Abstract
Background
COVID-19 pandemic effects are still being elucidated. Stay-at-home orders and social distancing compounded with COVID-19 concerns have caused significant disruptions in daily life. One notable effect of these variables may be a change in the number of emergency department (ED) visits. This study aims to investigate the effects of COVID-19 on ED visits, and possible reasons for changes.
Methods
Retrospective analysis using CDC data for ED visits and percentage of visits for COVID-19-Like Illness (CLI) and Influenza-Like Illness (ILI). Google Trends was used to assess COVID-19 public awareness. Motor vehicle collision (MVC) data was collected from cities, which reported current data. A descriptive statistical analysis and two-sample t-test was performed on ED visit data to assess for significance and a descriptive analysis was conducted to assess COVID-19's impact on MVCs.
Results
The mean number of ED visits per week for the last four weeks of available data during the pandemic was significantly less than the four weeks prior to COVID-19 pandemic (p = 0.008). The ED visit decrease per week varied by region, with Region 1 having the greatest decrease (45%). MVCs decreased substantially across all cities studied, with New York City and Baton Rouge experiencing the greatest decrease (66%) during the pandemic.
Conclusion
A number of factors have likely contributed to the substantial decrease in ED visits observed in this study. In light of these findings, it is important to raise patient awareness regarding acute conditions that are deadlier than COVID-19 and require immediate medical intervention to ensure recovery.
Keywords: COVID-19 pandemic, Motor vehicle collisions, Emergency department visits, Acute medical conditions, Medical emergencies
1. Introduction
Since being declared a pandemic by the World Health Organization on March 11, 2020 coronavirus disease (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread rapidly causing significant suffering worldwide [1]. In the United States (US) alone there were 895,766 reported cases and 50,439 reported deaths as of April 26, 2020 [2]. In addition to the physical effects of COVID-19, the disease has also challenged the psychological resilience of many individuals and altered behavioral patterns. For instance, a study, which surveyed the Chinese public (from January 31, 2020 to February 2, 2020), found that 54% of respondents rated the psychological impact of the COVID-19 pandemic as moderate or severe. Another study which surveyed the German public (from March 19, 2020 March 23, 2020) found that 28.2% of respondents were afraid of being infected by COVID-19 [3,4]. The fear that the public is experiencing due to COVID-19 is likely exacerbated by measures causing social isolation including quarantines, stay-at-home orders, travel restrictions and closures of non-essential businesses [5,6]. As people practice social distancing, self-isolation, and begin working remotely, the potential for injuries such as trauma due to motor vehicle collisions (MVCs) may decline considerably.
Given the potential reduction in injury, and the current climate of COVID-19 related fears, patients may be less likely to utilize hospital emergency department (ED) services. More worryingly, reports are surfacing that indicate patients may be ignoring signs of medical conditions that would normally cause them to seek ED services. For instance, health systems in Spain have reported treating 40% fewer patients with ST-segment elevation myocardial infarctions (STEMIs) during the COVID-19 pandemic (from March 16, 2020 to March 22, 2020) and EDs in Massachusetts were found to treat 44–45% fewer cases of depression or anxiety during March 2020 [7,8]. Thus, the primary objective of this study is to investigate the impact that COVID-19 may have had on ED visits nationwide. Additionally, this study aims to discuss potential reasons for any changes in the number of ED visits during the COVID-19 pandemic.
2. Methods
2.1. Data source and population
This retrospective analysis was performed utilizing data collected from the National Center for Immunization and Respiratory Diseases (NCIRD) division of the Centers for Disease Control and Prevention (CDC). Data was gathered from NCIRD regarding total ED visits, percentage of visits for COVID-19-Like Illness (CLI), and percentage of visits for Influenza-Like Illness (ILI) from the week of September 29, 2019 to the week of April 5, 2020. This data range from the week of September 29, 2019 to the week of April 5, 2020 was selected since it encompassed all available data at the time of writing for the topics selected. The data set included information from 3415 reporting facilities across 10 regions (Table 1 ). Data was also gathered from Google Trends for the past 12 months regarding search interest in the US, (Puerto Rico (PR) and Guam (GU) for the search terms coronavirus and COVID-19 to assess public awareness. Next, data regarding MVCs was collected from cities (Austin, Baton Rouge, Chicago, Cincinnati, Montgomery, New York) which reported data in alignment with the last four weeks of available COVID-19 ED data at the time of writing (MVC data was obtained from the week of March 15, 2020 to the week of April 5, 2020). MVC data was also gathered from the same cities for the same time period one year prior (from the week of March 15, 2019 to the week of April 5, 2019).
