Abstract
Objective
To assess the prevalence and sociodemographic correlates of insomnia symptoms among Chinese adolescents and young adults affected by the outbreak of coronavirus disease-2019 (COVID-19).
Methods
This cross-sectional study included Chinese adolescents and young adults 12–29 years of age during part of the COVID-19 epidemic period. An online survey was used to collect demographic data, and to assess recognition of COVID-19, insomnia, depression, and anxiety symptoms using the Pittsburgh Sleep Quality Index (PSQI), the Patient Health Questionnaire (PHQ-9), and the Generalized Anxiety Disorder (GAD-7) questionnaires, respectively. The Social Support Rate Scale was used to assess social support.
Results
Among 11,835 adolescents and young adults included in the study, the prevalence of insomnia symptoms during part of the COVID-19 epidemic period was 23.2%. Binomial logistic regression analysis revealed that female sex and residing in the city were greater risk factors for insomnia symptoms. Depression or anxiety were risk factors for insomnia symptoms; however, social support, both subjective and objective, was protective factors against insomnia symptoms. Furthermore, anxiety and depression symptoms were mediators of social support and insomnia symptoms.
Conclusions
Results of this study revealed a high prevalence of sleep problems among adolescents and young adults during the COVID-19 epidemic, especially senior high school and college students, which were negatively associated with students’ projections of trends in COVID-19. The adverse impact of COVID-19 was a risk factor for insomnia symptoms; as such, the government must devote more attention to sleep disorders in this patient population while combating COVID-19.
Keywords: Insomnia, COVID-19, Prevalence, Adolescents, Young adults
Abbreviations: COVID-19, coronavirus disease-2019; OR, odds ratio; CI, confidence interval; PSQI, Pittsburgh Sleep Quality Index; PHQ-9, Patient Health Questionnaire; GAD-7, Generalized Anxiety Disorder scale; SARS CoV-2, severe acute respiratory syndrome coronavirus-2; SSRS, Social Support Rate Scale
Highlights
-
•
An online survey was used to conduct rapid assessment during the COVID-19 epidemic.
-
•
Sleep problems among adolescents and young adults were negatively associated with the level of projections of COVID-19 trend.
-
•
Social support (including subjective support and objective support) was a protective factor for insomnia symptoms.
-
•
Anxiety and depression symptoms were mediators between social support and insomnia symptoms.
1. Introduction
Sleep disorders represent an important public health problem, and affect individuals across several age groups, including adolescents and young adults, with severe consequences for both the individual and society. Previous studies have found that insomnia is the most prevalent sleep disorder among adolescents [[1], [2], [3], [4]] and young adults [5]. The prevalence of insomnia symptoms in Chinese adolescents range from 3.4% to 12.2% [6], and the percentage of Chinese young adults experiencing insomnia symptoms is 20.3% [7]. Sleep disorders in adolescents and young adults are characterized by a lack of sleep, difficulty falling asleep, or remaining asleep [8].
Insomnia in adolescents and young adults is mainly related to demographic and psychosocial factors. Several studies have reported that insomnia symptoms are more common in girls [9,10] and older adolescents [10]. Stress and poor mental health are important psychosocial factors contributing to insomnia [10,11]. Intensive research has revealed that acute insomnia may be regarded as a physiological response to acute stressors or “threats” [[12], [13], [14], [15]]. Stressful environmental events have been associated with insomnia [15] and, for individuals experiencing stress, research has shown that, to some extent, social support is a helpful resource for coping with stress and an important protective factor in ensuring sleep quality [[16], [17], [18]].
Coronavirus disease-2019 (COVID-19) first emerged in Wuhan, Hubei province, China, on December 31, 2019 and was later declared an international public health emergency by the World Health Organization [19]. COVID-19 has spread to 212 countries/territories outside of China and, the causative virus, severe acute respiratory syndrome coronavirus-2 (SARS CoV-2) has infected 3,018,681 patients globally [20] (82,862 in China [21]) as of April 30, 2020. Because so many individuals and countries have been affected rapidly, it has caused public panic and mental health stress [22]. Many individuals have developed symptoms of anxiety, depression, and insomnia due to COVID-19. However, previous studies have focused primarily on health care workers and adults, and little attention has been devoted to the relationship between mental health status and insomnia symptoms in adolescents and young adults [[22], [23], [24], [25]]. In particular, adolescents and young adults are experiencing complex situations such as school suspension, online classes at home, and reduced activities during the COVID-19 epidemic. Therefore, it is necessary to quickly assess sleep disorders related to emergencies induced by the epidemic.
The objective of the current study was to assess the prevalence of and factors influencing insomnia symptoms among adolescents and young adults in the Chinese population during part of the COVID-19 outbreak.
2. Material and methods
2.1. Study population and design
The present cross-sectional study was conducted using an online survey to assess mental health problems from March 8 to March 15, 2020. Junior and senior high school students, and college students in China 12–29 years of age were invited to participate in the online survey through the Wenjuanxing platform (https://www.wjx.cn/app/survey.aspx). In total, 12,299 participants participated in the survey. After removing individuals who submitted incomplete questionnaires, 11,835 subjects from 21 provinces and autonomous regions were included in the analysis.
Approval for the study was obtained from the Ethics Committee of Beijing HuiLongGuan Hospital (Beijing, China). All subjects provided informed online consent to participate in the study.
2.2. Measurement
A data collection sheet was designed to collect basic sociodemographic information, while student awareness of COVID-19 (including knowledge and projections of future trends in the disease), adverse impact(s) of COVID-19, and insomnia symptoms were assessed using an online survey. The surveys addressing awareness of COVID-19 and its adverse impact(s) asked participants to select responses using a self-administered questionnaire. The self-administered questionnaire mainly includes the following three questions: (1) How well do you know about COVID-19? (2) Do you think COVID-19 has an impact on your normal study and life? (3) Are you optimistic or pessimistic about the development trends of COVID-19? First, subjects were asked about their familiarity with information about prevention and control of COVID-19, with responses ranging from 1 (“very unfamiliar”) to 5 (“very familiar”). Second, subjects were asked about their attitudes toward projections of trends in COVID-19, ranging from 1 (“very pessimistic”) to 5 (“very optimistic”). Third, subjects were asked whether the COVID-19 epidemic had seriously affected their normal study and life, with responses ranging from 1 (“none”) to 5 (“severe”).
