1. Clinical note
We present the case of a 74-year-old male with an 18-year history of IgG kappa multiple myeloma who received multiple lines of treatment, including carfilzomib-dexamethasone every three weeks for the last 8 months.
On April 1th, 2020, the patient presented to the outpatient clinic with asthenia, dry cough, and fever, so carfilzomib-dexamethasone was not administered. He was diagnosed with severe bilateral pneumonia due to SARS-CoV-2 infection. Laboratory tests showed ferritin of 4242 ng/mL (30–400), IL-6 of 85.97 pg/mL (0–7) and lymphocytes of 130 cels/μL (900–5200). He was hospitalized initiating treatment with hydroxichloroquine 200 mg/12 h, lopinavir/ritonavir 400−100 mg/12 h, ceftriaxone 2 g/24 h, dexamethasone 20 mg/12 h and enoxaparin at a prophylactic dose of 40 mg/24 h. Initially he remained stable, but despite the treatment his condition worsened quickly, developing severe lymphopenia (30–40 cels/μL) and severe anemia with haemoglobin of 7,5 g/dl.
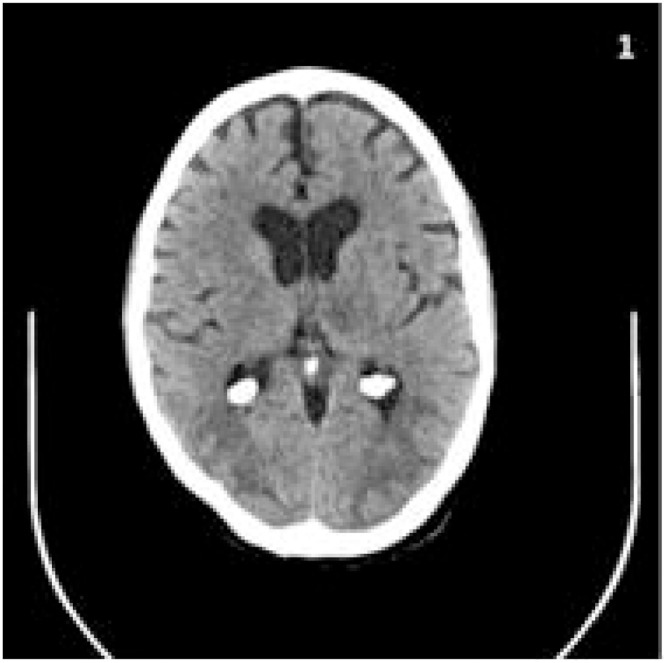
On the 15th day of hospitalization, once the infection had partially improved, he suffered two focal aware motor seizures, described as left oculocefalic deviation and clonic movements of the upper left limb, that ceased spontaneously. At that moment his systolic blood pressure was of 140−150 mmHg, higher than his usual levels of 110−120 mmHg. Following this episode, he presented a new focal motor onset seizure with impaired awareness. As he did not recover, progressive doses of antiepileptics were administered, reaching a total of 20 mg of diazepam, 1500 mg of levetiracetam, 200 mg of lacosamide and 1000 mg of valproate, without ceasing. An urgent cranial CT revealed cortical and subcortical hypodensities, with predominance on the parietooccipital regions, also affecting the frontal lobe, left basal ganglia, brain stem and cerebellum, a distribution consistent with reversible posterior leucoencephalopathy syndrome (PRES) (Image 1 ).
Image 1.
TC: occipital hypodensities.
The Intensive Care Unit rejected the case, due to his previous condition and the work overload of the ICU due to the SARS-CoV-2 pandemic. Two and a half hours after the onset of the symptoms, the patient had not recovered yet, despite using all the aforementioned drugs. Under the suspicion of refractory status epilepticus secondary to PRES, 2.5 mg of verapamil were administered. Promptly the patient recovered awareness completely, but developed cortical blindness and upper left limb palsy, which disappeared on the following days. A maintenance treatment with 1600 mg/ 24 h of valproate, 1500 mg/ 12 h of levetiracetam and 200 mg/ 12 h of lacosamide was prescribed, without developing any new seizures.