Table 1.
Region number and corresponding states and territories.
| Region number | States and territories |
|---|---|
| Region 1 | CT, ME, MA, NH, RI, VT |
| Region 2 | NJ, NY, PR |
| Region 3 | DE, DC, MD, PA, VA, WV |
| Region 4 | AL, FL, GA, KY, MS, NC, SC, TN |
| Region 5 | IL, IN, MI, MN, OH, WI |
| Region 6 | AR, LA, NM, OK, TX |
| Region 7 | IA, KS, MO, NE |
| Region 8 | CO, MT, ND, SD, UT, WY |
| Region 9 | AZ, CA, GU, HI, NV |
| Region 10 | AK, ID, OR, WA |
2.2. Data analysis and statistical methods
Descriptive statistical analysis was performed to evaluate the temporal relationship between the total number of ED visits and the percent of total visits for CLI or ILI from the week of September 29, 2019 to the week of April 5, 2020. A two-sample t-test was then used to assess if any significant differences existed between the mean number of ED visits for a four week period prior to increased COVID-19 awareness (week of December 15, 2019 to the week of January 5, 2020) to after increased awareness (the week of March 15, 2020 to the week of April 5, 2020). COVID-19 awareness was derived from Google search trends in the US, PR and GU. The percentage decrease in ED visits was calculated by region using the mean number of ED visits from the same four-week period prior to increased COVID-19 awareness and the mean number of ED visits for the same four weeks after increased awareness. The last four-week data set was the latest available data at the time of writing (from the week of March 15, 2020 to the week of April 5, 2020). Descriptive analysis of MVC data was conducted to assess if COVID-19 has impacted MVC rates. Finally, the percentage decrease in MVCs was calculated using data from each city during the weeks of March 15, 2020 to April 5, 2020 and data for the same time period one year prior. Minitab statistical software version 19.2020.1 was utilized for all statistical analysis. Statistical significance was defined a p < 0.05.
3. Results
3.1. ED visit trends
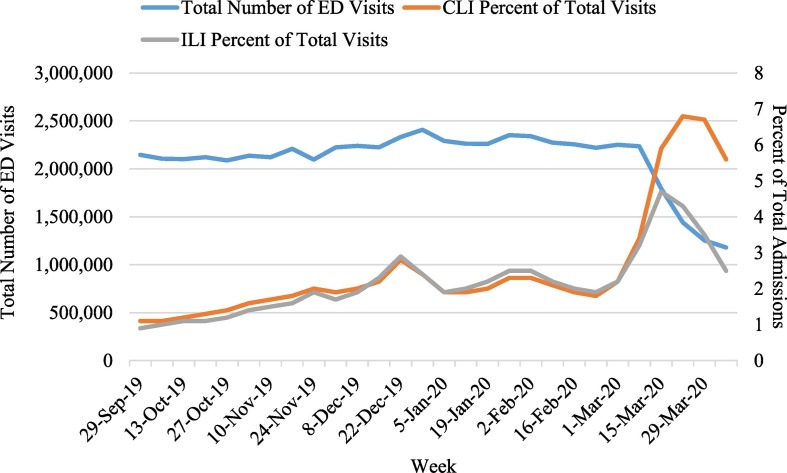
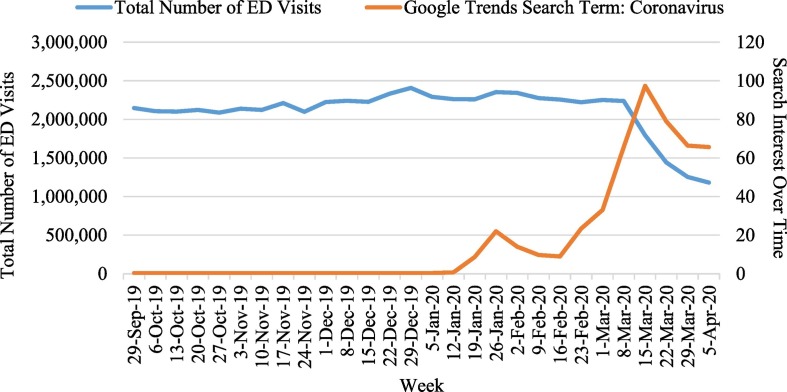
The total number of ED visits per week was found be relatively stable from the week of September 29, 2019 until the week of March 8, 2020. During this time the mean number of ED visits across all regions was 2,221,351 visits per week (SD = 89,767). Starting around the week of February 23, 2020 the percentage of visits for ILI, and the percentage of visits for CLI began to increase reaching their peaks during the week of March 15, 2020 and during the week of March 22, 2020 respectively (Fig. 1 ). The total number of ED visits per week began to decline during the week of March 8, 2020 reaching a nadir during the last week of available data (the week of April 5, 2020). This drop in the total number of ED visits per week was preceded by an uptrend in Google search interest, which initially began during the week of January 12, 2020 and reached a peak during the week of March 15, 2020 (Fig. 2 ).
