Abstract
Background
The literature indicates that cardiovascular disease (CVD; including stroke), older age, and availability of health care resources affect COVID-19 case fatality rates (CFRs). The cumulative effect of COVID-19 CFRs in global CVD populations and the extrapolated effect on access to health care services in the CVD population in Canada are not fully known. In this study we explored the relationships of factors that might affect COVID-19 CFRs and estimated the potential indirect effects of COVID-19 on Canadian health care resources.
Methods
Country-level epidemiological data were analyzed to study the correlation, main effect, and interaction between COVID-19 CFRs and: (1) the proportion of the population with CVD; (2) the proportion of the population 65 years of age or older; and (3) the availability of essential health services as defined by the World Health Organization Universal Health Coverage index. For indirect implications on health care resources, estimates of the volume of postponed coronary artery bypass grafting, percutaneous coronary intervention, and valve surgeries in Ontario were calculated.
Results
Positive correlations were found between COVID-19 CFRs and: (1) the proportion of the population with CVD (ρ = 0.40; P = 0.001); (2) the proportion of the population 65 years of age or older (ρ = 0.43; P = 0.0005); and (3) Universal Health Coverage index (ρ = 0.27; P = 0.03). For every 1% increase in the proportion of the population 65 years of age or older or proportion of the population with CVD, the COVID-19 CFR was 9% and 19% higher, respectively. Approximately 1252 procedures would be postponed monthly in Ontario because of current public health measures.
Conclusions
Countries with more prevalent CVD reported higher COVID-19 CFRs. Strain on health care resources is likely in Canada.
Résumé
Contexte
La littérature indique que les maladies cardiovasculaires (MCV, incluant les accidents vasculaires cérébraux), l’âge avancé et la facilité d’accès aux ressources de soins de santé ont une incidence sur les taux de létalité (TL) des cas de COVID-19. L’effet cumulatif du TL de la COVID-19 dans l’ensemble de la population atteinte de MCV et l’impact anticipé sur l'accès aux services de santé dans la population atteinte de MCV au Canada ne sont pas entièrement connus. Cette étude a exploré les liens entre les facteurs pouvant influencer le TL des cas de COVID-19 et a estimé le potentiel impact indirect de la COVID-19 sur les ressources de soins de santé au Canada.
Méthodes
Les données épidémiologiques à l’échelle du pays ont été analysées pour étudier la corrélation, l’effet principal et l’interaction entre le TL de laCOVID-19 et : 1) la proportion de la population souffrant de MCV, 2) la proportion de la population ≥ 65 ans, et 3) l’accessibilité des services de santé essentiels tels que définis par l’indice de couverture sanitaire universelle (CSU) de l’Organisation Mondiale de la Santé. Pour les implications indirectes concernant les ressources de santé, des estimations du volume d’opération de pontages coronariens, d'interventions coronariennes percutanées et de chirurgies valvulaires reportées en Ontario ont été calculées.
Résultats
Des corrélations positives ont été trouvées entre le TL de la COVID-19 et 1) la proportion de la population souffrant de MCV (ρ= 0,40, P = 0,001), 2) la proportion de la population ≥ 65 ans (ρ= 0,43, P = 0,0005), et 3) l’indice CSU (ρ= 0,27, P = 0,03). Pour chaque augmentation de 1 % de la proportion de la population ≥ 65 ans ou de la proportion de la population souffrant de MCV, le TL de la COVID-19 était respectivement supérieur de 9 % et 19 %. Environ 1 252 interventions seraient reportées chaque mois en Ontario en raison des mesures de santé publique actuelles.
Conclusions
Les pays où les MCV sont plus répandues ont signalé un TL de la COVID-19 plus élevé. Il est probable que les ressources de soins de santé soient soumises à de fortes contraintes au Canada.
