Abstract
To assess the effect of COVID-19 on health care, this study compares admissions data from the Veterans Affairs system for overall admissions and for 6 common emergencies immediately before and for 6 weeks during the pandemic.
Anecdotal reports suggest hospitalizations, including for emergency conditions and elective procedures, have declined during the coronavirus disease 2019 (COVID-19) pandemic.1 Reduced hospitalizations for conditions requiring timely treatment may have significant public health consequences.
The Department of Veterans Affairs (VA) is the largest health system in the US. The VA has ensured continuously available treatment for emergency conditions and canceled elective procedures during the COVID-19 pandemic.2 This study evaluated changes in the number of admissions to VA hospitals overall and for 6 common emergency conditions during the pandemic.
Methods
We analyzed data from the VA’s Corporate Data Warehouse, a national repository of electronic health records from visits to any VA facility.3 We describe trends in VA hospitalizations overall, for 6 common emergency conditions, and for COVID-19 during the first 16 weeks of 2019 and 2020 among a previously established cohort of adults enrolled in VA care between 2008 and 2018. We compared the number and demographic characteristics of patients hospitalized during weeks 5 to 10 (January 29 to March 10) and weeks 11 to 16 (March 11 to April 21) of 2020 overall, among demographic subgroups, and by International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) principal diagnosis codes I60-I69 for stroke, I21-I22 for myocardial infarction, I50 for heart failure, J44 for chronic obstructive pulmonary disease (COPD), K35-K37 for appendicitis, and J10-J18 for pneumonia. Incidence rate ratios (IRRs) comparing daily hospitalization counts during weeks 11 to 16 of 2020 vs January 1, 2019, through week 10 of 2020 were estimated using Poisson regressions that adjusted for seasonal variation and secular trends with week-of-year and year fixed effects.
Analyses were performed using Stata version 15 (StataCorp). The institutional review board at VA New York Harbor Healthcare System approved this study and waived patient informed consent.
Results
The number of patients in our cohort admitted to VA inpatient facilities decreased from 77 624 in weeks 5 to 10 of 2020 to 45 155 in weeks 11 to 16, a reduction of 41.9% (IRR, 0.57; 95% CI, 0.51-0.64) (Figure and Table). The mean age was 66.6 years (SD, 14.0 years), with 93.5% men, 69.0% white, and 24.6% black. The characteristics and case severity of patients admitted during weeks 5 to 10 vs weeks 11 to 16 of 2020 were similar (Table).
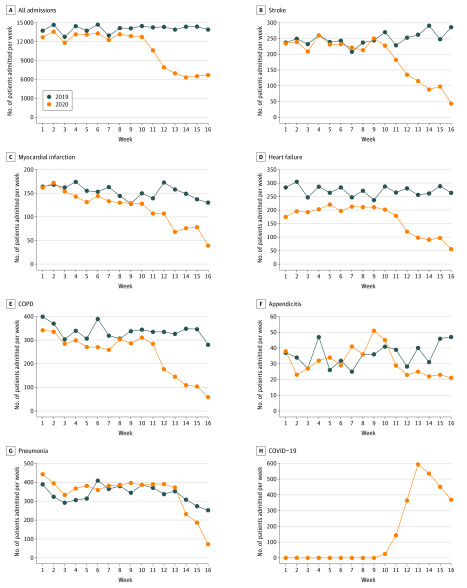
Figure. Trends in the Number of Patients Admitted to Veterans Affairs Inpatient Facilities in 2019 and 2020.
We used the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes for the principal diagnosis. See the Methods section for codes. The 2482 admitted patients who tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; 99% determined by nasopharyngeal swabs) were considered to have coronavirus disease 2019 (COVID-19); their most common principal diagnoses included 614 for emergency use (ICD-10 U07.1, activated at the VA for COVID-19 on April 1, 2020); 474, ICD-10 code not listed; 344, viral pneumonia, not elsewhere classified (ICD-10 J12); 237, other sepsis (ICD-10 A41); and 168, respiratory failure, not elsewhere classified (ICD-10 J96).
