Abstract
The world has been challenged by SARS CoV-2, a new virus causing pneumonia and acute respiratory distress syndrome, with common symptoms of COVID-19 in pediatric patients including both respiratory and GI symptoms. There is a lack of literature implicating COVID-19 in pancreatitis, yet viruses are generally understood to be a cause of pancreatitis in children. We present a case of a previously well 7-year-old girl, who presented to the emergency department with a chief complaint of abdominal pain and anorexia. She was diagnosed with acute pancreatitis with an abnormal lipase, ultrasound, and computed tomography, and was found to be COVID-19 positive by polymerase chain reaction. Our case suggests that, in the current pandemic, consideration for SARS CoV-2 testing in children with gastrointestinal symptoms and pancreatitis may be considered. Additionally, this case highlights the need for appropriate personal protective equipment for providers, even when COVID is not initially on the differential.
Keywords: SARS CoV-2, COVID-19, Acute pancreatitis, Pediatrics
Introduction
In 2019, the first cases of COVID-19 pneumonia and acute respiratory distress syndrome were reported in China [1]. The virus quickly propagated with the first case in the United States reported in January 2020 [1]. Since its discovery, there has been scientific pressure to characterize the symptomatology caused by the SARS CoV-2 virus. Common symptoms in pediatric populations include fever (36%-80%), dry cough (19%-65%), tachycardia (42%), tachypnea (29%), and less commonly diarrhea, vomiting, and abdominal pain (4%-10%) [2]. A majority of pediatric patients presenting with SARS CoV-2 present with mild symptoms (51%) including acute URI, fever, fatigue, myalgia, nausea, vomiting, abdominal pain and diarrhea [3]. As of March 5, 2020, the CDC reports only 2% of confirmed SARS CoV-2 cases in the United States have occurred in patients <18 years old [4].
Acute pancreatitis in children occurs in approximately 1/10,000 children per year [5]. Viral infections are identified as a cause of acute pancreatitis in approximately 8%-10% of cases in children with other common causes being biliary/obstructive (10%-30%), medications (5%-25%), and trauma (10%-20%) [5].
Case report
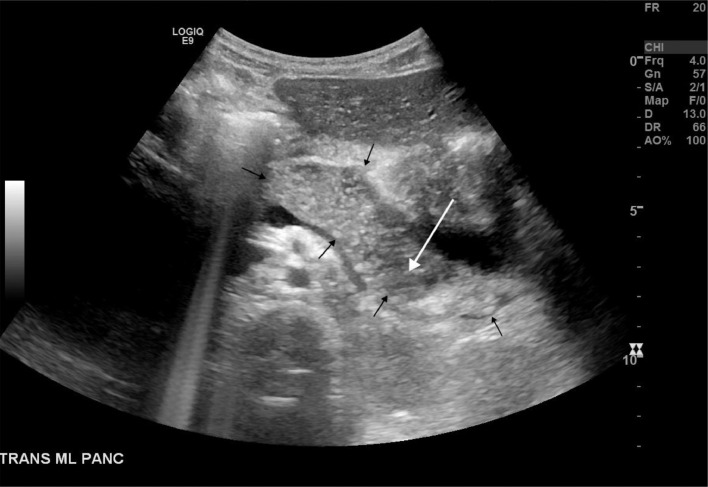
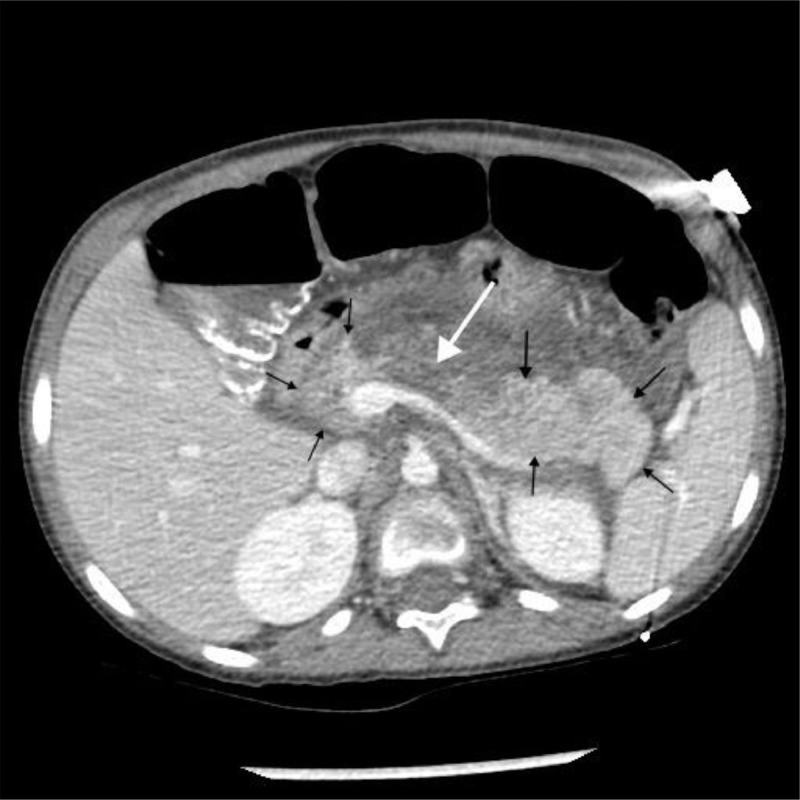