A growing number of publications indicate that underlying cardiovascular disease (CVD; including stroke), older age (65 years or older), and availability of health care resources can affect the risk of fatality from COVID-19.1, 2, 3, 4, 5, 6, 7 Underlying CVD confers up to a 4 times greater COVID-19 mortality risk relative to those without CVD.4,8 Moreover, upwards of 20% of hospitalized COVID-19 patients develop cardiac injury with a mortality rate as high as 51%.4,9 Variation in health care resource availability and accessibility was linked to regional disparities in COVID-19 mortality rates7 and differences in the reporting of COVID-19 test rates might influence the interpretation of case fatality rates (CFRs).10 The cumulative effect of the proportion of the population with CVD, proportion of the population 65 years of age or older, and availability of essential health services on COVID-19 CFRs in global CVD populations is not known.
Further to the immediate effect that an increased risk of COVID-19 mortality will have on individuals with CVD, this pandemic might have long-lasting implications for health care resources supporting CVD populations. Additional strain on the health of CVD populations and health care resources is implicit, because of a combination of factors including postponement of nonurgent CVD medical appointments and procedures to create capacity for COVID-19 patients, adherence to appropriate public health measures, and rationing of personal protective equipment.11,12 The extrapolated effect on access to health care services in the CVD population in Canada has not been reported. This information may inform health care planners on the anticipated changes in health care demand caused by disruption to the continuity of CVD care.
The goal of the Heart and Stroke Foundation of Canada (HSFC) is to work with its partners to expedite knowledge translation and facilitate changes to clinical practice with the aim of improving outcomes for people with CVD. In this study, an analysis of country-level epidemiological data was conducted to explore how the factors of the proportion of the population with CVD, the proportion of the population 65 years of age or older, availability of essential health services as defined by the World Health Organization (WHO) Universal Health Coverage (UHC) index, and COVID-19 test rate interact to affect COVID-19 CFR. Countries with higher proportions of the population with CVD and higher proportions of the population 65 years of age or older may have higher COVID-19 CFRs, and this effect might be modulated by the availability of health care services and test rates. The potential indirect effects of the pandemic on the provision of CVD health care services was determined by estimating the volume of postponed coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), and valve surgeries in Canada’s most populous province. Last, qualitative observations of indirect effects of COVID-19 on CVD populations are briefly discussed.
Methods
Data sources for analysis
COVID-19 CFR
Data on COVID-19 CFR according to country were obtained from global epidemiological data from January 21 to April 30, 2020 extracted from WHO Situation Reports13 and from the Johns Hopkins University Center for Systems Science and Engineering.14 Only countries with at least 60 days since first confirmed cases of COVID-19 were included in this study. The CFR as defined by the WHO is the proportion of reported cases of a specific disease or condition that are fatal within a specified time.
COVID-19 test rate
Data on COVID-19 test rate were obtained for 46 countries from the Our World in Data COVID-19 testing data set.15 Test rates were categorized into 1 of 3 reporting definitions: individuals tested, tests performed, or unclear/unknown. For countries that provided test numbers for individuals tested and tests performed per 100,000, values from the number of individuals tested per 100,000 were used. Test rates for the remaining 15 countries were obtained from Worldometers.info,16 and were classified as unclear/unknown because of the lack of reporting definition.
Proportion of the population with CVD
Data on CVD cases in 2017 according to country were obtained from the Institute for Health Metrics and Evaluation Global Burden of Disease (GBD) Study 2017.17 Data on country-specific population size were obtained from the World Bank18 and United Nations19 for the year 2017 to ensure time period consistency with the GBD CVD data.
Proportion of the population 65 years old or older
Data on country-specific population age distribution were obtained from the World Bank18 and United Nations19 for the year 2017 to ensure time period consistency with the global CVD and health services data.
Affordability and access to health services
The WHO UHC service coverage index20 was used as a measure of availability of essential health services in each country.21 The UHC service coverage index is comprised of 16 tracer indicators, which cover 4 essential health services categories of reproductive, maternal, newborn, and child health; infectious diseases; noncommunicable diseases; and services capacity and access. Across countries, the median value associated with this index was 65 of 100, with a range of 22-86. The UHC index was evaluated as a continuous variable in this study.
