Abstract
The novel coronavirus disease of 2019 (COVID-19) is associated with significant morbidity and mortality. While much of the focus has been on the cardiac and pulmonary complications, there are several important dermatologic components that clinicians must be aware of.
Objective
This brief report summarizes the dermatologic manifestations and complications associated with COVID-19 with an emphasis on Emergency Medicine clinicians.
Discussion
Dermatologic manifestations of COVID-19 are increasingly recognized within the literature. The primary etiologies include vasculitis versus direct viral involvement. There are several types of skin findings described in association with COVID-19. These include maculopapular rashes, urticaria, vesicles, petechiae, purpura, chilblains, livedo racemosa, and distal limb ischemia. While most of these dermatologic findings are self-resolving, they can help increase one's suspicion for COVID-19.
Conclusion
It is important to be aware of the dermatologic manifestations and complications of COVID-19. Knowledge of the components is important to help identify potential COVID-19 patients and properly treat complications.
Keywords: COVID-19, SARS-CoV-2, Coronavirus, Dermatology, Skin, Emergency medicine
1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the underlying cause of the novel coronavirus disease of 2019 (COVID-19), which has resulted in over 3.8 million infected patients worldwide [1]. While the majority of patients will experience respiratory complaints with congestion, cough, and shortness of breath, some patients may present without any pulmonary symptoms [[2], [3], [4]]. As the disease has progressed, literature has described involvement of other organ systems, including the cardiovascular, gastrointestinal, renal, and neurologic systems. Recently, there has been increasing recognition of the dermatologic complications of COVID-19.
2. Methods
This brief report outlines the underlying pathophysiology and dermatologic manifestations of COVID-19 with an emphasis on the ED clinician. A literature review of the PubMed and Google Scholar databases was performed from inception to May 2nd, 2020 for articles using the keywords COVID-19, SARS-CoV-2, dermatolog*, and skin for production of this brief report. Authors included case reports and series, retrospective and prospective studies, systematic reviews and meta-analyses, clinical guidelines, and narrative reviews. Commentaries and letters were also included. The initial literature search revealed 1553 articles. Authors reviewed all relevant articles and decided which studies to include for the brief report by consensus, with focus on emergency medicine-relevant articles. A total of 41 resources were selected for inclusion in this review.
3. Discussion
3.1. Pathophysiology and clinical features
SARS-CoV-2 is an RNA virus that may enter cells through the angiotensin-converting enzyme 2 (ACE2) receptor found on lung alveolar epithelial cells, small intestine enterocytes, and vasculature, as well as neurologic, endocrine, and cardiac systems [5,6]. ACE2 plays several key roles in normal physiology, including breakdown of angiotensin II [6]. SARS-CoV-2 may cause direct lung injury and systemic inflammation, as well as increased coagulation [[7], [8], [9]]. These factors can result in multiorgan dysfunction. Recent literature suggests ACE2 is also located in the skin, which may explain some of the dermatologic manifestations in the setting of COVID-19 infection [10].
Some case reports have noted that dermatologic findings may present prior to respiratory symptoms, though most studies suggest skin manifestations present several days after the onset of other symptoms [[11], [12], [13]]. These signs and symptoms may assist clinicians in considering the disease before the development of respiratory symptoms and may also be used to identify complications requiring treatment.
3.2. Dermatologic manifestations
While the most common symptoms of COVID-19 include congestion, cough, dyspnea, and fever, skin symptoms can occur in up to 20.4% of patients [11]. One early study found that only 2 of 1099 patients had a “rash”, but investigators may have missed several patients [2]. A more recent study found rash occurred in 18 of 88 patients, with 8 of these patients having rash at onset, while another study found that rash occurred in 5 out of 103 patients [11,14].
There are several proposed etiologies for rash in patients with COVID-19. The first is diffuse microvascular vasculitis, resulting from complement system activation. One study found significant complement protein deposition in the dermal capillaries, as well as interstitial and perivascular neutrophilia with prominent leukocytoclasia, suggesting a vasculitic phenomenon [15]. Others have suggested that this occurs as a direct effect of the virus. This has been based on high concentrations of lymphocytes without eosinophils, papillary dermal edema, epidermal spongiosis, and lymphohistiocytic infiltrates [16,17].