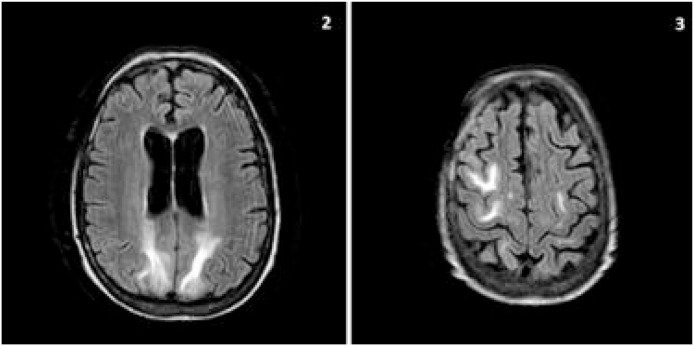
Being the patient stable, and 24 h after the onset of the status epilepticus, a lumbar puncture discarded evidence of infection by bacteria or neurotropic viruses, including SARS-Cov2. A cerebral MRI study showed hyperintensities on T2-weighted image and FLAIR sequences, predominantly on frontoparietal and occipital subcortical areas bilaterally, highly compatible with the diagnosis of PRES (Image 2 ).
Image 2.
1 hyperintensities in FLAIR secuence in parietal (2) and right frontal (3) white mater.
After reviewing the case, infection due to SARS-Cov-2 was proposed as the etiology of the PRES. The new coronavirus can induce endothelial dysfunction [1] that can damage the blood-brain barrier, making it highly permeable and subsequently causing cerebral edema, the underlying mechanism of PRES. This endothelial dysfunction determines a microvascular disturbance that may produce vasoconstriction, which can influence the development of PRES. In addition, the infection by SARS-CoV-2 can lead to a systemic inflammatory response mediated by proinflamatory cytokines, including TNF alpha. This motivates endothelial activation, increases vascular permeability and ultimately the cerebral interstitial edema [2]. Finally, carfilzomib has been described as an etiological factor in the appearance of PRES [3], and probably played a role in our case despite not receiving the last prescribed dose.
To our knowledge, this is the first reported case of PRES on a SARS-CoV-2 infected patient. This case has a probable multifactorial origin: the basal treatment with carfilzomib and the elevation of arterial blood pressure, although not substantial, could have created a susceptible environment in which the disease caused by the new coronavirus acted as a trigger.
On the other hand, verapamil, used mainly as a vasodilator, has reported good results on drug-resistant epilepsy as it inhibits P-glycoprotein, increasing the availability of antiepileptic drugs [4]. Moreover, similar drugs such as nimodipine have been used on the prevention of vasospasm secondary to SVCR and PRES [3].The use of verapamil in this instance was prompt by the CT images, suggestive of PRES, ceasing the focal status epilepticus with an unequivocal temporal correlation between the administration and the clinical response.
We believe this is the first reported case of verapamil as treatment for refractory epilepsy secondary to PRES. The effectiveness of the prescription in this case may be explained by its vasodilator effect, its adjuvant effect on refractory epilepsy, or a combination of both. Further research is crucial to confirm the results.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None.
Footnotes
Would it be possible to enlarge image 2 and 3 to make full use of all the space available? Thank you so much.
References
- 1.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A., et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/s0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu D., Yang X.O. TH17 responses in cytokine storm of COVID-19: an emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cai X., Bhattacharyya S., Plitt A., Raibagkar P., LaBuzetta J.N., Schleicher S.M., et al. Management of posterior reversible encephalopathy syndrome induced by Carfilzomib in a patient with multiple myeloma. J Clin Oncol. 2016;34(2):e1–e5. doi: 10.1200/JCO.2013.49.6166. [DOI] [PubMed] [Google Scholar]
- 4.Lakshmikanthcharan S., Chaitanya Juluri S.K., Nandakumar S.M. Verapamil as an adjuvant treatment for drug-resistant epilepsy. Indian J Crit Care Med. 2018;22(9):680–682. doi: 10.4103/ijccm.IJCCM_250_18. [DOI] [PMC free article] [PubMed] [Google Scholar]