Volume of selected CVD surgeries and procedures in Ontario
Canadian Classification of Health Intervention codes were used to capture the volume of selected CVD surgeries and procedures (CABG, PCI, and valve surgery) that occurred between April 1, 2018 to March 31, 2019 from the Canadian Institute for Health Information (CIHI) Discharge Abstract Database (Supplemental Tables S1 and S2). Valve surgery included excision or repair of the tricuspid, mitral, pulmonary, or aortic valves. Parts of this material are on the basis of data and information provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not those of CIHI.
Statistical analyses
The relationships among key variables were assessed using Spearman rank correlations. These were calculated between COVID-19 CFR and: (1) proportion of the population with CVD; (2) proportion of the population 65 years of age or older; (3) UHC index; and (4) COVID-19 test rate. The Spearman rank correlation was chosen because it is nonparametric.
To further explore possible collinearity, a linear regression model was fitted with COVID-19 CFR as the outcome variable, and proportion of the population with CVD, proportion of the population 65 years of age or older, and UHC index as independent variables. All 3 independent variables were continuous.
Separate negative binomial regression models were used to explore the relationship between COVID-19 CFR and the following variables: (1) proportion of the population with CVD; (2) proportion of the population 65 years of age or older; and (3) UHC index. The interactions, including Proportion of the population with CVD × UHC index and Proportion of the population 65 years or older × UHC index were examined in each model, respectively. A Poisson regression model was considered first but because of overdispersion, this approach was not pursued.
Because COVID-19 testing practices influence the interpretation of CFR by varying the denominator of proven cases, a second multiple regression model was applied to a subset of countries (18 of 65) for which COVID-19 test reporting practices were the same as Canada, namely test rate reported by the number of individuals tested per 100,000 as opposed to the number of tests performed per 100,000. As with the previous model, because of collinearity between proportion of the population with CVD and proportion of the population 65 years or older, 2 separate models were tested using negative binomial regression in this subcohort with COVID-19 CFR as the outcome variable: (1) COVID-19 test rate and proportion of the population with CVD; and (2) COVID-19 test rate and proportion of the population 65 years of age or older. All 3 independent variables were continuous. A stepwise selection method was used to determine best fit. UHC index was not included as an independent variable in these 2 models because the UHC index for 15 of the 18 countries was skewed to the upper range (ie, UHC index ≥ 70; Table 1).
Table 1.
UHC indices of countries reporting COVID-19 test rate as the number of individuals tested per 100,000
| Country | UHC index |
|---|---|
| Canada | 89 |
| Denmark | 81 |
| India | 55 |
| Italy | 82 |
| Japan | 83 |
| Luxembourg | 83 |
| Malaysia | 73 |
| Mexico | 76 |
| Nepal | 48 |
| Netherlands | 86 |
| Pakistan | 45 |
| Philippines | 61 |
| Qatar | 68 |
| Russia | 75 |
| Singapore | 86 |
| South Korea | 86 |
| Thailand | 80 |
| United Kingdom | 87 |
Refer to Supplemental Table S3 for UHC index of all of the countries included in this study.
UHC, universal health coverage.
At the time of this study, the expected duration of imposed public health measures was unknown. Data on percentage decrease in CVD procedures were available from the CorHealth Cardiac Registry of Ontario on the volumes of: CABG, PCI, and valve surgery (CorHealth Ontario, unpublished data, 2020). The percentage decrease in activity was calculated by comparing the weeks of March 16 through May 3 in 2019 and 2020, and then applied to historical data from CIHI (fiscal year 2018-2019) to generate an estimate of monthly backlog specific to Ontario. Volumes of procedures reported in fiscal year 2018-2019 were similar to those reported in fiscal year 2017-2018, and thus the former and more recent fiscal year was used as the historical benchmark to estimate the backlog of procedures.
