Structured Abstract
Introduction
The COVID-19 pandemic has spread globally and placed healthcare systems under substantial strain. Hip fracture patients represent a high-risk population for severe COVID-19 symptoms, as they are generally older with multiple medical comorbidities. There has been limited information available on the presenting characteristics and outcomes of COVID-positive patients with hip fractures who undergo surgical treatment.
Methods
This was a retrospective study of 10 patients ≥60 years of age with a hip fracture and COVID-19 who underwent surgical treatment in New York City during the COVID-19 outbreak from March 1, 2020 to May 22, 2020. Clinical characteristics and early postoperative outcomes were reported.
Results
Eight out of the 10 COVID-positive hip fracture patients in our series were asymptomatic on admission with no clinical signs or symptoms of COVID-19 infection. Only 2 patients presented with hypoxia. All 10 patients underwent surgery within 2 days of admission. Five out of the 10 patients – including the patients who presented with hypoxia – subsequently required supplemental oxygen postoperatively. Two patients had persistently elevated oxygen demands requiring prolonged administration of supplemental oxygen therapy beyond postoperative day 3. None of the patients were put on mechanical ventilation. One patient had a presumed venous thromboembolism postoperatively and subsequently died on postoperative day 19, likely due to respiratory failure. There were no other deaths in the early postoperative period. The average length of inpatient stay was 7.8 days.
Conclusions
Our findings suggest that hip fracture patients who present with asymptomatic or mild COVID-19 infection may have temporarily increased oxygen demands postoperatively, but they can safely undergo early surgical intervention after appropriate medical optimization.
Keywords: COVID-19, Coronavirus, Pandemic, Hip fracture, Mortality, Morbidity
1. Introduction
The first confirmed case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or COVID-19 infection in the United States was reported on January 31, 2020 in Washington state. Soon thereafter, the COVID-19 pandemic spread across the country and placed the United States healthcare system under substantial strain. Following the first confirmed case of COVID-19 in New York state on March 1, 2020, New York City quickly became the epicenter of the COVID-19 outbreak in the United States.
As the COVID-19 outbreak continues, there have been anecdotal and epidemiological evidence of patients avoiding hospitals and clinics despite requiring medical care, with significant decreases in hospital admissions for non-COVID-19 diagnoses.1 Potential delays in presentation for hip fractures are concerning given the morbidity and mortality associated with prolonged immobilization and delayed care.2, 3, 4 An additional concern is the potential independent effects of COVID-19 infection on early outcomes in the subgroup of hip fracture patients who are infected. The 1-year mortality rate in hip fracture patients has traditionally been estimated to be approximately 30%,5 while the 30-day mortality rate has been reported to be 5%–7%.4,6 Early reports from Wuhan, China and Italy, however, have showed significantly higher early mortality rates in patients with a hip fracture and COVID-19 infection.7, 8, 9
As of May 26, 2020, there have been no studies specifically examining outcomes in patients with hip fractures and COVID-19 infection who undergo surgical intervention in the United States. The purpose of this study was to report the clinical characteristics and early outcomes in a series of COVID-19-positive hip fracture patients who underwent surgery during the COVID-19 outbreak in New York City.
2. Methods
This research was approved by our internal Institutional Review Board. A retrospective cohort study was performed of patients ≥60 years of age who had positive COVID-19 diagnostic testing and underwent primary hip fracture surgery at our institution in New York City during the COVID-19 outbreak from March 1, 2020 to May 22, 2020. All patients at our institution who were hospitalized during the COVID-19 outbreak underwent COVID-19 diagnostic testing with a real-time reverse transcription polymerase chain reaction (RT-PCR) assay for the qualitative detection of nucleic acid from SARS-CoV-2 in nasopharyngeal swabs. COVID-positive hip fracture patients who were treated non-operatively were excluded, as our specific aim in this study was to examine outcomes after operative treatment of hip fractures. Other exclusion criteria included bilateral hip fractures, periprosthetic hip fractures, and revision hip surgery.