A rash associated with COVID-19 can involve various body regions, most commonly the trunk, but extremity involvement may also occur [11]. Pruritus is often minimal but depends on the type of rash, and lesions typically heal quickly, appearing within 3 days and disappearing within 8 days [11,18].
A challenging aspect of rash associated with COVID-19 is the myriad types of presentation. Many of these rashes have a broad differential diagnosis. However, it is important to consider COVID-19, especially in the patient with upper respiratory or systemic symptoms (Table 1 ).
Table 1.
Potential causes of each dermatologic finding.
| Dermatologic finding | Potential causes |
|---|---|
| Maculopapular rash | Viral exanthem, Scarlet fever, measles, rubella, medication reaction, secondary syphilis, heat rash, leukemia, graft-versus-host disease |
| Urticaria | Allergic reaction, anaphylaxis, angioedema, autoimmune disease (e.g., systemic lupus erythematosus), hypereosinophilia, chronic urticaria, malignancy |
| Vesicular | Varicella zoster (i.e., chickenpox), herpes zoster (i.e., shingles), herpes simplex, Rhus dermatitis (e.g., poison ivy, poison oak, poison sumac), pemphigoid |
| Petechiae/purpura | Thrombocytopenia, systemic lupus erythematosus, leukemia, disseminated intravascular coagulation, hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, vasculitis, vitamin C deficiency |
| Chilblains | Raynaud's phenomenon, systemic lupus erythematosus, systemic sclerosis, Buerger's disease |
| Livedo racemosa | Antiphospholipid antibody syndrome, Sneddon syndrome, cryoglobulinemia, multiple myeloma, disseminated intravascular coagulation, hemolytic uremic syndrome, deep venous thrombosis, systemic lupus erythematosus, rheumatoid arthritis, polyarteritis nodosa, Sjogren's syndrome, multiple sclerosis, Parkinson's disease, cancer (e.g., renal cell cancer, breast cancer, lymphoma, leukemia) |
| Distal ischemia/necrosis | Arterial ischemia, disseminated intravascular coagulation, Buerger's disease |
3.3. Maculopapular rash
There are multiple reports of patients presenting with a maculopapular rash, characterized by erythematous macules covered with small papules, or with large plaques (Fig. 1 ) [17,[19], [20], [21]]. The rash may also be perifollicular and associated with scaling and confluence, which may cause it to be mistaken for pityriasis rosea [22]. This type of rash has been suggested to have a mean duration of approximately 9 days [22]. One study of 88 patients in Italy found that a maculopapular rash was present in 14 patients (16%) [11].
Fig. 1.
Maculopapular rash.
Obtained from https://commons.wikimedia.org/wiki/File:Marburg_patient.jpg.
There are several descriptions of the rash in the literature. Four case reports comprising 7 patients described this as diffuse [16,20,23,24]. Some have identified this most commonly on the limbs and trunk [[25], [26], [27], [28]]. Others have described this on the face [14] or bilateral heels [29]. Two studies have described this as centrifugal in nature, initially starting in the periumbilical or trunk region before spreading distally [17,27].
3.4. Urticaria
Urticaria presents with acute, swollen, red wheals or plaques, typically associated with pruritis (Fig. 2 ). They occur due to a variety of causes and have been documented to occur with COVID-19. One study by Recalcati found urticaria in 3 of 88 COVID-19 patients [11]. There have been other reports of urticaria affecting various regions of the body in patients of all age groups infected with COVID-19. These cases describe involvement of the trunk, extremities, and head, as well as rash migration, with sparing of the palms and soles [12,14,19,27,28,[30], [31], [32], [33]]. One of the largest series of 73 COVID-19 positive patients with urticaria found that the trunk was most commonly involved, and pruritus occurred in 92% of cases [22]. The mean duration of symptoms was 6.8 days [22]. This study also found that urticaria generally occurred concomitantly with other symptoms in the majority of cases and was associated with more severe disease in this study, with a 2% mortality rate in this population [22].