Results
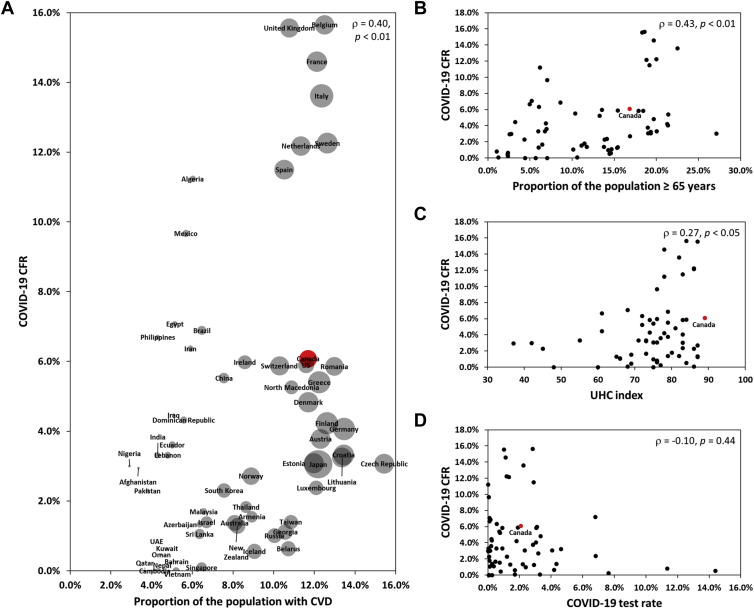
On April 30, 2020, 63 of 176 countries from the Johns Hopkins University data repository had confirmed cases of COVID-19 for at least 60 days (Supplemental Table S3). Spearman correlation analyses generated significant positive correlations of low/moderate magnitude between COVID-19 CFR and proportion of the population with CVD (ρ = 0.40; P = 0.001) and COVID-19 CFR and proportion of the population 65 years of age or older (ρ = 0.43; P = 0.0005). A significant positive correlation of low magnitude was found between COVID-19 CFR and UHC index (ρ = 0.27; P = 0.03; Fig. 1 and Table 2). Of note, the proportion of the population with CVD and the proportion of the population 65 years of age or older were highly correlated (ρ = 0.93; P = 0.0001).
Figure 1.
COVID-19 CFR, proportion of the population with CVD, 65 years of age or older, UHC index, and COVID-19 test rate. Scatter plots of (A) proportion of the population with CVD, including stroke and COVID-19 CFR, (B) proportion of the population 65 years old or older and COVID-19 CFR, (C) UHC service coverage index and COVID-19 CFR, and (D) COVID-19 test rate and COVID-19 CFR. In (A) the size of the bubbles corresponds to the proportion of the population 65 years of age or older. Data points representing Canada are highlighted in red. Spearman correlation coefficients are reported as ρ. Sample size of 63. CFR, case fatality rate; CVD, cardiovascular disease; UHC, universal health coverage; US, United States.
Table 2.
Spearman correlation coefficients
| Variable | 1. COVID-19 CFR | 2. COVID-19 test rate | 3. UHC index | 4. Proportion of the population 65 years old or older | 5. Proportion of the population with CVD |
|---|---|---|---|---|---|
|
-- | ||||
|
−0.10 (P = 0.44) | -- | |||
|
0.27 (P = 0.03) | 0.53 (P < 0.0001) | -- | ||
|
0.43 (P = 0.0005) | 0.37 (P = 0.003) | 0.58 (P < 0.0001) | -- | |
|
0.40 (P = 0.001) | 0.43 (P = 0.0005) | 0.52 (P < 0.0001) | 0.93 (P < 0.0001) | -- |
Coefficients are reported as ρ. UHC service coverage index for Taiwan was unavailable so the UHC service coverage index for China was used. Sample size of 63.
CFR, case fatality rate; CVD, cardiovascular disease including stroke; pop, population; UHC, universal health coverage.