Patient demographics were collected, including age, gender, and medical comorbidities. Evidence of COVID-19 infection was recorded, including clinical signs and symptoms, as well as laboratory testing and chest radiograph findings. The administration of any COVID-19-specific medical treatments were noted. The mechanism of injury, fracture type, and surgery performed were reviewed for all patients. Fractures were classified according to the AO/OTA classification. All patients were allowed to weight bear as tolerated postoperatively. Perioperative variables included laboratory testing on admission, time to surgery, and type of anesthesia. Laboratory testing included white blood cell (WBC) count, hemoglobin (Hgb), hematocrit (Hct), platelets, sodium, potassium, creatinine, prothrombin time (PT), international normalized ratio (INR), partial thromboplastin time (PTT), and inflammatory markers. Inflammatory markers included procalcitonin, C reactive protein, D-dimer, ferritin, and lactate dehydrogenase (LDH).
Outcomes of interest were oxygen demand on postoperative days 1 through 3, inpatient complications, length of stay (LOS), readmission, and death. Inpatient complications included blood transfusion, venous thromboembolism (VTE), cardiac complication, respiratory complication, acute kidney injury (AKI), and surgical site complication. Respiratory complications included hypoxia requiring prolonged administration of supplemental oxygen therapy beyond the third postoperative day, respiratory failure, and mechanical ventilation. AKI was defined as an increase in creatinine of 0.3 mg/dL or more in 48 h.
3. Results
Ten patients met our selection criteria and were included in this study. The clinical characteristics and postoperative complications are outlined in Table 1. There were 8 females and 2 males, ranging from 67 to 90 years of age. All 10 patients sustained hip fractures after a low-velocity fall from standing height. Seven of the patients had a positive COVID-19 test upon presentation to the hospital, whereas the remaining 3 patients (Cases 1, 2, and 9) had a nosocomial infection with a positive COVID-19 test within 5, 8, and 9 days of admission, respectively. None of the patients presented with symptoms of fever, chills, cough, sore throat, dyspnea, chest pain, or fatigue. Only 1 patient (Case 4) presented with obvious signs of COVID-19 infection on presentation, with hypoxia and an oxygen saturation of 89% on room air. Another patient (Case 2) presented with mild hypoxia and an oxygen saturation of 94% on room air. The remaining 8 patients did not exhibit any signs or symptoms of COVID-19 infection on admission.
Table 1.
Clinical characteristics and outcomes in 10 patients with COVID-19 who underwent hip fracture surgery.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Clinical characteristics | ||||||||||
| Age (years), sex | 83 F | 82 F | 90 F | 88 F | 73 M | 81 F | 80 F | 78 F | 75 F | 67 M |
| Comorbidities | Asthma, COPD, OSA, HTN, HLD, breast cancer, CVA, hypothyroidism, Sjogren's disease | HTN, HLD, IBS | HTN, CHF, DM | HTN, DM, pancreatic cancer, renal cancer, dementia | HLD, BPH, OCD | HTN, atrial fibrillation, hypothyroidism, hepatitis C, dementia | Cognitive disorder | HTN, TIA, hypothyroidism | HTN, CAD, DM | Asthma, kidney stones, BPH |
| Time to surgery (days) | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 1 | 1 |