Fig. 2.
Urticaria.
Obtained from https://commons.wikimedia.org/wiki/File:Hives_Urticaria.jpg.
3.5. Vesicular
Vesicular rashes include small, fluid-filled blisters, often on an erythematous base (Fig. 3 ). Numerous case reports have documented vesicular rashes in patients with COVID-19, with the study by Recalcati et al. finding vesicles in 1.1% of patients [11]. Vesicles are more commonly scattered, rather than diffuse in appearance, with one series finding scattered lesions in 16 of 22 patients and diffuse lesions in the remaining six patients [18]. Other case reports have described the appearance of vesicles [19,34], with one discussing diffuse involvement of the face and limbs in an 8-year-old [13]. A separate case series found that the vesicular rash occurred for a mean duration of 10.4 days, with vesicles appearing mostly on the trunk and extremities [22]. They also noted that the lesions appeared small and monomorphic as opposed to chickenpox and had hemorrhagic content [22]. In most cases, the vesicular rash preceded other symptoms [22].
Fig. 3.
Vesicular rash.
Obtained from https://commons.wikimedia.org/wiki/File:Chickenpox_Adult_back.jpg.
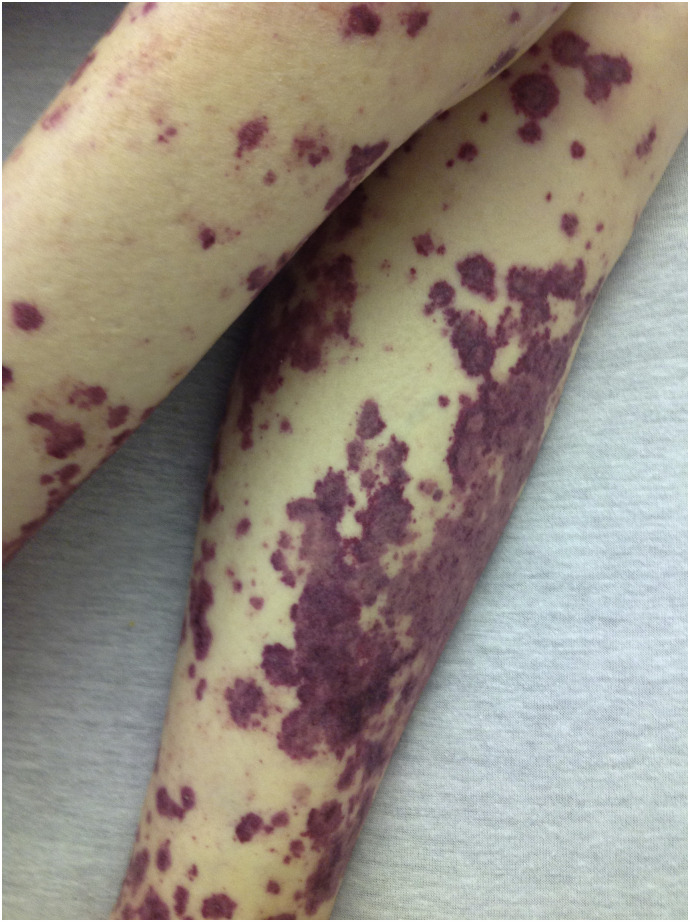
3.6. Petechiae/purpura
Petechiae are small, subdermal hemorrhages, while purpura are larger variants of this (Fig. 4 ). This rash is less commonly described than some of the other rashes, though there are a few case reports describing this in the literature. One case report described a patient with petechiae who was initially misdiagnosed as dengue fever (in an endemic area), but later discovered to have COVID-19 [35]. In this case, the patient was also noted to be significantly thrombocytopenic [35]. Another case described a patient with extensive purpura isolated to flexural areas [36]. Thrombocytopenia is not a common complication in COVID-19, so this may reflect a less common complication, or the rash may be due to an alternate etiology such as vasculitis.