We present a case of a previously well 7-year-old girl who initially complained of 48 hours of abdominal pain and anorexia. She was afebrile, with elevated lipase (676, normal 80-360 U/L) and an abdominal ultrasound and CT (Figs. 1 and 2) suggestive of necrotizing pancreatitis. The lower chest on the abdominal CT showed a normal-sized heart, small bilateral pleural effusions, and clear lung bases. Her pancreatitis was managed with IV fluids, ketorolac, and hydralazine; she was started on ceftriaxone and metronidazole. She improved with supportive care and was discharged on hospital day 4 with a normal lipase. Two weeks later her abdominal pain returned and was associated with reported fever (101°F).
Fig. 1.
Midline transverse grayscale sonographic image at the level of the pancreas (black arrows) reveals diffuse pancreatic enlargement and heterogeneous pancreatic echogenicity (white arrow) concerning for acute pancreatitis.
Fig. 2.
Postcontrast axial CT image at the level of the pancreas (black arrows) reveals diffuse pancreatic edema/enlargement with peripancreatic fluid and increased attenuation of the adjacent peripancreatic fat representing acute pancreatitis. An area of pancreatic parenchymal hypoenhancement (white arrow) is suspicious for pancreatic necrosis (necrotizing pancreatitis).
Simultaneously, her mother, a warehouse worker was experiencing fever, cough, and shortness of breath. Our patient denied shortness of breath or cough. She also presented with nonbloody, nonbilious emesis left lower quadrant, and epigastric pain.
On examination, her vital signs were BP: 130/92, P: 128, T: 99.9°F, RR: 24, BMI 13.79. She appeared uncomfortable, but nontoxic. Her abdominal exam was significant for distension and tenderness to palpation in the left upper and left lower quadrant, and the epigastric regions. There was fullness noted in the left upper, but no splenic edge was felt and there was no guarding, rebound, right lower quadrant tenderness, Rovsing, or psoas sign.
Her lipase this time was 1672 U/L, and due to fever and potential family exposure in a COVID-19 pandemic she was tested for SARS CoV-2 by polymerase chain reaction which was positive. She had thrombocytosis (498 thou/cmm), an elevated LDH (271 U/L), and an elevated IL-6 (13 pg/mL). A complete respiratory viral panel was negative including influenza A, B and RSV. She was managed again with bowel rest, IV, ketorolac, acetaminophen, and ceftriaxone and metronidazole until blood cultures returned. Over the next 2 days, she improved significantly and was discharged with a lipase that was trending down. Of note, the patient's mother, her mother's partner, and her older sister all tested positive for COVID-19 after the patient.