Insomnia symptoms were assessed using the Pittsburgh Sleep Quality Index (PSQI) [7,26,27]. The PSQI is a self-rated questionnaire that assesses seven components of sleep quality during the previous month: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. A total of 19 items were rated on a scale scored from 0 to 3 (0, not during the past month; 3, ≥3 times a week), with the total PSQI score ranging from 0 to 21 and a global score > 5 indicating poor sleep quality [26,28]. Previous studies have demonstrated that the scale has good reliability and validity in the Chinese adolescent and college population [29,30].
Depression symptoms were assessed using the Patient Health Questionnaire (PHQ-9) [[31], [32], [33], [34]], which consists of nine items. The PHQ-9 is a simple, highly effective, self-assessment tool for depression. Participants are asked to report the presence of nine problems, including depression and declines in interest in the past two weeks on a four-point scale ranging from “nearly every day” (3 points) to “not at all” (0 points) [32,34]. The scores for symptom severity were 5–9 for mild, 10–14 for moderate, 15–19 for moderately severe, and 20–27 for severe. The PHQ-9 has good internal consistency, with a Cronbach's alpha coefficient of 0.80–0.90 [[31], [32], [33], [34]]. Reliability and validity of the PHQ-9 in the general population, as well as in patients with mental disorders, have been demonstrated [35,36].
Anxiety symptoms were assessed using the Chinese version of the Generalized Anxiety Disorder Scale (GAD-7) [37,38], which measures seven symptoms. Participants were asked how often they were bothered by each symptom during the past two weeks. The response options were “not at all”, “several days”, “more than half the days” and “nearly every day”, and scored as 0, 1, 2, and 3, respectively. The scores for symptom severity were 5–9 for mild, 10–14 for moderate, and 15–21 for severe [37,38]. Good retesting reliability and validity for the GAD-7 have been confirmed in Chinese individuals [39], with a Cronbach's alpha of 0.90–0.92 [37,40].
Social support was assessed using the Social Support Rate Scale (SSRS) [41,42]. The scale was developed by Xiao Shuiyuan in 1968 and contains 10 items encompassing three dimensions: objective support, subjective support, and use of social support. A higher total score indicates a higher level of social support. The Cronbach coefficient for the SSRS is 0.89–0.94. The present study mainly evaluated the two dimensions: objective support and subjective support [41,43].
2.3. Statistical analyses
Data were analyzed using SPSS version 24.0 (IBM Corporation, Armonk, NY, USA). The chi-squared test was used to compare sex, age, presence or absence of anxiety, and depression symptoms with the prevalence of insomnia symptoms in junior and high school students, college students, and the total sample. The same method was used to separately compare the incidence of insomnia symptoms in junior and senior high school students, college students, and the overall sample in terms of familiarity with COVID-19 knowledge, predicted/projected trends in COVID-19, and the extent to which individual learning and life was affected by COVID-19. Chi-squared tests were also used to compare the incidence of insomnia symptoms and the distribution of factors related to insomnia symptoms in different groups. At the same time, the incidence of insomnia symptoms and the proportion of insomnia symptom-related factors were calculated in the total sample. Binomial logistic regression was used to analyze the predictors of insomnia symptoms. With versus without insomnia symptoms represented dichotomous dependent variables; the level of statistical significance was set at 0.05 (two-sided).
The SPSS function “PROCESS macro” was used for mediation analysis. According to the results of linear regression, the mediating effect model was as follows: X represented the score of subjective support and objective support, Y represented the total score of PSQI, and M represented the scores of the PHQ-9 and GAD-7 questionnaires. The relationship between independent variables, mediating variables, and dependent variables is presented in the form of plots. Regression coefficients represent the magnitude and direction of the effect on another variable in each model. The bootstrap method was used to test the mediating effect, and the sample size was set to 5000. A 95% confidence interval for indirect effects without zero was statistically significant.
3. Results
A total of 12,299 junior and senior high school, and college students were invited to participate in the online survey, 11,835 of whom (12–29 years of age [mean age, 17.41 ± 2.70 years) fulfilled the study inclusion criteria and completed the assessments, corresponding to a response rate of 96.2%. Results revealed that the proportion of men with insomnia symptoms was lower than that of women among junior and senior high school students (15.9% versus [vs.] 20.0%; 22.4% vs. 27.5%, respectively); however, there was no significant difference among college students (Table 1 ). Among the total study population, the incidence of insomnia symptoms in male students was lower than that in female students. Results of chi-squared testing revealed that the proportion of insomnia symptoms among senior high school and college students in cities was lower than that in rural areas (37.7% vs. 47.5%; 22.4% vs. 27.5%, respectively). Among students with depression symptoms (42.9%), 44.8% experienced insomnia symptoms. Similarly, among students with anxiety symptoms (34.4%), 44.4% experienced insomnia symptoms.
Table 1.
Socio-demographic characteristics, depression symptoms, anxiety symptoms and associations with insomnia symptoms (N = 11,835).