| Fracture type | 31A2.2 | 31B1.3 | 31A1.2 | 31A1.3 | 31A2.1 | 31A2.3 | 31A2.1 | 31B1.3 | 31A1.3 | 31B1.2 |
| Surgery performed | CMN | Hemi | CMN | CMN | CMN | CMN | CMN | THA | CMN | FNS |
| Type of anesthesia | General | Neuraxial | Neuraxial | General | Neuraxial | Neuraxial | General | Neuraxial | Neuraxial | General |
| Respiratory symptoms on admission | ||||||||||
| Fever | No | No | No | No | No | No | No | No | No | No |
| Chills | No | No | No | No | No | No | No | No | No | No |
| Cough | No | No | No | No | No | No | No | No | No | No |
| Sore throat | No | No | No | No | No | No | No | No | No | No |
| Dyspnea | No | No | No | No | No | No | No | No | No | No |
| Chest pain | No | No | No | No | No | No | No | No | No | No |
| Fatigue | No | No | No | No | No | No | No | No | No | No |
| SpO2 | 100% on RA | 94% on RA | 97% on RA | 89% on RA | 95% on RA | 97% on RA | 95% on RA | 98% on RA | 98% on RA | 98% on RA |
| Laboratory test values on admission | ||||||||||
| WBC (4.5–11.0 K/μL) | 7.7 | 9.5 | 8.7 | 12.0 | 8.4 | 8.5 | 19.5 | 17.7 | 17.0 | 13.1 |
| Hgb/Hct (13.9–16.3 g/dL)/(42–52%) | 11.5/35 | 14.4/43 | 13.0/39 | 10.5/30 | 7.7/23 | 15.3/46 | 12.3/35 | 12.7/39 | 10.5/32 | 12.9/38.5 |
| Platelets (150–450 K/μL) | 170 | 302 | 201 | 204 | 236 | 225 | 223 | 230 | 624 | 164 |
| Creatinine (0.7–1.3 mg/dL) | 0.50 | 0.87 | 0.98 | 0.64 | 1.51 | 0.58 | 0.70 | 0.56 | 1.54 | 1.03 |
| Sodium (135–145 mmol/L) | 138 | 139 | 129 | 136 | 135 | 136 | 136 | 130 | 128 | 139 |
| Potassium (3.5–5.2 mmol/L) | 3.3 | 5.7 | 4.7 | 3.6 | 4.8 | 4.4 | 4.0 | 4.1 | 4.5 | 3.9 |
| PT/INR (12.0–14.2 s)/(0.9–1.1) | 13.6/1.1 | 12.7/1.0 | 13.7/1.1 | 15.0/1.2 | 14.1/1.1 | 15.4/1.3 | 13.8/1.1 | 13.9/1.1 | 14.2/1.1 | 13.8/1.1 |
| PTT (24.6–34.7 s) | 23.2 | 24.5 | 27.3 | 29.8 | 29.2 | 25.6 | 30.0 | 32.4 | 26.5 | 28.8 |
| Inflammatory markers | ||||||||||
| Procalcitonin (<0.15 ng/mL) | 0.09 | 0.09 | – | 0.04 | 0.14 | 0.07 | 0.09 | – | 0.48 | – |
| C reactive protein (<5.1 mg/L) | 194.1 | 32.1 | – | 30.7 | 144.8 | 16.2 | 111.3 | – | – | – |
| D-dimer (<0.5 μg/mL) | 5.85 | 2.88 | – | 8.99 | 6.08 | 4.91 | 8.64 | – | – | – |
| Ferritin (15–150 ng/mL) | 223 | 1220 | – | 13 | 801 | 1893 | 350 | – | – | – |
| LDH (100–220 U/L) | 284 | 228 | – | 357 | 357 | 311 | 453 | – | – | – |
| Chest radiograph on admission | Unremarkable | Unremarkable | Unremarkable | Unremarkable | Multifocal/atypical pneumonia | Unremarkable | Unremarkable | Unremarkable | Unremarkable | Unremarkable |
| COVID-19 medical treatment | Yes (AZM, HCQ) | No | No | Yes (HCQ) | Yes (AZM, HCQ) | No | Yes (AZM, HCQ) | No | No | No |
| Postoperative outcomes | ||||||||||
| SpO2 on POD1 | 99% on RA | 98% on 2L NC | 99% on RA | 96% on 4L NC | 96% on 8L Venturi mask | 97% on RA | 98% on 4L NC | 98% on 2L NC | 95% on RA | 97% on RA |
| SpO2 on POD2 | 98% on RA | 95% on RA | 97% on RA | 94% on 2L NC | 97% on 4L NC | 94% on RA | 94% on 2L NC | 95% on RA | 98% on RA | 98% on RA |
| SpO2 on POD3 | 93% on RA | 99% on RA | 96% on RA | 98% on RA | 96% on 6L NC | ---(discharged on POD2) | 90% on 2L NC | 96% on RA | 96% on RA | 97% on RA |
| Blood transfusion | Yes | No | No | Yes | Yes | No | No | Yes | No | No |
| VTE | Yes | No | No | No | No | No | No | No | No | No |
| Cardiac complication | No | No | No | No | No | No | No | No | No | No |
