Abstract
Objective
To highlight the increased risk of hemorrhagic stroke secondary to postulated COVID-19 mediated vasculopathy with concomitant ECMO related bleeding complications.
Background
COVID-19 has shown to be a systemic illness, not localized to the respiratory tract and lung parenchyma. Stroke is a common neurological complication. In particular, critically ill patients on ECMO are likely at higher risk of developing hemorrhagic stroke.
Case Presentation
38-year-old man presented with fever, cough, and shortness of breath. Due to severe respiratory failure, he required ECMO support. Subsequently, he was found to have left temporal intraparenchymal hemorrhage. Overall, his clinical course improved, and he was discharged with minimal neurological deficits.
Conclusion
Although intracranial hemorrhage is a known complication of ECMO, patients with COVID-19 infection may be at a higher risk of cerebrovascular complications due to vasculopathy.
Keywords: COVID-19, hemorrhagic stroke, ECMO complications, intracranial hemorrhage on heparin
Introduction
To date, stroke is reported to be one of the most common neurological complications of COVID-19 infection. Proposed mechanisms of cerebrovascular events include a pro-inflammatory state, endothelial dysfunction, and thrombosis in micro- and macro-vasculature.1 , 2 Patients with COVID-19 infection may develop severe acute respiratory distress syndrome (ARDS) and require ECMO support as a life-saving measure, which is accompanied with risk of bleeding namely due to use of anticoagulation. Here, we present a case of hemorrhagic stroke in a patient with severe ARDS related to COVID-19 requiring ECMO.
Case Presentation
38-year-old, previously healthy man was admitted to our hospital with fever, cough, and shortness of breath. He tested positive for both parainfluenza-2 and COVID-19. CT chest showed bilateral diffuse reticulonodular infiltrates. Patient's respiratory status worsened requiring mechanical ventilation and eventually ECMO support with continuous heparin infusion.
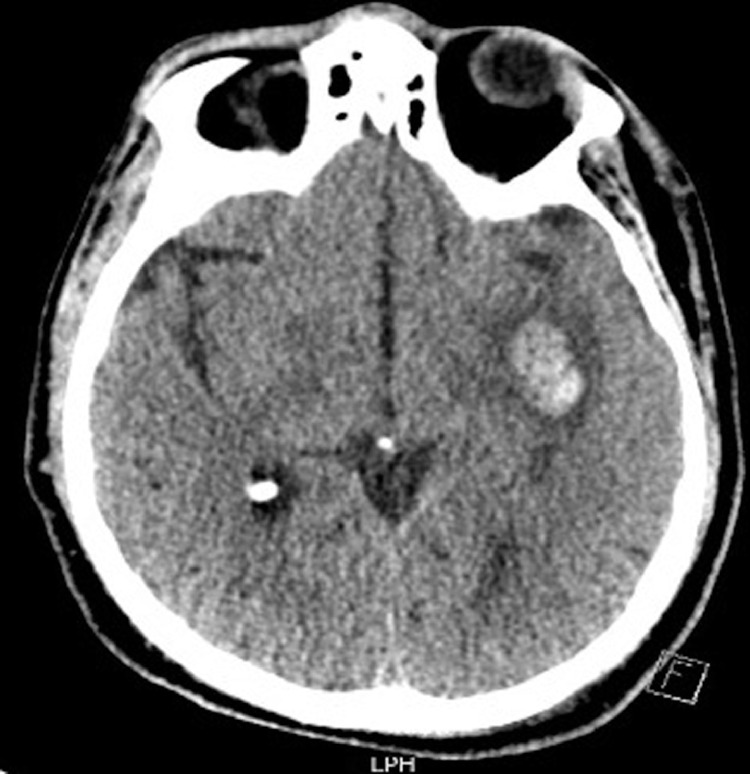
Other forms of therapy included course of Hydroxychloroquine, Azithromycin, and a dose of Tocilizumab. Patient became encephalopathic and a brain CT demonstrated a 2.6 cm left sub-insular parenchymal hemorrhage (Fig 1 ). Brain CT angiography showed no vascular abnormalities. Neurological examination revealed mild right facial weakness and dysarthria. Continuous EEG monitoring showed generalized slowing without EEG seizures. Follow up brain CT demonstrated resolution of hemorrhage. Overall, patient showed significant clinical improvement.
Figure 1.
Brain CT without contrast demonstrating left sub-insular intraparenchymal hemorrhage with surrounding vasogenic edema.
Discussion
Intraparenchymal hemorrhages have been reported with ECMO. Postulated mechanisms include disruption in hemostasis likely potentiated by concomitant anticoagulation during ECMO, a pro-inflammatory state, which in this case can also be attributed to COVID-19, and hemodynamic dysfunction with loss of cerebral perfusion autoregulation.3
Thus, there may be dual pathogenesis resulting in hemorrhage: 1) COVID-19 related vasculopathy with endothelial damage of small vessels perhaps making them more susceptible to rupture. 2) ECMO related bleeding risks as mentioned above.
We aim to shed light on hemorrhagic stroke as one of the major neurological complications of COVID-19 infection in patients on ECMO. In these patients, a low threshold should be maintained to evaluate for intracranial hemorrhage.
References
- 1.Varga Z., Flammer A.J., Steiger P. Endothelial cell infection and endotheliitis in COVID-19. Lancet (London, England) 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avula A., Nalleballe K., Narula N. COVID-19 presenting as stroke. Brain, behavior, and immunity. 2020 doi: 10.1016/j.bbi.2020.04.077. S0889-1591(20)30685-1. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fletcher-Sandersjöö A., Thelin E.P., Bartek J. Incidence, Outcome, and Predictors of Intracranial Hemorrhage in Adult Patients on Extracorporeal Membrane Oxygenation: A Systematic and Narrative Review. Frontiers in neurology. 2018;9:548. doi: 10.3389/fneur.2018.00548. [DOI] [PMC free article] [PubMed] [Google Scholar]