Abstract
COVID-19 is a significant worldwide challenge to many healthcare systems. In Trauma and Orthopaedics, there has been a significant change in the workload but departments have been compelled to change their practice in order to match the demand, as well as respond to the escalating situation of COVID. Some guidance is available on these changes from bodies such as the National Health Service (NHS), Public Health England and the British Orthopaedic Association (BOA). We have implemented certain changes in our university district general hospital trauma and orthopaedic department with regard to staff roles, outpatient and inpatient care and operative protocols. We aim to present some of these changes and their effects on patient care in an attempt to share these with colleagues who may face similar pressures and make some recommendations to help others prepare for a possible second wave of COVID-19.
Keywords: COVID, Orthopaedics, Response
1. Introduction
“…and there are no more surgeons, urologists, orthopaedists, we are only doctors who suddenly become part of a single team to face this tsunami that has overwhelmed us …” (Dr Daniele Macchine, Bergamo, Italy, March 2020).1 COVID-19, has had a significant impact on the entire health system since late December 2019 where the first cases were reported in Wuhan, China.2
All specialties have had to adapt their practices to cope with the change in demand. In trauma and orthopaedics, we have seen a significant change to our working practice, with most elective surgery stopped3 and only emergency trauma cases to be considered for operation.4 Provision of additional intensive care capacity, reduction of theatre space for trauma operating lists, compounded by increased patient turnaround time, has led to a significant decline in our operating efficiency.
Therefore, it has been necessary for us to adapt and this appears to be in line with the very limited evidence that appears in the literature.5 This is in order to free up resources, such as hospital beds, and staff to help deal with patients diagnosed with, or suspected to have, COVID-19 as well to improve safety amongst staff to try and restrict the spread of the disease.
We have based our changes on British Orthopaedic Association (BOA) Standards for Trauma (BOAST) COVID-19 Guidance,6 NHS England1 and Public Health England Guidance,7 as well as local consultant consensus, as recommended by the BOA.6
Specific changes made in our department can be divided into measures taken with regard to staff management, outpatient care and operative care and will be discussed in detail in a further section.
1.1. Guidance available
National guidance on how to adapt practice to meet the demands on the health system have been provided by bodies such as NHS England,1 Public Health England7 and the British Orthopaedic Association.6 The National Institute of Clinical Excellence (NICE) refers readers to the Public Health England and NHS England guidance.
NHS England has advised that urgent trauma inpatient care must continue to the highest standard possible, such as fracture neck of femur care, and that this should be expedited to minimise delay and hospital length of stay.1 This care should be consultant-delivered, with a priority placed on managing other urgent injuries (such as paediatric) as a day case and avoid unnecessary admissions. Other adaptations suggested include A&E immediately triaging a musculoskeletal injury straight to trauma and orthopaedics. The recommendation is for elective work to stop or be reduced to a minimum but urgent elective cases, such as infected prostheses still need to be monitored.1
The relevant Public Health England Guidance has been primarily focussed around theatre management of the patients and recommends that the patient wear a surgical mask where tolerated, anaesthetising and recovering the patient in theatre and advice around the level of Personal Protective Equipment (PPE) that needs to be worn for certain parts of the operative journey and by which members of staff. There is also limited guidance about what constitutes an “aerosol-generating procedure” and how the PPE worn and precautions taken should differ.7
The British Orthopaedic Association has produced a document entitled British Orthopaedic Association Standard for Trauma (BOAST) for COVID-19.6 It also advises consultant-delivered activities, adherence to PPE guidelines, measures to reduce encounters with healthcare professionals, such as use of splints which patients can remove themselves instead of plaster, rationalisation of follow-up imaging, clinical consideration of treatment of certain injuries conservatively and conversion of follow up appointments to telephone rather than face-to-face. In addition, consultant-delivered input to assist A&E in dealing with musculoskeletal injuries is recommended. A specific section on paediatric orthopaedics is provided, with regard to immobilisation of certain injuries and classifications of urgency of certain conditions such as slipped upper femoral epiphysis.
1.2. Changes made in our department
We are a department of 15 consultants, 10 registrars and 10 senior house officers. Therefore, consultants participate in a 1-in-15 weekday and 1-in-10 weekend on-call. On-calls are consultant-delivered. The consultant is first on-call in the “trauma hub”, which is adjacent to Accident and Emergency as part of the “Trauma and Orthopaedic Transformation Programme” (TOTP) in the Trust. This means there is a timely consultant review of every case, in line with the guidance available.