| Respiratory complication | Yes (respiratory failure) | No | No | No | Yes (prolonged hypoxia requiring supplemental O2) | No | Yes (prolonged hypoxia requiring supplemental O2) | No | No | No |
| AKI | No | No | Yes | No | No | No | No | No | No | No |
| Surgical site complication | No | No | No | No | No | No | No | No | No | No |
| Mortality | Yes (POD 19) | No | No | No | No | No | No | No | No | No |
| LOS (days) | – | 4 | 7 | 20 | 7 | 4 | 9 | 6 | 5 | a |
| Disposition | – | Acute rehab | SAR | SAR | SAR | SAR | SAR | Home | SAR | a |
| Readmission | – | Yes | Yes | No | No | No | No | No | No | – |
| Reason for readmission | – | Symptomatic COVID-19 | Unknown (OSH records unavailable) | – | – | – | – | – | – | – |
| Time of readmission | – | POD 9 | POD 8 | – | – | – | – | – | – | – |
COPD: chronic obstructive pulmonary disease; OSA: obstructive sleep apnea; HTN: hypertension; HLD: hyperlipidemia; CVA: cerebrovascular accident; IBS: irritable bowel syndrome; CHF: congestive heart failure; DM: diabetes mellitus; BPH: benign prostatic hyperplasia; OCD: obsessive compulsive disorder; TIA: transient ischemic attack; CAD: coronary artery disease; CMN: cephalomedullary nail; Hemi: hip hemiarthroplasty; THA: total hip arthroplasty; FNS: Femoral Neck System; RA: room air; AZM: azithromycin; HCQ: hydroxychloroquine; NC: nasal cannula; POD: postoperative day; SAR: subacute rehab; OSH: outside hospital.
Remains hospitalized – medically cleared for discharge but awaiting insurance authorization for admission to a rehabilitation facility.
Laboratory test values on admission were notable for leukocytosis in 5 patients, significant anemia with Hgb<8 g/dL in 1 patient, and elevated platelet count in 1 patient. Two patients presented with elevated creatinine. Hyponatremia and hyperkalemia were noted in 3 patients and 1 patient, respectively. PT and INR were mildly elevated in 2 patients and none of the patients had an abnormal PTT value. Of the 7 patients who received testing for 1 or more of the inflammatory markers of interest, all had at least 1 elevated inflammatory marker. Only 1 patient (Case 5) had an abnormal chest radiograph on admission that demonstrated evidence of multifocal or atypical pneumonia. Four patients (Cases 1, 4, 5, and 7) received COVID-19-specific medical therapy with hydroxychloroquine and/or azithromycin.
All patients underwent surgery within 2 days of admission. There were 7 patients who underwent cephalomedullary nailing for 31A-type fractures, 2 patients who underwent hemiarthroplasty or total hip arthroplasty (THA) for 31B1.3 fractures, and 1 patient who underwent internal fixation with the Femoral Neck System (DePuy Synthes, Warsaw, Indiana) for a 31B1.2 fracture. Four patients received general anesthesia and 6 patients received neuraxial anesthesia with a single-shot spinal anesthetic. There were no intraoperative complications.
Postoperatively, 5 out of the 10 patients required supplemental oxygen. Two of these patients (Cases 2 and 8) were successfully weaned off 2 L per minute (L/min) nasal cannula after postoperative day 1. Another patient (Case 4) was weaned off nasal cannula after postoperative day 2. The other 2 patients (Cases 5, and 7) had persistently elevated oxygen demands requiring prolonged administration of supplemental oxygen beyond postoperative day 3. None of the patients were put on mechanical ventilation.
