Abstract
Purpose
To evaluate the selected biomechanical differences of a double-row trans-osseous equivalent rotator cuff repair with a knotless versus knot-tying medial row using suture tape in regard to repair displacement, stiffness, and ultimate load to failure.
Methods
In 16 fresh-frozen human shoulders (8 matched pairs), double-row rotator cuff repairs were performed with medial-row mattress knots (MK) on one side, the other without (NK). Two DVRT (Differential Variable Reluctance Transducer) sensors were attached between the humerus and 3 mm above the repair site and were used to measure the displacement across the repair during cycling. The biomechanical parameters measured were repair displacement, stiffness, and ultimate load to failure. The supraspinatus was loaded in a similar fashion to previously described protocol using cyclic loading and load to failure testing.1
Results
All data from paired specimens were compared using paired Student t tests. No statistically significant difference (SSD) in displacement across the repair over the 200 cycles of the test was noted between the two groups (MK = 0.591 ± 0.501 mm; NK = 0.439 ± 0.417 mm, p = 0.618). No SSD in stiffness was noted between the two groups (MK = 32.87 ± 6.31 N/mm; NK = 27.98 ± 9.69 N/mm, p = 0.120). No SSD in ultimate load to failure was noted between the two groups (MK = 501.2 ± 126.1 N; NK = 416.8 ± 120.0 N, p = 0.116).
Conclusion
There was no statistically significant different between knotless versus knotted medial row double row rotator cuff repair constructs using suture tape in regard to displacement across the repair site, stiffness and ultimate load to failure. Despite previous evidence suggesting inferiority of knotless medial row technique using suture constructs, this evidence may support the biomechanical equivalency of knotless medial row technique using suture tape.
Keywords: Double row, Rotator cuff, Knotless fixation, Suture tape
1. Introduction
Arthroscopic rotator cuff repair is a reliable means for relieving shoulder pain and restoring function in patients with rotator cuff tears.2 Techniques for rotator cuff tear repair have evolved from single-to a double-row repair due to positive clinical and biomechanical evidence.3, 4, 5, 6, 7, 8 However, high re-tear rates were being observed by clinicians and researchers after double-row rotator cuff repair.9,10 Striving to improve structural integrity, modifications were made to the standard double-row repair techniques. Medial suture limbs were interconnected with lateral suture anchors, creating a more anatomical suture bridge construct, essentially compressing the tendon to its native footprint. (“transosseous-equivalent repair”).11, 12, 13, 14, 15 The SpeedBridge (Arthrex - Naples, FL) technique allows a knotless lateral row fixation by utilizing an interference fit of sutures from the medial row, simplifying double-row suture-bridge fixation. Rotator cuff tissue failure at the medial suture-tendon interface has subsequently become one of the primary mechanisms of repair failure.10,16, 17, 18, 19, 20 Several theories have developed regarding this mode of failure including impedance of vascular inflow16,19 and increased stress formation at the level of the medial knots.7,10 More recently, wider suture material has been developed in order to spread the force of compression over a larger surface area of the repaired cuff tendon, preventing suture cut through.15,21 A recent described suture technique is the knotless, double row, transosseous equivalent suture bridge using suture tape.15,22 This technique aims to reduce medial row rotator cuff failures by eliminating the medial knots while adding the benefits of suture tape including reduced suture cut through and self-reinforcement (shear stress converted to compressive force). Previous studies have demonstrated the biomechanical inferiority of a knotless medial row in double-row suture anchor fixation using No. 2 FiberWire (Arthrex, Naples, Fla).23, 24, 25, 26 Few biomechanical studies have evaluated the biomechanical properties of double-row suture-bridging constructs using FiberTape (Arthrex, Naples, Fla) with knotless versus knot-tying medial row of suture anchors in regards to footprint contact area, force, pressure, and gap formation.26,27
The purpose of this study is to evaluate biomechanical differences of a double-row trans-osseous equivalent rotator cuff repair with a knotless versus knot-tying medial row using suture tape in regard to repair displacement at the medial row fixation point, stiffness, and ultimate load to failure. Our hypothesis is that rotator cuff repairs with a completely knotless suture tape construct without medial row knots will have inferior biomechanical parameters in repair displacement at the medial row fixation point, stiffness, and ultimate load to failure of the repair.
2. Study design
Controlled laboratory study.