The linear regression revealed a variance inflation factor of 7.5 and 7.9 for the variables proportion of the population with CVD and proportion of the population 65 years of age or older, respectively (Supplemental Table S4). This indicated high collinearity between these variables and identified the need to separate out these predictors to determine their unique relationships to COVID-19 CFR.
A total of 4 negative binomial regression models (1a, 1b, 2a, and 2b) were performed. Model 1a and 1b were used to examine the effect of proportion of the population with CVD and UHC index on COVID-19 CFR (model 1a), as well as proportion of the population 65 years of age or older and UHC index on COVID-19 CFR (model 1b). The contributions of each predictor and their interactions in each model were assessed. In model 1a, neither proportion of the population with CVD nor UHC index emerged as significant predictors of COVID-19 CFR independently (Table 3). The interaction between UHC index and proportion of the population with CVD was marginally significant (interaction β = 0.80 [95% confidence interval (CI), 0.01 to 1.59]; P = 0.05; Table 3). In model 1b, the interaction between proportion of the population 65 years of age or older and UHC index on COVID-19 CFR was not significant (interaction β = 0.32 [95% CI, −0.11 to 0.76]; P = 0.15; Table 3).
Table 3.
Negative binomial regression models with outcome variable COVID-19 CFR
| β coefficient | SE | 95% CIs | χ2 | P | |
|---|---|---|---|---|---|
| Model 1a: log(COVID-19 deaths) = offset + proportion of the population with CVD and UHC Index | |||||
| UHC index | −0.03 | 0.03 | −0.08 to 0.02 | 1.67 | 0.20 |
| Proportion of the population with CVD | −54.35 | 31.30 | −115.7 to 6.7 | 3.02 | 0.08 |
| UHC index∗ (proportion of the population with CVD) | 0.80 | 0.40 | 0.01 to 1.59 | 3.98 | 0.05 |
| Model 1b: log(COVID-19 deaths) = offset + proportion of the population 65 years old or older + UHC index | |||||
| UHC Index | −0.01 | 0.02 | −0.05 to 0.02 | 0.51 | 0.48 |
| Proportion of the population 65 years old or older | −20.90 | 17.70 | −55.58 to 13.79 | 1.39 | 0.24 |
| UHC Index∗ (Proportion of the population 65 years old or older) | 0.32 | 0.22 | −0.01 to 0.76 | 2.13 | 0.15 |
| Model 2a: log(COVID-19 deaths) = offset + test rate + proportion of the population with CVD | |||||
| COVID-19 test rate | −0.39 | 0.16 | −0.69 to −0.08 | 6.15 | 0.01 |
| Proportion of the population with CVD | 17.8 | 6.4 | 5.29 to 30.26 | 7.79 | 0.005 |
| Model 2b: log(COVID-19 deaths) = offset + test rate + proportion of the population 65 years old or older | |||||
| COVID-19 test rate | −0.36 | 0.15 | −0.66 to −0.06 | 5.57 | 0.02 |
| Proportion of the population 65 years old or older | 8.8 | 3.2 | 2.55 to 15.12 | 7.60 | 0.006 |
Parameter estimates are reported as β coefficients; offset = log(COVID-19 cases). Sample size is 63 for model 1a and 1b; sample size is 18 for model 2a and 2b.
CFR, case fatality rate; CI, confidence interval; CVD, cardiovascular disease including stroke; SE, standard error; UHC, universal health coverage.
UHC service coverage index for Taiwan was unavailable so the UHC service coverage index for China was used.
In model 2 test rate was added as an independent variable and included only countries that reported the number of individuals tested per 100,000. There were 18 countries included in this analysis. Two separate models (models 2a and 2b) were used to explore the effect of proportion of the population with CVD and test rate (model 2a), and proportion of the population 65 years of age or older and test rate (model 2b) on COVID-19 CFR. In model 2a, test rate (β = −0.39 [95% CI, −0.70 to −0.08]; P = 0.01; Table 3) and proportion of the population with CVD (β =17.77 [95% CI, 5.29 to 30.26]; P = 0.005; Table 3) were significant contributors to COVID-19 CFR. In model 2b, test rate (β = −0.36 [95% CI, −0.66 to −0.06]; P = 0.02; Table 3) and the proportion of the population 65 years of age or older (β = 8.8 [95% CI, 2.55 to 15.12]; P = 0.006; Table 3) were significant contributors to COVID-19 CFR.