The most significant staff management changes have resulted from local consultant consensus, based upon the guidance available. This includes implementation of a daily video-conferenced trauma meeting to restrict the numbers of staff present. This is hosted from the education centre of the hospital via a video conferencing system. This is accessed remotely and securely by other members of the department. This appears to have been adopted in other centres as well.3,5
There is a strict in-person attendance policy of only the on-call emergency team, the trauma operating team and the ward cover team to ensure the number of people present in the room is limited, thus reducing the risk of spread of the virus to those present. It has also led to the creation of a three-tier backup system whereby two separate reserve staff members for the aforementioned activities are available to step up, should the rostered staff member have to self-isolate/is taken ill.
Another significant staff management change is the redeployment of 8 junior members of the orthopaedic team to the intensive care unit rota to assist with their management of COVID-19 patients. Whilst it is important to support the clinical response to COVID-19, this has introduced an initial element of anxiety within this team as a result of being placed in an unfamiliar environment and speciality to deal with confirmed COVID-19 patients. However, in hindsight, the junior team is well supported and the initial concern allayed. Additionally, we have followed the advice published by Health Education England8 on the support of the clinical response to COVID-19 specific to trainees, accepting that surgical exposure to trauma and orthopaedic cases has been reduced during this process. Despite this, trainees have been very supportive under the special circumstances. Similarly, the existing rota gaps have been efficiently covered by volunteers from the remainder of the trauma and orthopaedic team.
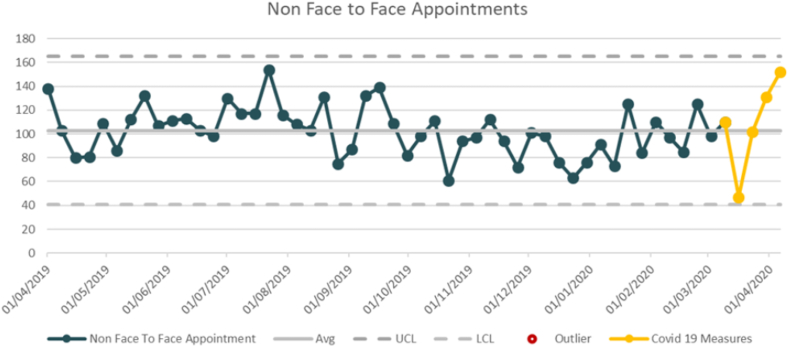
With regard to outpatient care, we have followed BOA Guidance6 and significantly reduced the number of face-to-face consultations in fracture clinic, with face-to-face consultations reserved for patients requiring physical examinations and wound checks. The remainder of consultations are performed over the telephone and documented appropriately. The increase in the number of these consultations is shown in Fig. 1.
Fig. 1.
Graph showing the average number of telephone consultations per week before COVID measures were introduced and during the first three weeks of COVID measures.
Our Trust has a catchment population of 7200009 and there are 6 Minor Injuries Units in the area. Patients requiring follow up radiograph are directed to their closest unit, where it is easier to practice social distancing measures, thereby reducing the risk of exposure of these patients to the acute medical sites. The radiographs are subsequently reviewed and followed up by a telephone consultation as necessary. In urgent cases, we call patients to the “Hot Clinic” which is delivered by the on-call consultant, for issues such as wound infection queries. These patients are asked a series of screening questions regarding symptoms of COVID-19 and are requested to observe strict hygiene measures.
Another system used in our institution is the “AccuRX” video consultation system (https://www.accurx.com/covid-19) for patient review. It securely sends a patient a link via SMS message, which takes them to a secure video chat room with the clinician. This can be then used to allow the clinician to observe clinical examination features such as range of motion of a joint and review a wound.
It is recognised that the risk of bringing patients to hospital may outweigh any benefit with regards to their orthopaedic injury6 hence the trauma and orthopaedic service provides consultant-delivered advice to GPs and minor injuries units to minimise patients brought into the hospital. This means that the consultant is first on-call, delivering the most appropriate advice rapidly.
For operative care changes, the most significant is the cessation of elective operating. It was gradually reduced at the beginning of the upward trend of the pandemic, in both the National Health and private sectors. This has released many members of staff for redeployment to other roles during this time, as previously described.
An emergency trauma service has continued throughout, and cases have been divided into inpatient trauma (such as fracture neck of femur) and ambulatory trauma (examples of which are ankle fractures and upper limb fractures). Ambulatory trauma is carried out within independent hospitals in the local area, which provides us with additional capacity. There tends to be strict criteria for facilitation of these, such as a proven negative COVID-19 swab and American Society of Anaesthesiologists (ASA) score restrictions.