Four out of the 10 patients received a perioperative blood transfusion. One patient (Case 1) was treated for a presumed VTE during hospitalization, and 1 patient (Case 3) had a postoperative AKI. There were no in-hospital cardiac complications or surgical site complications. One patient (Case 1) died during hospitalization on postoperative day 19 after being found unresponsive, likely due to respiratory failure. One patient (Case 10) remained hospitalized at the time of reporting; he was medically cleared for discharge to a rehabilitation facility, but awaiting insurance authorization. Four of the remaining 8 patients had a LOS ≥7 days, with the average LOS among these patients being 7.8 days. Seven patients were discharged to rehabilitation facilities and 1 patient was discharged home with services. Lastly, there were 2 early readmissions. One patient (Case 2) was readmitted at our institution for symptomatic COVID-19 infection. The other patient (Case 3) was readmitted at an outside hospital and we were unable to access the outside records to assess the reason for readmission.
4. Discussion
In this study, we presented the clinical characteristics and early outcomes from a cohort of 10 COVID-positive patients who underwent hip fracture surgery at our institution during the COVID-19 outbreak in New York City. All of the patients underwent surgery within 2 days of admission. Eight out of the 10 patients in our series were asymptomatic on admission with no clinical signs or symptoms of COVID-19 infection. Only 2 patients presented with hypoxia. However, 5 out of the 10 patients – including the patients who presented with hypoxia – subsequently required supplemental oxygen postoperatively. Two patients were successfully weaned off supplemental oxygen by postoperative day 2 and 1 patient was weaned off supplemental oxygen by postoperative day 3. The remaining 2 patients, however, continued to have increased oxygen demands requiring prolonged supplemental oxygen therapy beyond postoperative day 3. Neither of these patients ultimately required mechanical ventilation. Only 1 patient in our series had a presumed VTE postoperatively and this patient subsequently died on postoperative day 19, likely secondary to respiratory failure. There were no other deaths in the early postoperative period in this series of COVID-positive hip fracture patients who underwent urgent surgical intervention at our institution.
COVID-19 symptoms vary substantially among patients, ranging from no symptoms to respiratory failure.10 Mild presentations may include flu-like symptoms, such as cough, muscle pain, sore throat, and fever. However, more severe pulmonary symptoms can also occur, with patients such as the elderly and those with existing comorbidities being at particularly high risk for dyspnea, interstitial pneumonia, acute respiratory distress syndrome (ARDS), and multi-organ dysfunction. Hip fracture patients represent a high-risk population, as they are generally older with multiple medical