| Variables | Junior high school |
Senior high school |
College |
Total |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. (%) |
Insomnia |
No. (%) |
Insomnia |
No. (%) |
Insomnia |
No. (%) |
Insomnia |
|||||
| n (%) | P | n (%) | P | n (%) | P | n (%) | P | |||||
| Sex | 0.001 | <0.001 | 0.16 | <0.001 | ||||||||
| Male | 1757 (49.1) | 279 (15.9) | 1818 (43.8) | 407 (22.4) | 1434 (35.0) | 350 (24.4) | 5009 (42.3) | 1036 (20.7) | ||||
| Female | 1830 (51.0) | 366 (20.0) | 2331 (56.2) | 641 (27.5) | 2665 (65.0) | 740 (26.4) | 6826 (57.7) | 1711 (25.1) | ||||
| Region | 0.706 | 0.002 | 0.016 | 0.185 | ||||||||
| City | 1611 (44.9) | 294 (18.2) | 1339 (32.3) | 298 (22.3) | 1286 (31.4) | 362 (28.1) | 4236 (35.8) | 954 (22.5) | ||||
| Rural area | 1976 (51.0) | 351 (17.8) | 2810 (67.7) | 750 (26.7) | 2813 (68.6) | 692 (24.6) | 7599 (64.2) | 1793 (23.6) | ||||
| Depression | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Yes | 1403 (39.1) | 534 (38.1) | 2069 (49.9) | 940 (45.4) | 1605 (39.2) | 801 (49.9) | 5077 (42.9) | 2275 (44.8) | ||||
| No | 2184 (60.9) | 111 (5.1) | 2080 (50.1) | 108 (5.2) | 2494 (60.8) | 253 (10.1) | 6758 (57.1) | 472 (7.0) | ||||
| Anxiety | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Yes | 1261 (35.2) | 441 (35.0) | 1701 (41.0) | 769 (45.2) | 1112 (27.1) | 600 (54.0) | 4074 (34.4) | 1810 (44.4) | ||||
| No | 2326 (64.8) | 204 (8.8) | 2448 (59.0) | 279 (11.4) | 2987 (72.9) | 454 (15.2) | 7761 (65.6) | 937 (12.1) | ||||
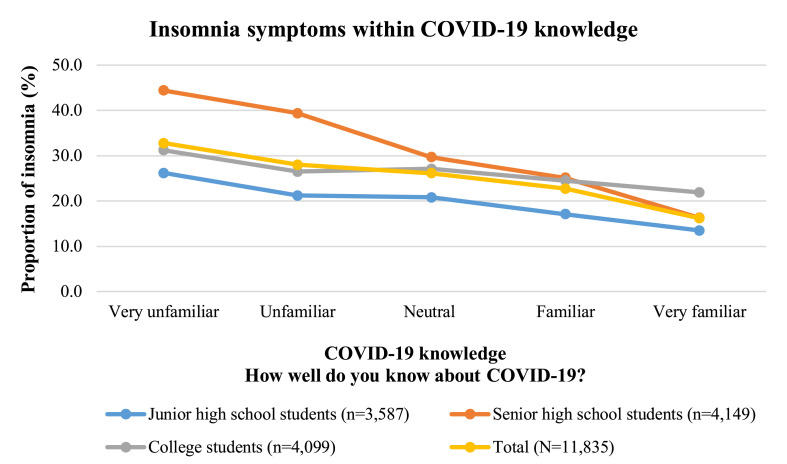
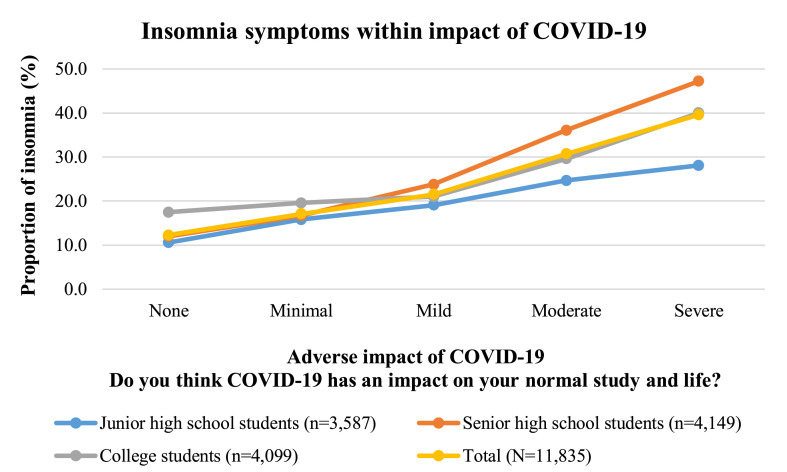
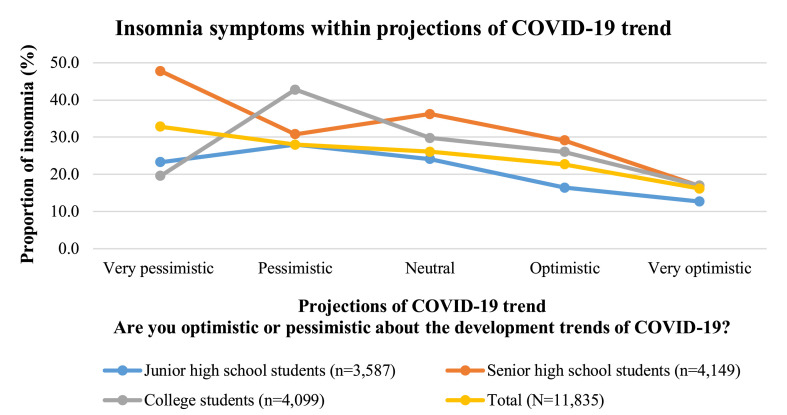
The incidence of insomnia symptoms in students with different levels of COVID-19 knowledge is presented in Fig. 1 . The lesser the knowledge about COVID-19, the higher the rate of insomnia symptoms among students. The rate of insomnia symptoms in students with different levels of adverse impact from COVID-19 are shown in Fig. 2 . The more serious the influence of COVID-19 on students’ study and life, the higher the incidence of insomnia symptoms. Fig. 3 shows the incidence of insomnia symptoms in students with different levels of projections regarding trends in COVID-19. The more optimistic the projections about trends in COVID-19, the lower the rate of insomnia symptoms among students.
Fig. 1.
The incidence of insomnia symptoms in students with different levels of COVID-19 knowledge (N = 11,835).
Fig. 2.
The incidence of insomnia symptoms in students with different levels of adverse impact of COVID-19 (N = 11,835).
Fig. 3.
The incidence of insomnia symptoms in students with different levels of projections of COVID-19 trend (N = 11,835).