Table. Characteristics of Patients Admitted to Veterans Affairs Inpatient Facilities During Weeks 5 Through 10 vs Weeks 11 Through 16 of 2020.
| Characteristics | No. (%) of patients | Incidence rate ratio (95% CI)a | ||
|---|---|---|---|---|
| January 29-March 10, weeks 5-10 | March 11-April 21, weeks 11-16 | Difference in No. of patients admitted (% change) | ||
| Overall | 77 624 | 45 115 | −32 509 (−41.9) | 0.57 (0.51-0.64) |
| Sex | ||||
| Women | 4897 (6.3) | 2769 (6.1) | −2128 (−43.5) | 0.57 (0.50-0.65) |
| Men | 72 757 (93.7) | 42 346 (93.9) | −30 411 (−41.8) | 0.57 (0.51-0.64) |
| Age, y | ||||
| 18-39 | 4837 (6.2) | 2833 (6.3) | −2004 (−41.4) | 0.60 (0.52-0.68) |
| 40-59 | 14 603 (18.8) | 8724 (19.3) | −5879 (−40.3) | 0.60 (0.53-0.69) |
| 60-79 | 47 124 (60.7) | 27 209 (60.3) | −19 915 (−42.3) | 0.56 (0.51-0.64) |
| ≥80 | 11 060 (14.3) | 6349 (14.1) | −4711 (−42.6) | 0.56 (0.51-0.62) |
| Race/ethnicityb | ||||
| American Indian/Alaska Native | 562 (0.7) | 391 (0.9) | −171 (−30.4) | 0.67 (0.58-0.77) |
| Asian | 390 (0.5) | 244 (0.5) | −146 (−37.4) | 0.73 (0.63-0.85) |
| Black or African American | 18 631 (24.0) | 11 594 (25.7) | −7037 (−37.8) | 0.62 (0.56-0.69) |
| Native Hawaiian or other Pacific Islander | 606 (0.8) | 365 (0.8) | −241 (−39.8) | 0.57 (0.47-0.69) |
| White | 54 193 (69.8) | 30 617 (67.8) | −23 576 (−43.5) | 0.56 (0.49-0.63) |
| Other | 3242 (4.2) | 1904 (4.2) | −1338 (−41.3) | 0.57 (0.51-0.65) |
| Hispanic/Latino | 5004 (6.5) | 2963 (6.6) | −2041 (−40.8) | 0.57 (0.51-0.67) |
| Married | 32 240 (41.5) | 17 624 (39.1) | −14 616 (−45.3) | 0.54 (0.47-0.61) |
| Hospitalizations | ||||
| Stroke | 1375 (1.7) | 661 (1.5) | −714 (−51.9) | 0.44 (0.33-0.59) |
| Myocardial infarction | 795 (1.0) | 475 (1.1) | −320 (−40.3) | 0.59 (0.50-0.69) |
| Heart failure | 1255 (1.6) | 639 (1.2) | −616 (−49.1) | 0.53 (0.42-0.67) |
| COPD | 1701 (2.2) | 877 (1.9) | −824 (−48.4) | 0.51 (0.38-0.68) |
| Appendicitis | 236 (0.3) | 134 (0.3) | −102 (−56.7) | 0.56 (0.45-0.70) |
| Pneumonia | ||||
| With SARS-CoV-2 | 2290 (3.0) | 1641 (3.6) | −649 (−28.3) | 0.79 (0.65-0.95) |
| Without SARS-CoV-2 | 2289 (2.9) | 1244 (2.8) | −1045 (−45.7) | 0.61 (0.49-0.77) |
| Case severityc | ||||
| In-hospital death | 149 (2.1) | 90 (2.2) | ||
| Length of stay, mean (SD), dd | 5.0 (2.8) | 5.0 (2.8) | ||
| MS-DRG weight, mean (SD)e | 1.6 (1.1) | 1.6 (1.2) | ||
| No. of comorbidities, mean (SD) | 28.7 (12.4) | 28.9 (12.8) | ||
| ≥1 Procedure | 1323 (17.4) | 654 (16.4) | ||
Abbreviations: COPD, chronic obstructive pulmonary disease; MS-DRG, medical severity diagnosis related group; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Estimated using a Poisson regression model with the dependent variable the daily count of hospitalizations and independent variable exposure to the timing of the pandemic (a binary variable equal to 1 during weeks 11-16 of 2020 and equal to 0 otherwise), with adjustment for seasonality using a week-of-year fixed effect and for secular trends using a year fixed effect. Huber-White standard errors were clustered at the week-year level.