Fig. 1.
Total number of ED visits per week and percent of total visits for COVID-19-Like Illness (CLI) or Influenza-Like Illness (ILI) from the week of September 29, 2019 to the week of April 5, 2020.
Fig. 2.
Total number of ED visits per week and Google trends search interest over time for the term coronavirus (A value of 100 is the peak popularity for the term. A value of 50 means that the term is half as popular. A score of 0 means there is not enough data for the term).
3.2. Change in ED visits in response to COVID-19
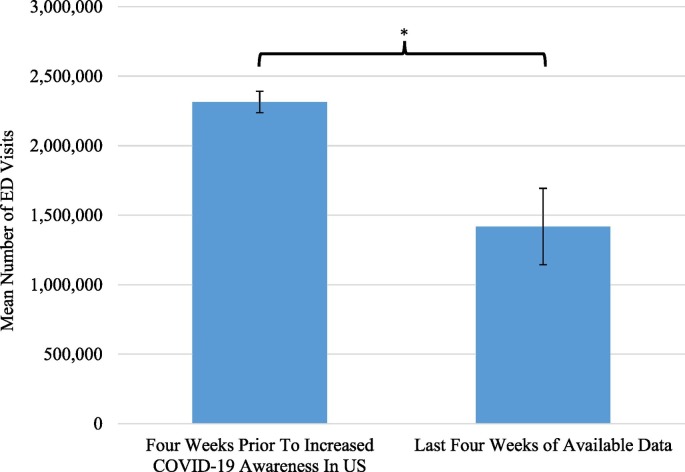
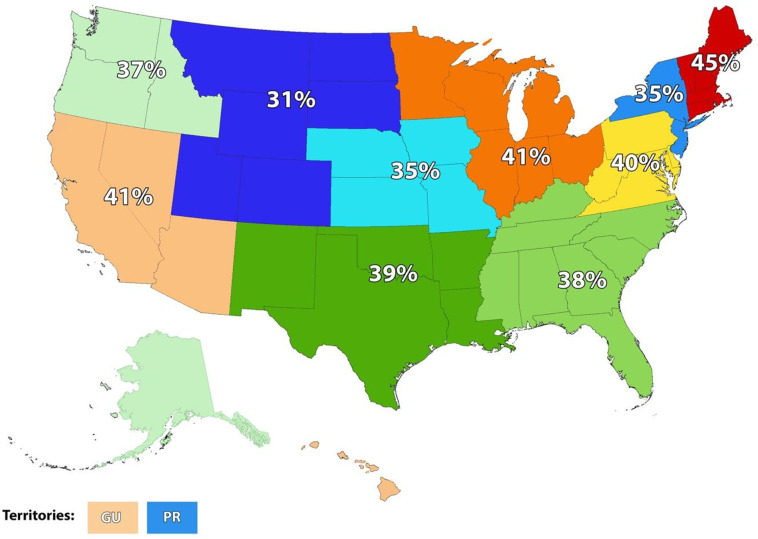
The mean number of ED visits per week for the last four weeks of available data (M = 1,417,565, SD = 274,469) during the pandemic (the week of March 15, 2020 to the week of April 5, 2020) was significantly less than a period of four weeks prior to COVID-19 pandemic (M = 2,314,485, SD = 76,401) (week of December 15, 2019 to the week of January 5, 2020). The data was again derived from Google search trends in the US, PR and GU); t (3) = 6.30, p = 0.008 (Fig. 3 ). The percentage decrease in the mean number of ED visits per week also varied by region with Region 1 (CT, ME, MA, NH, RI, VT) having the greatest decrease (45%) and Region 8 (CO, MT, ND, SD, UT, WY) having the smallest decrease (31%) (Fig. 4 ).