As shown in Table 2 , 23.2% of the sample experienced insomnia symptoms, with 18.0%, 25.3%, and 25.7% of junior school students, high school students, and college students, respectively, experiencing difficulty in sleeping. The proportions of poor sleep quality, sleep disturbance(s), and use of sleep medication were higher in college students compared with junior and senior school students. Furthermore, the proportion of college students who went to bed after 24:00 was significantly higher than that of junior and senior high school students (43.8% vs. 7.9% and 4.5%, respectively). In addition, the sleep efficiency of college students was the worst, with 27.4% at < 85%. For senior high school students, sleep duration was the worst, and more than one-half of high school students slept <7 h per night. Daytime dysfunction caused by insomnia was also more prominent in high school students, 59.3% of whom were affected. However, their sleep efficiency was best, with only 16.7% exhibiting an efficiency ≤85%. Generally speaking, junior school students slept better; however, the proportion of junior school students who slept >9 h per night was higher.
Table 2.
The incidence rate and patterns of insomnia symptoms (N = 11,835).
| Variables | Junior high school |
Senior high school |
College |
P |
Total |
||||
|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | ||
| Insomnia | 645 | 18.0bc | 1048 | 25.3a | 1054 | 25.7a | <0.001 | 2747 | 23.2 |
| Subjective sleep quality | <0.001 | ||||||||
| Excellent | 1793 | 49.9bc | 1694 | 40.8ac | 1585 | 38.7ab | 5072 | 42.8 | |
| Good | 1493 | 41.6bc | 1945 | 46.9a | 1925 | 47.0a | 5363 | 45.3 | |
| Bad | 254 | 7.1ab | 436 | 10.5ac | 515 | 12.6bc | 1205 | 10.2 | |
| Poor | 53 | 1.5 | 75 | 1.8 | 74 | 1.8 | 202 | 1.7 | |
| Sleep latency | <0.001 | ||||||||
| ≤15 min | 2069 | 57.7c | 2390 | 57.6c | 2076 | 50.6ab | 6535 | 55.2 | |
| 16–30 min | 1167 | 32.5c | 1399 | 33.7c | 1538 | 37.5ab | 4104 | 34.7 | |
| 31–60 min | 251 | 7.0c | 280 | 6.7c | 349 | 8.5ab | 880 | 7.4 | |
| ≥60 min | 100 | 2.8b | 80 | 1.9ac | 135 | 3.3b | 316 | 2.7 | |
| Sleep duration (hours) | <0.001 | ||||||||
| No more than 7 | 816 | 22.7bc | 2080 | 50.1ac | 1134 | 27.7ab | 4030 | 34.0 | |
| Greater than 7 and not greater than 9 | 2385 | 66.4bc | 1949 | 47.0ac | 2592 | 63.2ab | 6926 | 58.5 | |
| More than 9 | 392 | 10.9bc | 373 | 2.9ac | 373 | 9.1ab | 886 | 7.5 | |
| Sleep efficiency | 837 | 23.3bc | 691 | 16.7ac | 164 | 27.4ab | 2651 | 22.4 | |
| Bedtime | <0.001 | ||||||||
| Before 22 o'clock | 1208 | 33.8bc | 286 | 6.9ac | 164 | 4.0ab | 1658 | 14.0 | |
| Greater than or equal to 22 o'clock and less than 24 | 2087 | 58.3bc | 3325 | 80.4ac | 2138 | 52.2ab | 7550 | 63.9 | |
| No less than 24 o'clock | 282 | 7.9bc | 527 | 4.5ac | 1797 | 43.8ab | 2606 | 22.1 | |
| Sleep disturbance | 1880 | 52.3bc | 2403 | 57.9ac | 2731 | 66.6ab | <0.001 | 7015 | 59.2 |
| Used sleep medication | 23 | 0.6bc | 61 | 1.5ac | 99 | 2.4ab | <0.001 | 183 | 1.5 |
| Daytime dysfunction | 1602 | 44.6bc | 2463 | 59.3ac | 2277 | 55.6ab | <0.001 | 6342 | 53.6 |
a Compared with junior high school, P < 0.05.
b Compared with senior high school, P < 0.05.
c Compared with college, P < 0.05.
Results of binary logistic regression analysis of the factors associated with insomnia symptoms are summarized in Table 3 . In the logistic regression model, female sex was a stronger risk factor for insomnia symptoms (odds ratio [OR] 1.301 [95% CI 1.175–1.441]). With regard to the effect on grades, attending senior high school and college were risk factors for insomnia (OR 1.378 [95% CI 1.210–1.568]; OR 2.033 [95% CI 1.768–2.338], respectively). With regard to region, residing in a city was a risk factor for insomnia symptoms (OR 1.183 [95% CI 1.065–1.315]). Depression and anxiety were risk factors for insomnia (OR 6.361 [95% CI 5.599–7.227]; OR 2.059 [95% CI 1.835–2.310], respectively). Projections of trends in COVID-19 were protective factors against insomnia symptoms (OR 0.919 [95% CI 0.875–0.965]). The adverse impact of COVID-19 was a risk factor for insomnia (OR 1.165 [95% CI 1.112–1.222]). Regarding social support, subjective and objective support were protective factors against insomnia symptoms (OR 0.967 [95% CI 0.957–0.978]; OR 0.991 [95% CI 0.988–0.995], respectively).
Table 3.
Binary regression analyses of the factors associated with insomnia (N = 11,835).