3. Materials and methods
16 fresh-frozen cadavers (8 matched pairs) were used for this study. Specimens with preexisting rotator cuff tears were excluded leaving 6 matched pairs for analysis. Specimen were kept frozen and thawed at room temperature for the dissection. All specimen were kept refrigerated to avoid freeze-thaw cycles between dissection, repair, and testing. The shoulders were dissected, removing all structures except for the rotator cuff muscles. The supraspinatus, infraspinatus, and subscapularis were sharply elevated from their muscle origins. The joint capsule was cut freeing the humerus from the scapula, leaving the humeral rotator cuff attachments intact. A full-thickness tear of the supraspinatus was created by sharp dissection at the footprint. All repairs were made by a sports medicine fellowship trained Orthopaedic Surgeon. Repairs were made using a double-row construct. All repairs used Arthrex 4.75 mm SwiveLock anchors with FiberTape for the medial row and Arthrex 4.75 mm SwiveLock anchors for the lateral row (Arthrex, Naples, Fla). After punching and placing the medial row anchors, FiberTape was passed medially using a Scorpion FastPass suture passer (Arthrex, Naples, Fla) for each medial row anchor. For the knotted medial row group, both limbs of the inner FiberWire suture were passed just lateral to the FiberTape from the same anchor, one anterior and one posterior (Fig. 1, Fig. 2). These were tied using a sliding locking knot to simulate in vivo repair. The tails were then cut. For the knotless repair, the inner FiberWire suture was removed from the anchor and not used. A lateral row was then created using the same technique for both groups. Once the pilot holes were punched into the lateral aspect of the greater tuberosity, one FiberTape from the anterior medial row anchor and one from the posterior medial row anchor was placed into each lateral row anchor. Inner sutures from the lateral row anchors were removed and excess FiberTape cut.
Fig. 1.
Placement of double row suture tape and medial row configuration at the medial footprint.
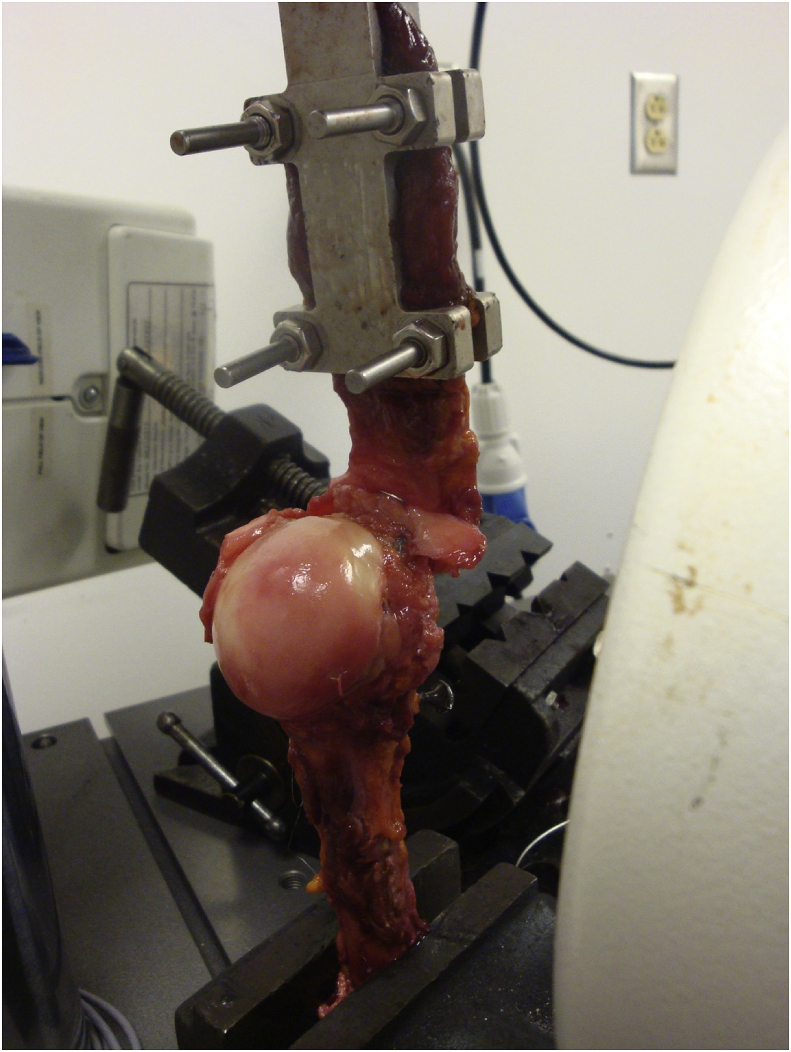
Fig. 2.

Medial-row knotted double row repair spanning the artificial cut.
Samples were secured on a material testing machine (Instron E3000 – Instron Corp., Norwood, MA) using a variable angle vice, oriented such that the direction of pull was 45° to the long axis of the humerus to mimic the physiologic pull of the superior rotator cuff.6 The muscle belly of the supraspinatus was secured to a clamp.
Two DVRT sensors were attached between the humerus (at the insertion point of the supraspinatus on the supraspinatus footprint) and 3 mm above the repair site and were used to measure the displacement of the repair during cycling. To augment and ensure reproducibility, a 1 mm metal bead was implanted in the humerus and a radio-opaque surgical staple was secured to the soft tissue 3 mm above the repair site (Fig. 3). Relative motion between the staple and bead was monitored and video captured via a FluoroScan Premiere Mini C-arm. Kinovea software was used for video analysis of gap formation. Kinovea has a resolution of 0.2 mm.
Fig. 3.