In line with BOAST COVID-19 guidance,6 we have increased the number of fractures which have been treated conservatively. Examples of this include distal radius fractures which are minimally-displaced. Management includes placing these fractures in splints instead of plaster cast to avoid return to hospital for removal. It also includes Weber A and some Weber B ankle fractures as well as some paediatric fractures.
We have made a number of adaptations to surgical techniques such as the use of dissolvable sutures in all cases. This appears to have been adopted in other centres.3
Another significant concern is the risk of COVID-19 being spread by surgical aerosol-generating-procedures (AGPs) such as drilling, sawing, reaming and the use of diathermy, which can all produce aerosol to different levels.10 The BOA6 and Public Health England7 have provided some guidelines to this effect. On this basis, our Trust has recommended that all staff performing any orthopaedic procedure should use full PPE. However, a recent research report published in Nature shows that there is no viral load detected in blood.11 The “donning and doffing” protocols as well as the safety protocols implemented as per Public Health England guidelines for intubation and extubation of patients with COVID-19 have added to the overall turnaround time for each patient, contributing to a not-insignificant reduction in our trauma operating capacity. Other measures that have been introduced include covering the power tools with a plastic sheet, reduced use of diathermy and cessation of use of a saw in hip hemiarthroplasty (with bone cutters and nibblers preferred) and stopping the use of pulsed lavage. The number of surgeons has been strictly limited to one operator and one assistant to conserve PPE.
The above changes in protocols have increased patient turnaround time significantly. Public Health England Guidance7 was adopted with regards to anaesthetising and recovering the patient in theatre. Initially, only one theatre was available to the trauma team hence the process of anaesthetising, operating and recovering the patient, then cleaning the theatre often lasted around 4 hours, making it difficult to complete more than two cases on average on a daily list. In order to overcome this, a second theatre space was obtained. The anaesthetic, surgical and nursing teams would transfer to the second theatre to start the next case, allowing the first theatre to be free for recovering the operated patient and subsequent cleaning protocols. This increased the operating capacity up to 4 cases a day, utilising the same number of team members.
2. Conclusion
In summary, we have successfully made multiple changes to our working practices to allow us to adapt to the demand of the outbreak. These include:
-
•
Implementation of a daily virtual trauma meeting
-
•
Increased use of telephone clinics, with or without video consultations
-
•
Use of a separate COVID-free site to complete ambulatory trauma
-
•
Minimisation of number of staff on site to reduce the risk of spread of COVID-19
-
•
Reduction of intra-operative aerosol-generating practices such as pulsed lavage and use of power tools
We recommend that our colleagues adopt the appropriate policies to reduce risk to staff and patients so that in the possible event of a second wave/peak of COVID, departments are ready to adapt to the changing demand.
Lists of meetings presented at
None to Declare.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Funding
None to declare.
Author contribution
GF designed and wrote the majority of this manuscript with BT, IO and JR providing critical analysis and an opinion on its final contents.
Declaration of competing interest
None to Declare.
Contributor Information
Giles Faria, Email: gilesfaria@doctors.org.uk.
Baha John Tadros, Email: b_tadros@yahoo.com.
References
- 1.https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0274-Specialty-guide-Orthopaedic-trauma-v2-14-April.pdf
- 2.Chang Liang Z., Wang W., Murphy D., Po Hui J.H. Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Jt Surg Am. 2020;(published online ahead of print, 2020 Mar 20) doi: 10.2106/JBJS.20.00236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stinner D., Lebrun C., Hsu J., Jahangir A., Hassan R. The orthopaedic trauma service and COVID-19 – practice considerations to optimize outcomes and limit exposure. J Orthop Trauma. 2020 doi: 10.1097/BOT.0000000000001782. April 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaishya R., Vaish A. Roles and responsibilities of the orthopaedic community and the society during COVID-19 pandemic. Indian J Orthop. 2020;1–2 doi: 10.1007/s43465-020-00105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mauffrey C., Trompeter A. Lead the way or leave the way: leading a Department of Orthopedics through the COVID-19 pandemic. Eur J Orthop Surg Traumatol. 2020;30(4):555–557. doi: 10.1007/s00590-020-02670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf
- 7.https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe
- 8.https://www.hee.nhs.uk/coronavirus-information-trainees
- 9.https://www.nhs.uk/Services/Trusts/Overview/DefaultView.aspx?id=1768
- 10.Yeh H.C., Turner R.S., Jones R.K., Muggenburg B.A., Lundgren D.L., Smith J.P. Characterization of aerosols produced during surgical procedures in hospitals. Aerosol Sci Technol. 1995;22(2):151–161. [Google Scholar]
- 11.Wölfel R., Corman V.M., Guggemos W. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.