Fig. 3.
Mean number of ED visits per week for a four week period prior to increased COVID-19 awareness in the US, PR and GU (from the week of December 15, 2019 to the week of January 5, 2020: derived from Google search trends in the US, PR and GU) and the mean number of ED visits for the last four weeks of available data at the time of writing (from the week of March 15, 2020 to the week of April 5, 2020). The mean number of ED visits significantly [t(3) = 6.30; *p = 0.008] decreased during the current outbreak. Error bars represent standard deviation.
Fig. 4.
Represents the percentage decrease in the mean number of ED visits per week by region using data from a four week period prior to increased COVID-19 awareness in the US, PR and GU (from the week of December 15, 2019 to the week of January 5, 2020: derived from Google search trends in the US, PR and GU) and the last four weeks ED visit data available at the time of writing (from the week of March 15, 2020 to the week of April 5, 2020). Region 1 (CT, ME, MA, NH, RI, VT), Region 2 (NJ, NY, PR), Region 3 (DE, DC, MD, PA, VA, WV), Region 4 (AL, FL, GA, KY, MS, NC, SC, TN), Region 5 (IL, IN, MI, MN, OH, WI), Region 6 (AR, LA, NM, OK, TX), Region 7 (IA, KS, MO, NE), Region 8 (CO, MT, ND, SD, UT, WY), Region 9 (AZ, CA, GU, HI, NV), Region 10 (AK, ID, OR, WA).
3.3. MVCs during the COVID-19 pandemic
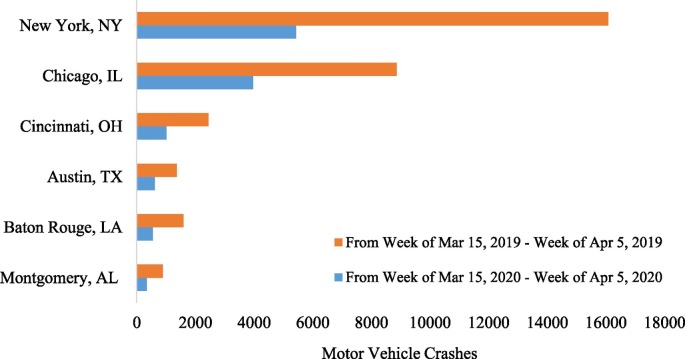
New York City (NYC) and Baton Rouge, LA experienced the greatest decrease in MVCs (66%) during the pandemic (from the week of March 15, 2020 to the week of April 5, 2020) compared to the same time period one year before (Fig. 5 ). Montgomery, AL experienced a 62% decrease in MVCs, Cincinnati, OH experienced a 59% decrease in MVCs, and both Chicago, IL and Austin, TX experienced a 55% decrease in MVCs during the pandemic (from the week of March 15, 2020 to the week of April 5, 2020) compared to the same time period one year before.
Fig. 5.
The comparison of motor vehicle crashes by city from before (from the week of March 15, 2019 – the week of April 5, 2019) and during the COVID-19 outbreak (from the week of March 15, 2020 – the week of April 5, 2020).
4. Discussion
The total number of ED visits per week across all study regions began to decline precipitously during the week of March 8, 2020 following months of relative stability. This drop in the total number of ED visits per week was also preceded by an increased percentage of visits for ILI and CLI beginning around the week of February 23, 2020, which correlated with increased public awareness of COVID-19 as indicated by Google search interest. The increased percentage of visits for ILI and CLI can likely be explained by a number of factors including a substantial increase in actual COVID-19 cases in the US during March 2020, revisions made to COVID-19 testing criteria allowing for wider testing starting on March 4, 2020, and increased public concern regarding COVID-19 like symptoms [9,10].