The potential effect on health care resources in Ontario was estimated. In fiscal year 2018-2019, of more than 100,000 hospitalizations for CVD, 8485 CABG procedures, 20,077 PCI procedures, and 7212 valve surgeries were completed on patients with CVD in the province of Ontario. The percentage decrease in CABG, PCI, and valve surgery at cardiac centres in Ontario, calculated by comparing the weeks of March 16 through May 3 in 2019 and 2020, was 42% for CABG, 37% for PCI, and 45% for valve surgery. By applying the percentage decrease to historical CIHI data from fiscal year 2018-2019, approximately 297 CABG, 703 PCI, and 252 valve surgeries, for a total of 1252 procedures, would be postponed per month because of current COVID-19 public health measures (Table 4).
Table 4.
2018-2019 Volumes of CABG, PCI, and valve surgery and expected reductions in activity in Ontario
| Procedure | 2018-2019 volume | Number of procedures per month | Estimated reduction between the weeks of March 16 and May 3, 2020 | Forecasted backlog of procedures per month |
|---|---|---|---|---|
| CABG | 8485 | 707 | 42% | 297 |
| PCI | 20,077 | 1673 | 37% | 703 |
| Valve surgery | 7212 | 601 | 45% | 252 |
Valve surgery includes repair or excision of tricuspid, pulmonary, mitral, and aortic valves, and does not include transcatheter aortic valve implantation.
CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
Discussion
To date, most publications on COVID-19 have been limited to cohorts from China, Italy, and the United States. Incorporating data from 63 countries, the findings from this study suggest that the cumulative effect and interaction of the proportion of the population with CVD, the proportion of the population 65 years of age or older, and availability of health care services on COVID-19 CFR is complex. Regression modelling showed a nuanced pattern of relationships between these variables. Surprisingly, the proportion of the population with CVD was only related to higher COVID-19 CFR in countries with a higher UHC index, such as Canada. Although further studies are necessary to fully understand this unexpected finding, one possible explanation is that more available essential health care services in these countries might lead to more individuals surviving and living with CVD relative to countries with less health care availability. Indeed, three-quarters of global CVD deaths take place in low- and middle-income countries,22 but CVD accounts for a higher percent of disability-adjusted life-years in high-income than in low-income countries.23 This in turn may lead to more individuals living with complex CVD characterized by multimorbidity and greater risk of poorer outcomes from COVID-19. Overall, these results suggest that public health measures and COVID-19 management specific to CVD populations in Canada are likely necessary because of the relatively high proportion of the population with CVD.