Fig. 4.
Petechial rash.
Obtained from https://commons.wikimedia.org/wiki/File:Petechial_rash.JPG.
3.7. Chilblains
Chilblains (also known as pernio or perniosis) is an abnormal response to cold, wherein distal arteries and veins constrict, which can lead to pruritic and tender wounds on the extremities (Fig. 5 ). Patients can present with erythematous or violaceous papules and macules, bullae, or digital swelling [37]. This has been increasingly recognized in association with COVID-19. There have been nearly 100 cases of chilblains associated with COVID-19 already described in the literature [19,22,37,38]. Galván Casas et al. described 71 cases which had a mean duration of 12.7 days [22]. The authors noted that it typically presented in the hands or feet and was usually asymmetrical [22]. Thirty-two percent of cases were painful and 30% had associated pruritus [22]. Compared with other rashes, chilblains typically occurred later in the disease course and after other symptoms had presented [22]. The authors also noted that this was more common in younger patients (mean age 32 years) than the other rashes in their study [22]. This was also evidenced by Recalcati who described 14 cases occurring in mostly children and young adults [37]. In this latter case series, 10 patients had feet involvement, while only 6 had hand involvement [37].
Fig. 5.
Chilblains of the foot.
Obtained from https://commons.wikimedia.org/wiki/File:Wintertenen.jpg.
3.8. Livedo racemosa
Livedo racemosa (LR) is a violaceous web or net-like patterning of the skin similar to livedo reticularis; however, this is found diffusely, compared to livedo reticularis that is found in gravity-dependent areas (Fig. 6 ) [39]. Reports have described LR or retiform purpura (branching grouping of purpura) in 3 patients in one series [15], as well as several other case reports [19,40]. One series of 21 cases found that the rash had a mean duration of 9.4 days [22]. LR was more common in older patients, with a mean age of 63 years [22]. LR was also associated with more severe disease (10% mortality rate) [22].
Fig. 6.
Livedo reticularis of the lower extremity.
Obtained from https://en.wikipedia.org/wiki/Livedo_reticularis#/media/File:Livedo_reticularis_of_left_leg.jpg.
3.9. Distal ischemia and necrosis
Perhaps one of the most severe complications includes distal ischemia resulting in tissue necrosis (Fig. 7 ). One case series described seven patients with acro-ischemia including finger and toe cyanosis, skin bullae, and dry gangrene [41]. Another report of two patients described the appearance of red and purple papules on the distal fingers due to distal ischemia, which occurred before the appearance of other symptoms [42]. Other case reports describe a 13-year-old with distal toe ischemia presenting with blistering and necrosis [43], as well as one patient with necrotic purpura [19]. Given the coagulopathic impact of SARS-CoV-2, these findings necessitate discussion with vascular surgery specialists and consideration of intravenous thrombolytics.
Fig. 7.
Necrotic toe.
Obtained from https://commons.wikimedia.org/wiki/File:Dry_gangene_4th_toe.jpg.
4. Conclusion
Patients with COVID-19 most commonly present with respiratory symptoms, but multiorgan involvement can occur, with multiple skin manifestations. Dermatologic findings may include a maculopapular rash, urticaria, vesicular rash, petechia, purpura, chilblains, livedo racemosa, and distal ischemia. These rashes should trigger consideration of COVID-19, and understanding these manifestations is important to help identify potential COVID-19 patients and properly treat complications.
Meetings
None.
Grants
None.
Author contributions
None except listed.
Declaration of competing interest
None.
Acknowledgements
This review does not reflect the views or opinions of the U.S. government, Department of Defense, U.S. Army, U.S. Air Force, Brooke Army Medical Center, or SAUSHEC EM Residency Program.
References
- 1.World Health Organization Situation report 110. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ Available at.
