/Covid%20-19%20WSCS%20-%20WFNS%20Spine%20guidelines.pdfa WFNS Spine Committee. 2020. Available at: Accessed May 05,2020.
- 10.Netsereab T.B., Kifle M.M., Tesfagiorgis R.B., Habteab S.G., Weldeabzgi Y.K., Tesfamariam O.Z. Validation of the WHO self-reporting questionnaire-20 (SRQ-20) item in primary health care settings in Eritrea. Int J Ment Health Syst. 2018;12:61. doi: 10.1186/s13033-018-0242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green A., Duthie H.L., Young H.L., Peters T.J. Stress in surgeons. Br J Surg. 1990;77:1154–1158. doi: 10.1002/bjs.1800771024. [DOI] [PubMed] [Google Scholar]
- 12.Narenthiran G. Internation Webinar Symposium from the Neurosurgery Research Listserv on ‘Impact of COVID-19 on Neurosurgery’. https://www.youtube.com/watch?v=NIDWcrqkMIU 2020. Available at: Accessed May 05,2020.
- 13.Jones N., Whybrow D., Coetzee R. UK military doctors; stigma, mental health and help-seeking: a comparative cohort study. J R Army Med Corps. 2018;164:259–266. doi: 10.1136/jramc-2018-000928. [DOI] [PubMed] [Google Scholar]
- 14.Zheng W. Mental health and a novel coronavirus (2019-nCoV) in China. J Affect Disord. 2020;269:201–202. doi: 10.1016/j.jad.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerada C. Clinical depression: surgeons and mental illness. Bull R Coll Surg Engl. 2017;99:260–263. [Google Scholar]
- 16.Half of UK health workers suffering stress because of Covid-19. https://www.theguardian.com/society/2020/apr/23/half-of-uk-health-workers-suffering-stress-because-of-covid-19 The Guardian. 2020. Available at: Accessed May 05,2020.
- 17.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien) 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAbee J.H., Ragel B.T., McCartney S. Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J Neurosurg. 2015;123:161–173. doi: 10.3171/2014.12.JNS141348. [DOI] [PubMed] [Google Scholar]