Discussion
While there is evidence that children with COVID-19 develop abdominal pain and vomiting, the effects of the virus specifically on the pancreas have not been described [2,3,6,7]. It is unclear if our patient's pancreatitis was associated or caused by COVID-19. Because children remain PCR positive longer than adults and they do not have to show respiratory symptoms, patients can have the disease for long before symptoms; it is possible that even the first experience of pancreatitis was related to COVID-19 [2]. In hindsight, her initial CT showed not only mild-to-moderate edema and ascites in the abdomen and pelvis but also small bilateral pleural effusions. Her lipase on the second admission was much higher—there is at the least, concern that there may have been a new factor that aggravated her underlying necrotizing pancreatitis. The mechanism for how COVID-19 infection can cause acute pancreatitis is unclear. It may be related to direct infection of the pancreas by the virus, as has been reported for other viruses [8,9]. There is currently some evidence that it enters GI epithelium via ACE-2 receptors, the same receptor it enters in the lungs, which may provide a possible pathophysiologic explanation for GI symptoms experienced in patients. The endothelial location of the ACE-2 receptors is also the hypothesized mechanism for increased thrombophilia in COVID-19 and potentially an etiology of the acute pancreatitis [10]. This case certainly leaves the possibility of a coincidental nature of COVID-19 and pancreatitis in a child, it was not on the differential for the child in the first hospital stay. Currently, the literature has focused on respiratory symptoms and associated lymphopenia and elevated liver function abnormalities, whereas the GI symptoms are left largely unexplored [2,3,6,7]. Further research is needed to explore the possibility of causation for acute pancreatitis in children with COVID-19. In the current pandemic, consideration for SARS CoV-2 testing in children with acute pancreatitis may be considered. Finally, this case highlights the need for appropriate personal protective equipment, even when COVID is not initially on the differential.
Author contributions
All authors provided substantial contributions to manuscript content. All authors gave final approval of the version of the article to be published.
Acknowledgment
The authors would like to acknowledge Adam P. Wallach, MD and Bret J. Kricun, MD for radiology assistance and to Marna Rayl Greenberg, DO, MPH for formatting and editing.
Footnotes
Competing Interests: The authors have no outside support information, conflicts or financial interest to disclose.
References
- 1.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Streng A., Hartmann K., Armann J., Berner R., Liese J.G. COVID-19 bei hospitalisierten Kindern und Jugendlichen: Ein systematischer Review zu publizierten Fallserien (Stand 31.03.2020) und erste Daten aus Deutschland [COVID-19 in hospitalized children and adolescents] Monatsschr Kinderheilkd. 2020:1–12. doi: 10.1007/s00112-020-00919-7. [Published online ahead of print, 2020 April 21] [DOI] [PMC free article] [PubMed] [Google Scholar]; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7171916/.
- 3.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z. Epidemiology of COVID-19 among children in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. Accessed 16 May, 2020. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention, Information for pediatric healthcare providers 2020. www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html, Accessed 16 May, 2020.
- 5.Pohl J.F., Uc A. Paediatric pancreatitis. Curr Opin Gastroenterol. 2015;31(5):380–386. doi: 10.1097/MOG.0000000000000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang T.H., Wu J.L., Chang L.Y. Clinical characteristics and diagnostic challenges of pediatric COVID-19: A systematic review and meta-analysis. J Formos Med Assoc. 2020 doi: 10.1016/j.jfma.2020.04.007. [Published online ahead of print, 2020 April 16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39(5):355–368. doi: 10.1097/INF.0000000000002660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parenti D.M., Steinberg W, Kang P. Infectious Causes of acute pancreatitis. Pancreas. 1996;13(4):356–371. doi: 10.1097/00006676-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Capua I., Mercalli A, Pizzuto M, Romero-Tejeda A, Kasloff S, DeBattisti C. Influenza A viruses grow in human pancreatic cells and cause pancreatitis and diabetes in an animal model. J Virol. 2013;87(1):597–610. doi: 10.1128/JVI.00714-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E. COVID-19 and Thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]