- 2.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Long B., Brady W.J., Koyfman A., Gottlieb M. Cardiovascular complications in COVID-19 [published online ahead of print, 2020 Apr 18] Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bridwell R., Long B., Gottlieb M. Neurologic complications of COVID-19 [published online ahead of print, 2020 May 16] Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamming I., Timens W., Bulthuis M.L., Lely A.T., Navis G., van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang H., Penninger J.M., Li Y., Zhong N., Slutsky A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586–590. doi: 10.1007/s00134-020-05985-9. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. Feb 7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li M.Y., Li L., Zhang Y., Wang X.S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. Apr 28 2020;9(1):45. doi: 10.1186/s40249-020-00662-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16387. [published online ahead of print, 2020 Mar 26] [DOI] [PubMed] [Google Scholar]
- 12.Henry D., Ackerman M., Sancelme E., Finon A., Esteve E. Urticarial eruption in COVID-19 infection. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16472. [published online ahead of print, 2020 Apr 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Genovese G., Colonna C., Marzano A.V. Varicella-like exanthem associated with COVID-19 in an 8-year-old girl: a diagnostic clue? Pediatr Dermatol. 2020 doi: 10.1111/pde.14201. [published online ahead of print, 2020 Apr 21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hedou M., Carsuzaa F., Chary E., Hainaut E., Cazenave-Roblot F., Masson Regnault M. Comment on “Cutaneous manifestations in COVID-19: a first perspective” by Recalcati S. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16519. [published online ahead of print, 2020 Apr 21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Magro C., Mulvey J.J., Berlin D. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020 doi: 10.1016/j.trsl.2020.04.007. [S1931-5244(20)30070-0, published online ahead of print, 2020 Apr 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gianotti R., Veraldi S., Recalcati S. Cutaneous clinico-pathological findings in three COVID-19-positive patients observed in the metropolitan area of Milan, Italy. Acta Derm Venereol. 2020 doi: 10.2340/00015555-3490. [published online ahead of print, 2020 Apr 21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanchez A., Sohier P., Benghanem S. Digitate papulosquamous eruption associated with severe acute respiratory syndrome coronavirus 2 infection. JAMA Dermatol. 2020 doi: 10.1001/jamadermatol.2020.1704. [published online ahead of print, 2020 Apr 30] [DOI] [PubMed] [Google Scholar]
- 18.Marzano A.V., Genovese G., Fabbrocini G. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.04.044. [published online ahead of print, 2020 Apr 16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouaziz J.D., Duong T., Jachiet M. Vascular skin symptoms in COVID-19: a french observational study. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16544. [published online ahead of print, 2020 Apr 27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amatore F., Macagno N., Mailhe M. SARS-CoV-2 infection presenting as a febrile rash. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16528. [published online ahead of print, 2020 Apr 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gisondi P., Piaserico S., Conti A., Naldi L. Dermatologists and SARS-CoV-2: the impact of the pandemic on daily practice. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16515. [published online ahead of print, 2020 Apr 22] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galván Casas C., Català A., Carretero Hernández G. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020 doi: 10.1111/bjd.19163. [published online ahead of print, 2020 Apr 29] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hunt M., Koziatek C. A case of COVID-19 pneumonia in a young male with full body rash as a presenting symptom. Clin Pract Cases Emerg Med. 2020 doi: 10.5811/cpcem.2020.3.47349. [published online ahead of print, 2020 Mar 28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Najarian D.J. Morbilliform Exanthem associated with COVID-19. JAAD Case Rep. 2020 doi: 10.1016/j.jdcr.2020.04.015. [published online ahead of print, 2020 Apr 20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahouach B., Harant S., Ullmer A. Cutaneous lesions in a patient with COVID-19: are they related? Br J Dermatol. 