comorbidities. Extensive literature has consistently demonstrated the benefits of early hip fracture surgery for elderly patients, which include reducing bed rest, promoting early mobilization, controlling pain, improving function, and reducing mortality.3,4 However, the high risk associated with severe respiratory dysfunction and pneumonia secondary to COVID-19 infection may represent a contraindication to urgent hip fracture surgery in COVID-positive patients. Furthermore, in patients who proceed to hip fracture surgery, pulmonary complications are known to be a significant contributor to postoperative morbidity, with the incidence of these complications estimated to be approximately 4%–9%.11,12
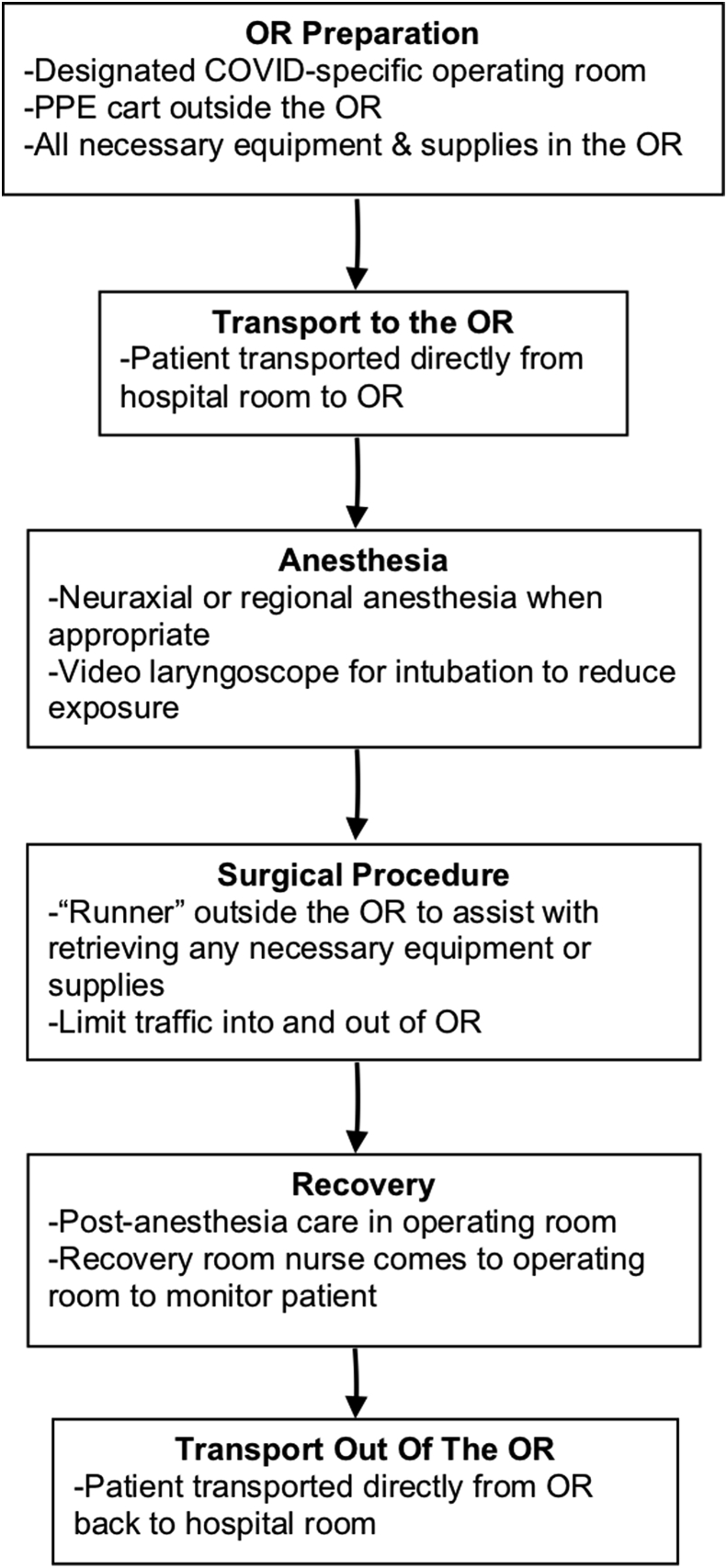
At our institution, all patients who underwent surgical procedures during the COVID-19 outbreak were required to have COVID-19 diagnostic testing within 48 h of the procedure. The operating room protocols for COVID-positive patients at our institution are outlined in Fig. 1. COVID-positive patients were transported directly from their hospital room to a designated COVID-specific operating room without passing through the usual preoperative holding area. Only essential staff were permitted in the operating room, all of whom had appropriate personal protective equipment (PPE), including N95 respirator masks, face shields, gowns, and gloves. Anesthesiologists utilized neuraxial or regional anesthesia when appropriate, and video laryngoscopes to assist with endotracheal intubations to reduce exposure. A designated “runner” outside the operating room was available to retrieve any required equipment or supplies throughout the procedure, in order to limit incoming and outgoing traffic in the operating room. After completion of the surgical procedure, COVID-positive patients remained in the operating room for post-anesthesia care and recovery, with the recovery room nurse coming into the operating room to provide care. After patients had satisfactorily completed their post-anesthesia care, they were transported directly from the operating room back to their hospital room.
Fig. 1.
Operating room protocols for COVID-positive patients at our institution.
There has been limited information available on the presenting characteristics and outcomes of COVID-positive patients with hip fractures. Mi et al. published one of the first reports on the characteristics and early prognosis of patients with a fracture and COVID-19 infection in China.7 In their series of 10 patients, 6 had sustained hip fractures and only 3 underwent surgery. These 3 patients did not present with any severe symptoms on admission or have any clear evidence of COVID-19 infection on CT scans, and thus, proceeded with surgical intervention. All 3 patients were observed to have fever and cough postoperatively, and 2 of the patients had symptoms of dyspnea. One of the 3 patients died on postoperative day 11, while the other 2 patients remained in the hospital for further treatment.