| Variables | B | SE | OR | 95%CI | P |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 1 | ||||
| Female | 0.263 | 0.052 | 1.301 | 1.175–1.1.441 | <0.001 |
| Institution | |||||
| Junior high school | 1 | ||||
| Senior high school | 0.320 | 0.066 | 1.378 | 1.210–1.568 | <0.001 |
| College | 0.710 | 0.071 | 2.033 | 1.768–2.338 | <0.001 |
| Region | |||||
| Rural area | 1 | ||||
| City | 0.168 | 0.054 | 1.183 | 1.065–1.315 | 0.002 |
| Depression | |||||
| No | 1 | ||||
| Yes | 1.850 | 0.065 | 6.361 | 5.599–7.227 | <0.001 |
| Anxiety | |||||
| No | 1 | ||||
| Yes | 0.722 | 0.059 | 2.059 | 1.835–2.310 | <0.001 |
| COVID-19 knowledge | −0.013 | 0.02 | 0.987 | 0.964–1.010 | 0.255 |
| Adverse impact of COVID-19 | 0.153 | 0.024 | 1.165 | 1.112–1.222 | <0.001 |
| Projections of COVID-19 trend | −0.085 | 0.025 | 0.919 | 0.875–0.965 | 0.001 |
| Subjective support | −0.033 | 0.005 | 0.967 | 0.957–0.978 | <0.001 |
| Objective support | −0.009 | 0.002 | 0.991 | 0.988–0.995 | <0.001 |
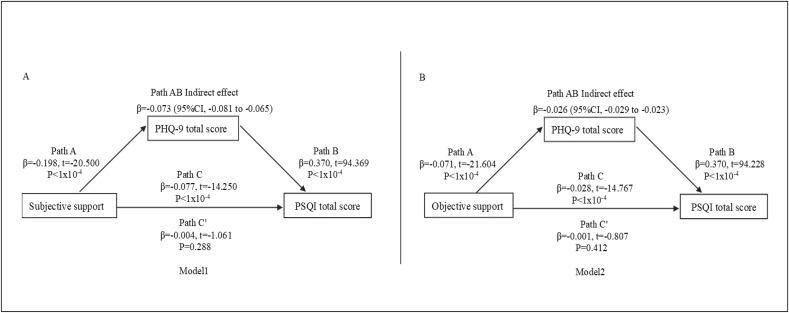
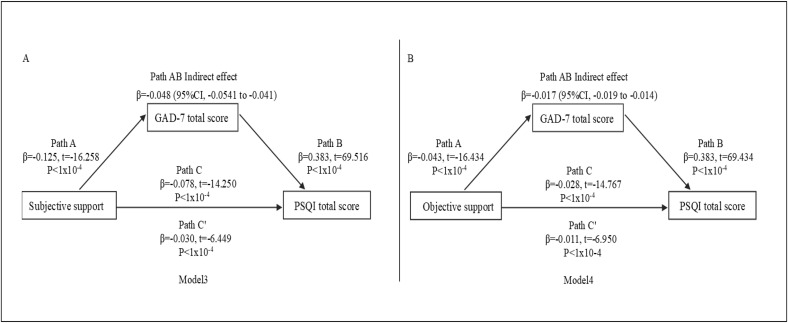
Linear regression revealed that subjective and objective support were protective factors for insomnia symptoms, anxiety, and depression symptoms, and the total PHQ-9 and GAD-7 scores were risk factors for insomnia symptoms (Supplementary Material 2). As shown in Fig. 4 (models 1 and 2), the indirect effects between subjective support, objective support, and PSQI total scores through the mediator (PHQ-9 total score) were significant, suggesting that models 1 and 2 were full mediation models. In models 3 and 4 (using the same format as model 1 and 2 to present the results; see Fig. 5 ), the direct effects were also significant, suggesting that models 3 and 4 had partial mediating effects.
Fig. 4.
A shoes model 1 path diagram of the mediation model (X = subjective support; Y= PSQI total score). Path C represent the variance in subjective support associated with PSQI total score. Path C′ represent the association between subjective support and PSQI total score after taking into account PHQ-9 total scores. B shows model 2 path diagram of the mediation model (X = subjective support; Y= PSQI total score). Path C represent the variance in subjective support associated with PSQI total score. Path C′ represent the association between subjective support and PSQI total score after taking into account GAD-7 total scores. Path AB is the mediation effect and is significant at P<0.05 based on 95% CI from bias-corrected bootstrapping of 5000 samples.
Fig. 5.
A shows model 3 path diagram of the mediation model (X = subjective support; Y= PSQI total score). Path C represent the variance in subjective support associated with PSQI total score. Path C′ represent the association between subjective support and PSQI total score after taking into account PHQ-9 total scores. B shows model 4 path diagram of the mediation model (X = subjective support; Y= PSQI total score). Path C represent the variance in objective support associated with PSQI total score. Path C′ represent the association between objective support and PSQI total score after taking into account GAD-7 total scores. Path AB is the mediation effect and is significant at P<0.05 based on 95% CI from bias-corrected bootstrapping of 5000 samples.
4. Discussion
The present large-scale, cross-sectional epidemiological study revealed that the prevalence of insomnia symptoms in adolescents and young adults in China during part of the COVID-19 epidemic period was 23.2%. Moreover, the prevalence of insomnia symptoms among senior high school and college students was higher. The prevalence of insomnia symptoms in adolescents was higher than that in the United States (9.4%) in the absence of epidemics [44]. The percentage of insomnia symptoms in young adults (25.7%) has been reported to be higher than the incidence reported for the general population in China (18.3–23.6%) in the absence of epidemics [7,45].
Results of analysis revealed that, during part of the COVID-19 epidemic, college students were more likely to experience declines in sleep quality, increased sleep times, later bedtimes, and sleep disturbances. Previous studies have reported that college students have poor sleep habits [46], and the COVID-19 epidemic has further worsened sleep habits by allowing college students to have more hours free from school. Poor sleep habits, such as staying up late due to increased mobile phone use, playing online games, and online shopping, also lead to decreased sleep hygiene/quality, prolonged sleep latency, and shorter sleep time, which is consistent with previous studies [9,47]. Among these, a small number of college students need to use sleep medication to regulate sleep.
Regarding senior high school students, the percentage of insomnia symptoms was also higher (25.3%), which was higher than that in the students without COVID-19 in China or other countries [6]. Stress during academic examination season is known to compromise sleep quality in students [48], and senior high school students in China have a heavy academic burden. In particular, third-grade senior school students are facing college entrance examinations [49]. As a result of the COVID-19 epidemic, they cannot go to school normally, and college entrance examinations were also forced to be postponed. These problems can easily lead to sleep disorders. More than one-half of senior high school students (50.1%) had insufficient sleep (<7 h per night), which was especially higher than college and junior high school students. In addition, sleep time was also generally later for senior high school students, with 80.4% going to sleep between 22:00 to 24:00. Less sleep and later sleep times lead to a decline in student daytime function, which also has an impact on learning efficiency and academic achievement [50,51]. Therefore, we should devote attention to sleep disorders among senior high school students. It should be ensured that they have sufficient rest and sleep time so that they can be in a good position to study during the daytime.