2020 doi: 10.1111/bjd.19168. [published online ahead of print, 2020 Apr 30] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mahé A., Birckel E., Krieger S., Merklen C., Bottlaender L. A distinctive skin rash associated with Coronavirus Disease 2019? J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16471. [published online ahead of print, 2020 Apr 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morey-Olivé M., Espiau M., Mercadal-Hally M., Lera-Carballo E., García-Patos V. Cutaneous manifestations in the current pandemic of coronavirus infection disease (COVID 2019) An Pediatr (Engl Ed) 2020 doi: 10.1016/j.anpede.2020.04.002. [published online ahead of print, 2020 Apr 27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rivera-Oyola R., Koschitzky M., Printy R. Dermatologic findings in two patients with COVID-19. JAAD Case Rep. 2020 doi: 10.1016/j.jdcr.2020.04.027. [published online ahead of print, 2020 Apr 28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Estébanez A., Pérez-Santiago L., Silva E., Guillen-Climent S., García-Vázquez A., Ramón M.D. Cutaneous manifestations in COVID-19: a new contribution. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16474. [published online ahead of print, 2020 Apr 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu S., Lin J., Zhang Z. Alert for non-respiratory symptoms of Coronavirus Disease 2019 (COVID-19) patients in epidemic period: a case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25776. [published online ahead of print, 2020 Mar 19] [DOI] [PubMed] [Google Scholar]
- 31.Fernandez-Nieto D., Ortega-Quijano D., Segurado-Miravalles G., Pindado-Ortega C., Prieto-Barrios M., Jimenez-Cauhe J. Comment on: cutaneous manifestations in COVID-19: a first perspective. Safety concerns of clinical images and skin biopsies. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16470. [published online ahead of print, 2020 Apr 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quintana-Castanedo L., Feito-Rodríguez M., Valero-López I., Chiloeches-Fernández C., Sendagorta-Cudós E., Herranz-Pinto P. Urticarial exanthem as early diagnostic clue for COVID-19 infection. JAAD Case Rep. 2020 doi: 10.1016/j.jdcr.2020.04.026. [published online ahead of print, 2020 Apr 29] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Damme C., Berlingin E., Saussez S., Accaputo O. Acute urticaria with pyrexia as the first manifestations of a COVID-19 infection. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16523. [published online ahead of print, 2020 Apr 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tammaro A., Adebanjo G.A.R., Parisella F.R., Pezzuto A., Rello J. Cutaneous manifestations in COVID-19: the experiences of Barcelona and Rome. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16530. [published online ahead of print, 2020 Apr 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Joob B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol. 2020;82(5):e177. doi: 10.1016/j.jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jimenez-Cauhe J., Ortega-Quijano D., Prieto-Barrios M., Moreno-Arrones O.M., Fernandez-Nieto D. Reply to “COVID-19 can present with a rash and be mistaken for Dengue”: petechial rash in a patient with COVID-19 infection. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.04.016. [published online ahead of print, 2020 Apr 10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Recalcati S., Barbagallo T., Frasin L.A. Acral cutaneous lesions in the time of COVID-19. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16533. [published online ahead of print, 2020 Apr 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Landa N., Mendieta-Eckert M., Fonda-Pascual P., Aguirre T. Chilblain-like lesions on feet and hands during the COVID-19 Pandemic. Int J Dermatol. 2020 doi: 10.1111/ijd.14937. [published online ahead of print, 2020 Apr 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uthman I.W., Khamashta M.A. Livedo racemosa: a striking dermatological sign for the antiphospholipid syndrome. J Rheumatol. 2006;33(12):2379–2382. [PubMed] [Google Scholar]
- 40.Manalo I.F., Smith M.K., Cheeley J., Jacobs R. A dermatologic manifestation of COVID-19: transient livedo reticularis. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.04.018. [published online ahead of print, 2020 Apr 10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang Y., Cao W., Xiao M. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi. 2020;41(0) doi: 10.3760/cma.j.issn.0253-2727.2020.0006. [DOI] [PubMed] [Google Scholar]
- 42.Alramthan A., Aldaraji W. A case of COVID-19 presenting in clinical picture resembling chilblains disease. First report from the Middle East. Clin Exp Dermatol. 2020 doi: 10.1111/ced.14243. [published online ahead of print, 2020 Apr 17] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mazzotta F., Troccoli T. Acute Acro-ischemia in the child at the time of COVID-19. Dermatologia Pediatrica. 2020 https://www.ejpd.com/images/acroischemia-ENG.pdf Available at. [Google Scholar]