Another study by Catellani et al. reported on a series of 16 COVID-positive patients with proximal femoral fractures in northern Italy, of which 13 underwent surgical treatment.8 All of the patients in this series reported symptoms of fever and dyspnea prior to admission, and had signs of oxygen desaturation on room air upon presentation to the emergency room. The majority of patients in this study demonstrated significant improvements in oxygen saturation and respiratory function following surgery. However, 4 out of the 13 patients (30.8%) died with the first week after surgery. High early mortality rates in COVID-positive hip fracture patients were also reported in another study in Italy by Maniscalco et al.13 In this cohort, 32 COVID-positive hip patients were treated surgically, and there was a 43.8% (14/32) mortality rate within 21 days. These early reports from China and Italy suggested a higher rate of mortality in the early postoperative period for patients with a hip fracture and COVID-19 infection.
Similar findings have also been reported in a more recent study in Spain. A multicenter, observational study from 13 major hospitals in Spain examined the early mortality rate in 136 hip fracture patients who were treated surgically or nonoperatively during the COVID-19 pandemic.9 Of the 62 patients who were tested for COVID-19 in their cohort, 23 patients had positive test results. The early mortality rate in this group of COVID-positive hip fracture patients was approximately 3 times higher than that for COVID-negative hip fracture patients. This was consistent with the high early mortality rates noted in the earlier reports from China and Italy.
The findings from our cohort of 10 COVID-positive hip fracture patients in New York City who underwent surgical treatment differed from the above mentioned studies in China and Europe. The early mortality rate in this series was only 10%. However, it is important to note that nearly all of our COVID-positive patients were asymptomatic or had only mild symptoms on presentation. The 3 hip fractures patients who underwent surgery in Mi et al.‘s study similarly had no severe symptoms on admission, but the 13 patients in Catellani et al.‘s study all presented with evidence of symptomatic COVID-19 infection.7,8 This difference in the presentation of COVID-19 symptoms on admission likely contributed to the observed discrepancy in early mortality rates between our patient cohort and those of prior studies.
In our study, nearly half of the patients had an inpatient stay ≥7 days, and the average LOS among discharged patients was 7.8 days. This is slightly longer than the average LOS after hip fracture surgery reported in past studies, which has ranged between 5 and 6 days.14,15 Three of the 4 patients in our cohort who had a LOS ≥7 days had increased oxygen demands postoperatively and required prolonged administration of supplemental oxygen therapy beyond the second postoperative day. The fourth patient had a postoperative AKI that required treatment with intravenous fluids over several days. These postoperative complications likely contributed to the longer inpatient stay.
This study has several limitations. First, we had a small sample size of COVID-19-positive patients who underwent hip fracture surgery, despite being an institution in the epicenter of the COVID-19 outbreak in the United States. However, this sample size was comparable to existing case series in the literature. Second, we limited our inclusion criteria to patients who underwent surgical intervention. This excluded patients with hip fractures and COVID-19 infection who were deemed to be unsuitable candidates for surgery for reasons such as medical instability from existing comorbidities or severe COVID-19 infection. Therefore, our findings should not be extrapolated to hip fracture patients with severe presentations of COVID-19 infection. Third, the short follow-up period may have resulted in an underestimation of the mortality rate. Longer term follow-up will be needed to assess morbidity and mortality beyond the early postoperative period. Lastly, our study population was limited to only patients within the New York metropolitan area, thereby potentially limiting generalizability to patient populations in other geographic regions with different baseline demographics and comorbidity profiles.
In conclusion, this study described the clinical characteristics and early outcomes after hip fracture surgery in patients who presented with asymptomatic or mild COVID-19 infection in New York City. Despite the absence of clinical signs and symptoms of COVID-19 infection in nearly all of these patients on admission, half of these patients subsequently had increased oxygen demand postoperatively requiring supplemental oxygen therapy. However, more than half of these patients who had increased oxygen demand postoperatively were successfully weaned off oxygen therapy within 3 days after surgery. Furthermore, the mortality rate in the early postoperative period in our series was only 10%, which is in contrast to the higher mortality rates reported from studies in China and Europe. Our findings suggest that hip fracture patients who present with asymptomatic or mild COVID-19 infection may have temporarily increased oxygen demands postoperatively, but they can safely undergo early surgical intervention after appropriate medical optimization.