Moreover, insomnia was strongly associated with female sex. Previous studies have also shown that among those with insomnia, females predominated [44,52]. Anxiety and depression symptoms are risk factors for insomnia. As we know, there is a correlation and a cyclical relationship between anxiety, depression and insomnia. Anxiety and depression are risk factors for insomnia [53,54]. Many patients with anxiety disorders and depression are accompanied by insomnia, and some patients with anxiety disorders and depression disorder even suffer from co-morbid insomnia [55]. And in a lot of insomnia sufferer, are also co-morbid with anxiety, depressed disorder [56]. In addition, the comorbidity rate of anxiety and depression symptoms and insomnia has been relatively high. Studies have shown that sleep problems are common in individuals with anxiety and depression [57,58]. Some studies also suggest that persistent insomnia may be a risk factor for anxiety and depression disorder [59]. During the COVID-19 epidemic, many people (including adolescents and young adults) had symptoms of anxiety and depression [23], which exacerbated the symptoms of insomnia. In addition, prolonged insomnia can also lead to increased anxiety and depression symptoms, so it is important to pay attention to students' psychological problems and insomnia symptoms during the COVID-19 epidemic. In addition, the proportion of anxiety and depression in the female population was higher [25,60,61], which also aggravated insomnia symptoms. Students residing in cities were more likely to experience insomnia, which was consistent with previous research [62].
The COVID-19 epidemic has had a significant impact and is a risk factor for insomnia [24]. It has disrupted the normal learning and living conditions of students and affected their sleep hygiene [23]. However, a positive and optimistic attitude toward the COVID-19 epidemic can reduce insomnia. Therefore, students should endeavor to gain more knowledge about COVID-19 and increase their confidence in fighting the disease.
As most provinces and cities in China are currently determining school re-opening times, sleep problems may be partially alleviated. Therefore, we suggest that teachers devote attention to students’ sleep problems after schools open again. For students experiencing insomnia symptoms, we should actively promote counseling and intervention. Students who have not yet started school can survey their sleep status online in the form of a questionnaire at the same time as online classes.
In addition, our research has shown that good social support (subjective and objective support) can reduce insomnia symptoms as well as indirectly reduce insomnia symptoms by reducing anxiety and depression symptoms. Previous studies have reported similar results [18]. Therefore, it is particularly important for parents, teachers, and other social groups to provide support to students during the COVID-19 outbreak to reduce insomnia symptoms. We can also provide some sleep knowledge and videos of sleep intervention through mobile phones or computers, such as relaxation training and cognitive behavioral therapy for insomnia, to alleviate or relieve insomnia symptoms [63]. COVID-19 remains widespread globally. To date, nearly 3.0 million people globally have been infected with SARS CoV-2 [20]. Most of the world's schools are not open; as such, this may be an opportunity to devote attention to sleep problems.
This study had three limitations. First, possible bias could have led to the underestimation of the prevalence of insomnia symptoms. This sample was a non-probability sample, which is a sample of voluntary participants. For some areas with a severe epidemic, insomnia rates may be higher. However, due to the influence of anxiety and depression, students may not be willing to participate in a questionnaire survey [64], and there may be a certain deviation in the response population. Second, because the online questionnaire was a self-administered evaluation, the indicated levels of insomnia symptoms may not always be consistent with the evaluations of mental health professionals. Third, there were differences in the proportion of men and women in the study. Female students accounted for a relatively large proportion. The relatively high proportion of female students is mainly caused by the imbalance between male and female students in schools. In China, the proportion of female students in both high schools and universities is higher than that of male students on the whole, and the imbalance between male and female students among college students is more prominent. This is also the reason why the proportion of female students in this study is much higher than that of male students. Notably, this is also the limitation of this study, Gender matching should be carried out in future studies [65].
5. Conclusions
Results of the present study revealed a high prevalence of sleep problems among adolescents and young adults during part of the COVID-19 epidemic, especially among senior high school and college students, which were negatively associated with the level projection in trends in COVID-19. We have also found that social support can alleviate or reduce symptoms of insomnia by reducing symptoms of anxiety and depression, so parents, school organizations, and other groups should provide some social support to adolescents and young adults during the COCID-19 outbreak. These findings also suggest that the government needs to devote more attention to sleep problems among adolescents and young adults while combating COVID-19. Fortunately, the Chinese government has provided psychological health services through various channels, including hotlines, online consultation, and outpatient consultations [66]. Nevertheless, more attention should be devoted to sleep disorders, especially among senior high school and college students.
Funding
This work was supported by Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding, code: XMLX201806; Beijing Municipal Administration of Hospitals Incubating Program, code: PX2017070.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
Ethics Committee of Beijing HuiLongGuan Hospital approved the study.
CRediT authorship contribution statement
Shuang-Jiang Zhou: Conceptualization, Methodology, Validation, Data curation, Writing - original draft, Funding acquisition. Lei-Lei Wang: Conceptualization, Methodology, Data curation, Writing - original draft. Rui Yang: Funding acquisition, Investigation, Methodology, Supervision, Validation. Xing-Jie Yang: Investigation, Methodology. Li-Gang Zhang: Investigation, Methodology. Zhao-Chang Guo: Investigation, Methodology. Jin-Cheng Chen: Investigation, Methodology. Jing-Qi Wang: Investigation, Methodology. Jing-Xu Chen: Conceptualization, Project administration, Supervision, Writing - review & editing.
Acknowledgements
The authors would like to thank Jia-Ling Xue and Juan Liang for all of their hard work and significant contributions to the study. We would like to thank Editage (www.editage.cn) for English language editing.
Footnotes
All authors declare no competing financial interest.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2020.06.001.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleep.2020.06.001.