Interestingly, the drop in ED visits per week during the week of March 8, 2020 coincides with both the World Health Organization declaration describing the COVID-19 outbreak originated in Wuhan, China as a pandemic on March 11, 2020, and increased Google search interest (indicating greater public awareness of COVID-19) [1]. The number of ED visits per week for the last four weeks of available data (from the week of March 15, 2020 to the week of April 5, 2020) was also found to be significantly less than a period of four weeks (from the week of December 15, 2019 to the week of January 5, 2020) prior to increased COVID-19 awareness as determined by Google search trends. This significant decrease in ED visits per week may partly be explained by desire to maintain social distancing and a desire to avoid contact with infected individuals. A recent poll conducted by the Kaiser Family Foundation in the US from March 25-30th, 2020 identified that 57% of respondents were concerned about being exposed to COVID-19 due to an inability to stay home and miss work [11]. The results of the poll also demonstrated that 82% of respondents were concerned that they will be unable to obtain needed medical care due to the health care system being overrun [11]. Thus, it appears that the current COVID-19 pandemic may have created a climate of fear similar to what has been observed in other countries like Germany and China [3,4].
The study also demonstrated regional variation in the percentage decrease in mean ED visits per week across all regions studied. Region 1 had the greatest decrease (45%) and region 8 had the smallest decrease (31%). This variation could be due to regional cultural differences affecting levels of compliance with health guidelines, level of concern regarding infection, differences in socioeconomic status, and varying remote work opportunities. Finally, a steep decline in MVCs was noted across all cities studied, with the greatest decrease seen in NYC and Baton Rouge (66%). This finding is not surprising given the rise of remote work, curfews, stay at home orders, closure of nonessential businesses, COVID-19 fears, and social distancing. This decrease in MVCs has likely also substantially contributed to reduced ED visits.
This study has several limitations. First, inconsistency in reporting and lack of centralized resources for up to date MVC data reduced the sample size and hindered the extrapolation of results to all regions studied. Next, a lack of current fatality data due to medical conditions of almost any kind prevented an analysis of the association between reduced ED visits and current fatality trends.
5. Conclusions
The mean number of ED visits per week for the last four weeks of available data during the pandemic was significantly less than the four weeks prior to COVID-19 pandemic. A number of factors including the current climate of fear regarding COVID-19 infection and decreased opportunity for injury due to MVCs have likely contributed to the substantial decrease in ED visits. In light of these findings, it is important to raise patient awareness regarding acute conditions (e.g., STEMI and stroke) that are deadlier than COVID-19 and require immediate medical intervention to ensure recovery. Patients should also be made aware of the strict COVID-19 guidelines imposed by organizations such as the CDC, the American College of Emergency Physicians, the American College of Surgeons and others to increase patient confidence. In contrast, patients should also be made aware of telehealth options for non-acute conditions but need to be encouraged to utilize ED services during an emergency.
Funding
None.
Declaration of competing interest
Authors declare no competing interests.
References
- 1.World Health Organization. WHO director-General's opening remarks at the media briefing on COVID-19 - 11 march 2020. World Health Organization. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Published 2020. Accessed April 19, 2020.
- 2.Centers for Disease Control and Prevention. Cases of coronavirus disease (COVID-19) in the U.S. U.S. Department of Health & Human Services. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Published 2020. Accessed April 18, 2020.
- 3.Gerhold L. 2020. COVID-19: Risk perception and coping strategies. [Google Scholar]
- 4.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parmet W.E., Sinha M.S. Covid-19 — the law and limits of quarantine. New England Journal of Medicine. 2020;382(15):e28. doi: 10.1056/NEJMp2004211. [DOI] [PubMed] [Google Scholar]
- 6.Desantis R. State of Florida Office of the Governor Executive Order Number 20-91 (essential services and activities during COVID-19 emergency. In: Governor EOoT, ed. State of Florida2020.
- 7.Castro V.M., Perlis R.H. Impact of COVID-19 on psychiatric assessment in emergency and outpatient settings measured using electronic health records. medRxiv. 2020 doi: 10.1101/2020.03.30.20048207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodríguez-Leor O., Cid-Alvarez B., Ojeda S. REC: Interventional cardiology. 2020. Impact of the COVID-19 pandemic on care activity in interventional cardiology in Spain. Published. [Accessed2020] [Google Scholar]
- 9.Centers for Disease Control and Prevention . U.S. Department of Health & Human Services; 2020. Evaluating and testing persons for coronavirus disease (COVID-19) Published. [Accessed April 26, 2020] [Google Scholar]
- 10.Johns Hopkins. COVID-19 case tracker. Johns Hopkins https://coronavirus.jhu.edu/. Published 2020. Accessed April 26, 2020.
- 11.Kirzinger A., Kearney A., Hamel L., Brodie M. Kaiser Family Foundation; 2020. KFF health tracking poll - early April 2020: the impact of coronavirus on life in America. [Google Scholar]