When evaluating the relationship for countries such as Canada that report COVID-19 test rate as the number of people tested per 100,000, COVID-19 test rate alone negatively affected COVID-19 CFR. That is, countries that conducted more COVID-19 tests had a lower COVID-19 CFR. For every 1% increase in COVID-19 test rate, one would expect the COVID-19 CFR to be 4% lower. This may be driven by causative and correlative factors. Countries that have higher test rates for COVID-19 are likely capturing a greater number of milder and asymptomatic cases, increasing the size of the denominator used to calculate the CFR and thereby reducing the CFR. These countries might have more available health care resources to treat people infected with SARS-CoV-2. However, when evaluating the interactions between test rate and the proportion of the population with CVD or the proportion of the population 65 years of age or older, no interactions were found. This means, independent of test rate, higher COVID-19 CFRs were observed in countries whose populations had higher proportions of CVD and individuals 65 years of age or older. For every 1% increase in the proportion of the population 65 years of age or older, or proportion of the population with CVD, one would expect the COVID-19 CFR to be 9% and 19% higher, respectively. Although the nature of the positive effect of CVD on COVID-19 CFR cannot yet be fully characterized at this early stage of the pandemic, postulated mechanisms include predisposition to cardiac injury, inflammation, hypoxia, and hypercoagulability.9
In addition to the large number of deaths, the COVID-19 pandemic may put a strain on CVD health care resources and the health of the CVD population. Emergency public health measures, staff redeployment, and shifts in health care resources are resulting in the postponement of nonurgent procedures: preliminary estimates from this study, which only accounted for CABG, PCI, and valve surgery, already indicate a potential backlog of > 1200 procedures each month in Ontario alone. Because Ontario represents only 38% of Canada by population, the COVID-19 pandemic will have a notable effect on health care resources nationally. As provinces restart elective surgeries and procedures while health care resources continue to support treatment of existing and new patients with COVID-19, as well as urgent CVD care, careful consideration of health care system planning is warranted to manage the imbalance between health care capacity and demand created as the direct and indirect consequences of the COVID-19 pandemic. Proactive planning of reinstitution of CVD care resources will be crucial to address this backlog. Further challenges to CVD management might include complications in patients who have delayed medical care because of COVID-19 fears. Anecdotal data suggest delayed presentation of CVD emergencies by patients because of fear to seek medical attention during the pandemic. A significant increase in the time from symptom onset to first medical contact has been reported in ST-elevation myocardial infarction patients.24,25 These delays can further worsen their conditions, leading to the need for more complex care and greater risk with interventions. Moreover, delays to the rapid triage of CVD patients are possible.12
Study limitations
It is important to note that the results of all correlation analyses and regression modelling are on the basis of country-level data and the relationships reported between variables should not be generalized to the individual patient level. There were several limitations to this study. First, male sex has been reported to be a risk factor for COVID-19 mortality.26 However, country-specific sex-disaggregated data for COVID-19 CFRs were unavailable at the time of this study and including sex as an independent variable in the analyses was not possible. Second, there was significant variation in how countries report COVID-19 test rate, which limited our ability to evaluate the full effect of this variable. Moreover, CFR is an indicator of disease fatality that does not consider differences in case ascertainment, and specificity and sensitivity of tests, which confounds the interpretation of CFR-based data. Third, although the WHO has provided guidance for standardized reporting of COVID-19-related deaths, countries might deviate from these guidelines and reporting variance was possible. Fourth, although this study provides insights into the potential implications of COVID-19, the small sample size of the country-level epidemiological data set at this early stage of the pandemic limits the estimation precision of the regression coefficients. Last, there were variations in how procedures were captured in the CIHI and CorHealth Cardiac Registry databases.
Conclusions
Our findings provide insight into the direct and indirect implications of COVID-19 on CVD populations and health care resources. Among countries with more available health care resources, a higher proportion of the population with CVD was related to higher COVID-19 CFR. Public health measures and COVID-19 management specific to CVD populations in Canada are thereby essential because of the relatively high proportion of the population with CVD. The pandemic has disrupted the provision of health care services for patients with CVD in Canada. This information may be of benefit to health care planners to guide reactive and proactive measures in the management of the COVID-19 pandemic in Canada, the planning for health system recovery, and triaging burgeoning wait lists.
Acknowledgements
The authors thank CorHealth Ontario, Brittany Gould, Joon Lee, Lavanya Uruthiramoorthy, and Norine Foley for their assistance.
Funding Sources
The authors have no funding sources to declare.
Disclosures
R.H.S. receives support from an HSFC Clinician-Scientist Award. T.S.F. is supported by an HSFC National New Investigator Award, a Michael Smith Foundation for Health Research Health-Professional Investigator Award, and a Vancouver Coastal Health Research Institute Clinician-Scientist award, and receives in-kind study medication from Bayer Canada. A.K. receives support from the Sauder Family and HSFC Chair in Cardiology and the Paul Brunes Chair in Heart Rhythm Disorders (Vancouver, British Columbia). The other authors have no conflicts of interest to disclose.