Conflict of interest
The following is the supplementary data related to this article:
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Multimedia component 2
References
- 1.Johnson E.O., Roth T., Schultz L. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:e247–e256. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 2.Kaneita Y., Ohida T., Osaki Y. Insomnia among Japanese adolescents: a nationwide representative survey. Sleep. 2006;29:1543–1550. doi: 10.1093/sleep/29.12.1543. [DOI] [PubMed] [Google Scholar]
- 3.Roberts R.E., Roberts C.R., Duong H.T. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42:294–302. doi: 10.1016/j.jadohealth.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amaral M.O., de Figueiredo Pereira C.M., Silva Martins D.I. Prevalence and risk factors for insomnia among Portuguese adolescents. Eur J Pediatr. 2013;172:1305–1311. doi: 10.1007/s00431-013-2037-0. [DOI] [PubMed] [Google Scholar]
- 5.Amaral A.P., Soares M.J., Pinto A.M. Sleep difficulties in college students: the role of stress, affect and cognitive processes. Psychiatr Res. 2018;260:331–337. doi: 10.1016/j.psychres.2017.11.072. [DOI] [PubMed] [Google Scholar]
- 6.Zhang J., Chan N.Y., Lam S.P. Emergence of sex differences in insomnia symptoms in adolescents: a large-scale school-based study. Sleep. 2016;39:1563–1570. doi: 10.5665/sleep.6022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li L., Wang Y.Y., Wang S.B. Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res. 2018;27 doi: 10.1111/jsr.12648. [DOI] [PubMed] [Google Scholar]
- 8.Yang C.M., Wu C.H., Hsieh M.H. Coping with sleep disturbances among young adults: a survey of first-year college students in Taiwan. Behav Med. 2003;29:133–138. doi: 10.1080/08964280309596066. [DOI] [PubMed] [Google Scholar]
- 9.Hysing M., Pallesen S., Stormark K.M. Sleep patterns and insomnia among adolescents: a population-based study. J Sleep Res. 2013;22:549–556. doi: 10.1111/jsr.12055. [DOI] [PubMed] [Google Scholar]
- 10.Liu X., Uchiyama M., Okawa M. Prevalence and correlates of self-reported sleep problems among Chinese adolescents. Sleep. 2000;23:27–34. [PubMed] [Google Scholar]
- 11.Zhang S.C., Yang R., Li D.L. Association of health literacy and sleep problems with mental health of Chinese students in combined junior and senior high school. PloS One. 2019;14 doi: 10.1371/journal.pone.0217685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellis J.G., Gehrman P., Espie C.A. Acute insomnia: current conceptualizations and future directions. Sleep Med Rev. 2012;16:5–14. doi: 10.1016/j.smrv.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 13.McNamara P.A.S. Cambridge University Press; New York, NY: 2010. Evolutionary medicine of sleep disorders: toward a science of sleep duration. [Google Scholar]
- 14.Riemann D., Spiegelhalder K., Feige B. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Nunn C.L., Samson D.R., Krystal A.D. Shining evolutionary light on human sleep and sleep disorders. Evol Med Public Health. 2016;2016:227–243. doi: 10.1093/emph/eow018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geng F., Fan F., Mo L. Sleep problems among adolescent survivors following the 2008 Wenchuan earthquake in China: a cohort study. J Clin Psychiatr. 2013;74:67–74. doi: 10.4088/JCP.12m07872. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto S., Yamaoka K., Inoue M. Implications for social support on prolonged sleep difficulties among a disaster-affected population: second report from a cross-sectional survey in ishinomaki, Japan. PloS One. 2015;10 doi: 10.1371/journal.pone.0130615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nursalam N., Octavia M., Tristiana R.D. Association between insomnia and social network site use in Indonesian adolescents. Nurs Forum. 2019;54:149–156. doi: 10.1111/nuf.12308. [DOI] [PubMed] [Google Scholar]
- 19.WHO . 2020. WHO director-general's statement on IHR emergency committee on novel coronavirus (2019-nCoV)https://wwwwhoint/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov [Google Scholar]
- 20.WHO . 2020. Coronavirus disease 2019 (COVID-19) situation report – 100.https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200429-sitrep-100-covid-19pdf?sfvrsn=bbfbf3d1_6 [Google Scholar]
- 21.NHCotPsRo C . 2020. Latest situation report of coronavirus disease 2019 (COVID-19)http://wwwnhcgovcn/xcs/yqfkdt/202004/ce78f5575e0d4ef0b4543eb072acebc3shtml [Google Scholar]
- 22.Bao Y., Sun Y., Meng S. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang C., Yang L., Liu S. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatr. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou S.J., Zhang L.G., Wang L.L. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatr. 2020:1–10. doi: 10.1007/s00787-020-01541-4. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buysse D.J., Reynolds C.F., 3rd, Monk T.H. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 27.Mah C.D., Kezirian E.J., Marcello B.M. Poor sleep quality and insufficient sleep of a collegiate student-athlete population. Sleep Health. 2018;4:251–257. doi: 10.1016/j.sleh.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Sing C.Y., Wong W.S. Prevalence of insomnia and its psychosocial correlates among college students in Hong Kong. J Am Coll Health. 2010;59:174–182. doi: 10.1080/07448481.2010.497829. [DOI] [PubMed] [Google Scholar]
- 29.Wang Y., Yu C.D., Yang X.T. Reliability and validity of Pittsburgh sleep quality index in adolescents with myopia. Mod Prev Med. 2019;46:1062–1069. [Google Scholar]
- 30.Liu X.C., Tang M.Q., Hu L. Reliability and validity of the Pittsburgh sleep quality index. Chinese journal of psychiatry. 1996;29:103–107. [Google Scholar]
- 31.Spitzer R.L., Kroenke K., Williams J.B. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. Jama. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wittkampf K.A., Naeije L., Schene A.H. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: a systematic review. Gen Hosp Psychiatr. 2007;29:388–395. doi: 10.1016/j.genhosppsych.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 34.Levis B., Benedetti A., Thombs B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365:l1476. doi: 10.1136/bmj.l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang W., Bian Q., Zhao Y. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatr. 2014;36:539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Y.L., Liang W., Chen Z.M. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatr. 2013;5:268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 37.Spitzer R.L., Kroenke K., Williams J.B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 38.Xu W.F., Peng Y., Chen B.Q. Assessment of anxiety and depression by self-rating scales of GAD-7 and PHQ-9 in cardiovascular outpatients. World Latest Medicine Information. 2018;18:12–14. (In Chinese) [Google Scholar]