Self-reported and defined by participants; data were used to compare demographic characteristics across exposure groups and over time. Other includes more than 1 race, unknown by patient, declined to answer, or missing.
Case severity measures were calculated for stroke, myocardial infarction, heart failure, COPD, appendicitis, and pneumonia excluding admissions of patients testing positive for SARS-CoV-2 (398 for principal diagnosis of pneumonia; 20 for COPD; 15 for heart failure; 9 for stroke; 6 for myocardial infarction; and 1 for appendicitis).
The mean length of stay is the mean length of stay for admissions in each MS-DRG. Admissions are categorized on the principal diagnosis, up to 25 additional diagnoses, up to 25 procedures performed during the stay, and in some cases age, sex, and discharge status of the patient.
MS-DRG weights represent the average resources required to care for cases in that particular MS-DRG, relative to the average resources used to treat cases in all MS-DRGs.
The number of patients admitted in weeks 5 to 10 vs weeks 11 to 16 of 2020 with a principal diagnosis of stroke decreased from 1375 to 661 (−51.9%; IRR, 0.44; 95% CI, 0.33-0.59), for myocardial infarction from 795 to 475 (−40.3%; IRR, 0.59; 95% CI, 0.50-0.69), for COPD from 1701 to 877 (−48.4%; IRR, 0.51; 95% CI, 0.38-0.68), for heart failure from 1255 to 639 (−49.1%; IRR, 0.53; 95% CI, 0.42-0.67), and for appendicitis from 236 to 134 (−56.7%; IRR, 0.56; 95% CI, 0.45-0.70). In contrast, the number of patients admitted overall and for each condition did not decline during the same period of 2019. For pneumonia, admissions decreased during weeks 11 to 16 by −13.7% in 2019 and by −28.3% in 2020 (IRR, 0.79; 95% CI, 0.65-0.95); when excluding patients who tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), pneumonia admissions decreased by −45.7% in 2020 (IRR, 0.61; 95% CI, 0.49-0.77). Among patients admitted during weeks 11 to 16 of 2020, 2458 tested positive for SARS-CoV-2 vs 26 during weeks 5 to 10.
Discussion
Between March 11 and April 21, 2020, 42% fewer patients were admitted to VA inpatient facilities compared with the preceding 6 weeks, including for conditions generally requiring emergency treatment. The percentage decrease in admissions for conditions generally requiring emergency treatment was greater or similar in magnitude to the decrease in admissions overall and is unlikely to be attributable to declines in elective surgeries or disease incidence related to reduced stress or lower exposure to other pathogens or pollution. Rather, many patients may be avoiding hospitals to minimize risk of SARS-CoV-2 infection.
Limitations of this study include the VA population, which may not be generalizable, and use of a cohort first enrolling in VA care prior to 2019. However, comparatively few patients first enrolled later. Furthermore, the clinical consequences of decreased hospitalizations remain unknown and warrant longer-term studies using out-of-hospital mortality data. Nevertheless, the reduction in admissions observed should raise serious concerns about the well-being and health outcomes of patients who are not receiving inpatient care for conditions that require emergency treatment.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med. Published online April 17, 2020. doi: 10.1056/NEJMms2009984 [DOI] [PubMed] [Google Scholar]
- 2.COVID-19 response plan—incident-specific annex to the VHA high consequence infection (HCI) base plan. Published March 23, 2020. Accessed May 12, 2020. https://www.va.gov/opa/docs/VHA_COVID_19_03232020_vF_1.pdf
- 3.Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi: 10.1377/hlthaff.2014.0054 [DOI] [PubMed] [Google Scholar]