Footnotes
Ethics Statement: The present article adheres to ethical guidelines.
See page 271 for disclosure information.
To access the supplementary material accompanying this article, visit CJC Open at https://www.cjcopen.ca/ and at https://doi.org/10.1016/j.cjco.2020.06.003.
Supplementary Material
References
- 1.Lippi G., Wong J., Henry B.M. Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med. 2020;130:304–309. doi: 10.20452/pamw.15272. [DOI] [PubMed] [Google Scholar]
- 2.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arentz M., Yim E., Klaff L. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) [e-pub ahead of print]. JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.1017 accessed April 15, 2020. [DOI] [PMC free article] [PubMed]
- 5.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson S., Hirsch J.S., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8 doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen R., Liang W., Jiang M. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China [e-pub ahead of print]. Chest. https://doi.org/10.1016/j.chest.2020.04.010 accessed April 15, 2020. [DOI] [PMC free article] [PubMed]
- 9.Shi S., Qin M., Shen B. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China [e-pub ahead of print]. JAMA Cardiol. https://doi.org/10.1001/jamacardio.2020.0950 accessed April 15, 2020. [DOI] [PMC free article] [PubMed]
- 10.Kim D.H., Choe Y.J., Jeong J.Y. Understanding and interpretation of case fatality rate of coronavirus disease 2019. J Korean Med Sci. 2020;35:e137. doi: 10.3346/jkms.2020.35.e137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Urbach D.R., Martin D. Confronting the COVID-19 surgery crisis: time for transformational change. CMAJ. 2020;192 doi: 10.1503/cmaj.200791. E586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Driggin E., Madhavan M.V., Bikdeli B. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization Novel Coronavirus (2019-nCoV) Situation Reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available at:
- 14.John Hopkins University & Medicine. Johns Hopkins Coronavirus Resource Center COVID-19 World Map. https://coronavirus.jhu.edu/map.html Available at:
- 15.Our World in Data. Hassell J, Mathieu E, Beltekian D, et al. Coronavirus (COVID-19) Testing. Available at: https://ourworldindata.org/covid-testing. Accessed May 1, 2020.
- 16.Worldometer Reported Cases and Deaths by Country, Territory, or Conveyance. https://www.worldometers.info/coronavirus/#countries Available at:
- 17.GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017 [errata in: 2018;392:2170, 2019;393:e44] Lancet. 2018;392 doi: 10.1016/S0140-6736(18)32203-7. 1736-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The World Bank Population ages 65 and above (% of total population) https://data.worldbank.org/indicator/sp.pop.65up.to.zs Available at:
- 19.United Nations, Department of Economic and Social Affairs, Population Division World Population Prospects 2019, Online Edition. https://population.un.org/wpp/Download/Standard/Population Available at:
- 20.World Health Organization The Global Health Observatory. Universal Health Coverage. apps.who.int/gho/cabinet/uhc.jsp Available at:
- 21.Hogan D.R., Stevens G.A., Hosseinpoor A.R., Boerma T. Monitoring universal health coverage within the Sustainable Development Goals: development and baseline data for an index of essential health services. Lancet Glob Health. 2018;6:e152–e168. doi: 10.1016/S2214-109X(17)30472-2. [DOI] [PubMed] [Google Scholar]
- 22.Our World in Data Total Confirmed Deaths Due to COVID-19 Per Million People. https://ourworldindata.org/grapher/total-covid-deaths-per-million Available at:
- 23.World Health Organization The Atlas of Heart Disease and Stroke. https://www.who.int/cardiovascular_diseases/resources/atlas/en Available at:
- 24.Tam C.C.F., Cheung K.S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solomon M.D., McNulty E.J., Rana J.S. The COVID-19 pandemic and the incidence of acute myocardial infarction [e-pub ahead of print]. N Engl J Med. https://doi.org/10.1056/NEJMc2015630 accessed April 15, 2020. [DOI] [PubMed]
- 26.Jin J.M., Bai P., He W. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.