Institutional Review Board approval
IRB approval was obtained for the submitted work at our institution.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
References
- 1.De Filippo O., D'Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020 Apr 28 doi: 10.1056/NEJMc2009166. Epub ahead of print, NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vidal E.I.O., Moreira-Filho D.C., Pinheiro R.S. Delay from fracture to hospital admission: a new risk factor for hip fracture mortality? Osteoporos Int. 2012;23(12):2847–2853. doi: 10.1007/s00198-012-1917-x. [DOI] [PubMed] [Google Scholar]
- 3.Ryan D.J., Yoshihara H., Yoneoka D., Egol K.A., Zuckerman J.D. Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma. 2015;29(8):343–348. doi: 10.1097/BOT.0000000000000313. [DOI] [PubMed] [Google Scholar]
- 4.Pincus D., Ravi B., Wasserstein D. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. J Am Med Assoc. 2017;318(20):1994–2003. doi: 10.1001/jama.2017.17606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moran C.G., Wenn R.T., Sikand M., Taylor A.M. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 6.Beaupre L.A., Khong H., Smith C. The impact of time to surgery after hip fracture on mortality at 30- and 90-days: does a single benchmark apply to all? Injury. 2019;50(4):950–955. doi: 10.1016/j.injury.2019.03.031. [DOI] [PubMed] [Google Scholar]
- 7.Mi B., Chen L., Xiong Y., Xue H., Zhou W., Liu G. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am. 2020;102(9):750–758. doi: 10.2106/JBJS.20.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Catellani F., Coscione A., D'Ambrosi R., Usai L., Roscitano C., Fiorentino G. Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in northern Italy. J Bone Joint Surg Am. 2020 Apr 28 doi: 10.2106/JBJS.20.00617. Epub ahead of print, JBJS.20.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munoz Vives J.M., Jornet-Gibert M., Camara-Cabrera J. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID observational study. J Bone Joint Surg Am. 2020 May 6 doi: 10.2106/JBJS.20.00686. Epub ahead of print, JBJS.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pascarella G., Strumia A., Piliego C. COVID-19 diagnosis and management: a comprehensive review. J Intern Med. 2020 Apr 29 doi: 10.1111/joim.13091. Epub ahead of print, joim.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawrence V.A., Hilsenbeck S.G., Noveck H., Poses R.M., Carson J.L. Medical complications and outcomes after hip fracture repair. Arch Intern Med. 2002;162(18):2053–2057. doi: 10.1001/archinte.162.18.2053. [DOI] [PubMed] [Google Scholar]
- 12.Lv H., Yin P., Long A. Clinical characteristics and risk factors of postoperative pneumonia after hip fracture surgery: a propective cohort study. Osteoporos Int. 2016;27(10):3001–3009. doi: 10.1007/s00198-016-3624-5. [DOI] [PubMed] [Google Scholar]
- 13.Maniscalco P., Poggiali E., Quattrini F. Proximal femur fractures in COVID-19 emergency: the experience of two orthopedics and traumatology departments in the first eight weeks of the Italian epidemic. Acta Biomed. 2020;91(2):89–96. doi: 10.23750/abm.v91i2.9636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khoshbin A., Atrey A., Chaudhry H. Mortality rate of geriatric acetabular fractures is high compared to hip fractures. A matched cohort study. J Orthop Trauma. 2020 Mar 10 doi: 10.1097/BOT.0000000000001758. Epub ahead of print, BOT.0000000000001758. [DOI] [PubMed] [Google Scholar]
- 15.Lowe J., Mitchell S.M., Agarwal S., Jones C.B. Traumatic hip fracture and primary elective total hip patients are not the same: a comparison of comorbidity burden, hospital course, postoperative complications and cost of care analysis. J Orthop Trauma. 2020 May 4 doi: 10.1097/BOT.0000000000001800. Epub ahead of print, BOT.0000000000001800. [DOI] [PubMed] [Google Scholar]