- 39.He X.Y., Li C.B., Qian J. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Archives of Psychiatry. 2010;22:200–203. (In Chinese) [Google Scholar]
- 40.Beck A.T., Guth D., Steer R.A. Screening for major depression disorders in medical inpatients with the beck depression inventory for primary care. Behav Res Ther. 1997;35:785–791. doi: 10.1016/s0005-7967(97)00025-9. [DOI] [PubMed] [Google Scholar]
- 41.Xiao Shuiyuan Y.D. The influence of social support on physical and mental health. Chin Ment Health J. 1987;1:183–187. [Google Scholar]
- 42.Xiao H., Zhang Y., Kong D. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in january and february 2020 in China. Med Sci Mon Int Med J Exp Clin Res. 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang X.D., Wang X.L., Ma H. China Journal of Mental Health Press; Beijing: 1999. Rating scales for mental health; pp. 127–130. [Google Scholar]
- 44.de Zambotti M., Goldstone A., Colrain I.M. Insomnia disorder in adolescence: diagnosis, impact, and treatment. Sleep Med Rev. 2018;39:12–24. doi: 10.1016/j.smrv.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiang X.L., Zheng X.Y., Yang J. A systematic review of studies on the prevalence of insomnia in university students. Publ Health. 2015;129:1579–1584. doi: 10.1016/j.puhe.2015.07.030. [DOI] [PubMed] [Google Scholar]
- 46.Sivertsen B., Øverland S., Pallesen S. Trends in timing of sleep in the general population of Norway: 1980 to 20001. Percept Mot Skills. 2011;113:509–518. doi: 10.2466/02.06.13.PMS.113.5.509-518. [DOI] [PubMed] [Google Scholar]
- 47.Gellis L.A., Park A., Stotsky M.T. Associations between sleep hygiene and insomnia severity in college students: cross-sectional and prospective analyses. Behav Ther. 2014;45:806–816. doi: 10.1016/j.beth.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 48.Zunhammer M., Eichhammer P., Busch V. Sleep quality during exam stress: the role of alcohol, caffeine and nicotine. PloS One. 2014;9 doi: 10.1371/journal.pone.0109490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yuan F., Li Z.S., Yang Y.L. Prevalence of anxiety tested with Test Anxiety Scale(TAS) in senior three students: a Meta-analysis. Chin J Sch Health. 2018;39:1324–1328. (In Chinese) [Google Scholar]
- 50.Chan C.S., Poon C.Y.S., Leung J.C.Y. Delayed school start time is associated with better sleep, daytime functioning, and life satisfaction in residential high-school students. J Adolesc. 2018;66:49–54. doi: 10.1016/j.adolescence.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 51.Kim S.K., Kim J.H., Jeon S.S. Relationship between sleep quality and dizziness. PloS One. 2018;13 doi: 10.1371/journal.pone.0192705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Perogamvros L., Castelnovo A., Samson D. Failure of fear extinction in insomnia: an evolutionary perspective. Sleep Med Rev. 2020;51:101277. doi: 10.1016/j.smrv.2020.101277. [DOI] [PubMed] [Google Scholar]
- 53.Jansson M.L.S. The role of anxiety and depression in the development of insomnia: cross-sectional and prospective analyses. Psychol Health. 2006;21:383–397. [Google Scholar]
- 54.Lin R.M., Xie S.S., Yan Y.W. Intolerance of uncertainty and adolescent sleep quality: the mediating role of worry. Pers Indiv Differ. 2017;108:168–173. [Google Scholar]
- 55.Taylor D.J., Lichstein K.L., Durrence H.H. Insomnia as a health risk factor. Behav Sleep Med. 2003;1:227–247. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- 56.Harvey A.G. A transdiagnostic approach to treating sleep disturbance in psychiatric disorders. Cognit Behav Ther. 2009;38(Suppl 1):35–42. doi: 10.1080/16506070903033825. [DOI] [PubMed] [Google Scholar]
- 57.Benca R.M., Peterson M.J. Insomnia and depression. Sleep Med. 2008;9(Suppl 1):S3–S9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 58.Li Y.I., Starr L.R., Wray-Lake L. Insomnia mediates the longitudinal relationship between anxiety and depressive symptoms in a nationally representative sample of adolescents. Depress Anxiety. 2018;35:583–591. doi: 10.1002/da.22764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baglioni C., Battagliese G., Feige B. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 60.Lim G.Y., Tam W.W., Lu Y. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8:2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Putwain D.W. Test anxiety in UK schoolchildren: prevalence and demographic patterns. Br J Educ Psychol. 2007;77:579–593. doi: 10.1348/000709906X161704. [DOI] [PubMed] [Google Scholar]
- 62.Zhai K., Gao X., Wang G. The role of sleep quality in the psychological well-being of final year UndergraduateStudents in China. Int J Environ Res Publ Health. 2018;15 doi: 10.3390/ijerph15122881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang Y., Luo X., Paudel D. Effects of e-aid cognitive behavioural therapy for insomnia (eCBTI) to prevent the transition from episodic insomnia to persistent insomnia: study protocol for a randomised controlled trial. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-033457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Allgulander C. Psychoactive drug use in a general population sample, Sweden: correlates with perceived health, psychiatric diagnoses, and mortality in an automated record-linkage study. Am J Publ Health. 1989;79:1006–1010. doi: 10.2105/ajph.79.8.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang H.Z., Zhang X.L. The view summary of college Students'Sex ratio. Journal of Higher Education in Science & Technology. 2009;28:16–18. [Google Scholar]
- 66.NHCotPsRo C. Guideline for psychological crisis intervention during 2019-nCoV. http://wwwgovcn/xinwen/2020-01/27/content_5472433htm. 2020
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 2
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.