Samples were secured on a material testing machine (Instron E3000 – Instron Corp., Norwood, MA) using a variable angle vice, oriented such that the direction of pull was 45° to the long axis of the humerus to replicate the physiologic pull of the rotator cuff superiorly. The muscle belly of the supraspinatus was secured to a clamp. To augment and ensure reproducibility, a 1 mm metal bead was implanted in the humerus and a radio-opaque surgical staple was secured to the soft tissue 3 mm above the repair site.
Specimens were loaded in a similar fashion to previously described protocol.1 A 10 N preload was applied, at which time the DVRT’s were implanted, followed by the cycling protocol from 10 to 100 N for 200 cycles at 0.5 Hz. Failure during static testing was defined as displacement of 5 mm. Initial failure was defined as 0.5 mm on preload. Stiffness was calculated from the load/displacement curves as well as any construct creep that occurred during the 200 cycles. After cycling, ultimate load to failure was performed at 33 mm/min.
Values were reported as means and standard deviations. Differences between the two interventions were assessed using a Paired Students t-test. Significance was set at p < 0.05.
4. Results
Data included cyclic and failure data (Table 2). All data from paired specimens were compared using paired Student t tests. No statistically significant difference in total displacement across the repair between the two DVRT sensors over the 200 cycles of the test was noted between the two groups (Tied = 0.591 ± 0.501 mm; Not Tied = 0.439 ± 0.417 mm, p = 0.618). No statistically significant difference in stiffness was noted between the two groups (Tied = 32.87 ± 6.31 N/mm; Not Tied = 27.98 ± 9.69 N/mm, p = 0.120). No difference in ultimate load to failure was noted between the two groups (Tied = 501.2 ± 126.1 N; Not Tied = 416.8 ± 120.0 N, p = 0.116).
Table 2.
Cyclic loading results.
| Cyclic Displacement (mm) |
Stiffness (N/mm) |
Ultimate Load to Failure (N) |
||||
|---|---|---|---|---|---|---|
| MK | NK | MK | NK | MK | NK | |
| Cadaver No. | ||||||
| 1 | 1.121 | 0.203 | 34.8 | 40.2 | 466.4 | 272.6 |
| 2 | 0.860 | 0.379 | 30.8 | 27.1 | 305.2 | 373.3 |
| 3 | 0.179 | 0.003 | 41.6 | 38.5 | 636.7 | 437.4 |
| 4 | 0.231 | 0.217 | 29.4 | 16.6 | 510.4 | 509.3 |
| 5 | 0.028 | 1.154 | 36.9 | 26.3 | 638.3 | 591.2 |
| 6 | 1.126 | 0.681 | 23.6 | 19.2 | 449.9 | 317.3 |
| Overall mean | 0.591 | 0.439 | 32.87 | 27.98 | 501.2 | 416.8 |
| Overall SD | 0.501 | 0.417 | 6.31 | 9.69 | 126.1 | 120.0 |
Abbreviations: MK, Medial-row Knotted; NK, Not-Knotted.
5. Discussion
Our study demonstrated no significant difference in medial row fixation point displacement, construct stiffness, and ultimate load to failure between tying and not tying medial anchor fiberwire sutures in a transosseous-equivalent double row rotator cuff repair using FiberTape. Several biomechanical studies have demonstrated conflicting results with knotted and knotless fixation of the medial row in the setting of double row repairs.23,24,26, 27, 28, 29, 30 The study methods between each of these studies differ making it difficult to make conclusions on which construct is more superior biomechanically than another. The different variables in the study methods that could potentially affect outcomes are whether the specimens were tested with cyclic or progressive loading, the amount of cycles, the rate of loading, the amount of force used, the type of suture material and construct configuration. The current study used a validated biomechanical protocol described by Burkhart et al.1
Mall et al. performed a systematic review on the biomechanical importance of tying medial row knots and concluded that ultimate load to failure, stiffness, gap formation, and contact area were all significantly improved when medial knots were tied compared to knotless constructs.24 However, most of the studies in the systematic review used No. 2 Fiberwire and not a wider suture-tape for their repair construct. In 2017, Liu et al. studied footprint contact pressure and load to failure in sixteen ovine shoulders using a knotless medial row double-row suture construct comparing No. 2 FiberWire versus FiberTape. The FiberTape repair provided a three-fold increase in footprint contact pressure and a 1.5-fold increase in construct strength compared with the No.2 FiberWire.21
Werner et al. performed a biomechanical study comparing knotless versus knotted medial row double-row suture tape constructs in harvested bovine specimens (10 knotless specimens and 5 knotted specimens). After 200 cycles at 180 N the knotless group had the highest gap formation of 6.1 ± 2.2 mm and also had the highest failures with 70% (7 of 10) specimens not reaching 200 cycles due to suture cutting through tendons. The knotted group had the lowest gap formations and had no failures at 200 cycles. The study failed to report the numerical mean value for the knotted medial row gap formation, but rather displayed the mean on a box plot, which we estimated to be between 2 and 3 mm with less than 1 mm SD. The authors concluded that the knotted medial row group had superior cyclic biomechanical properties regarding initial construct stability compared to the knotless group.26
Pauly et al. compared a medial row knotted construct with knotless fixation (single tendon perforation and double tendon perforation) using a double row suture bridging technique with porcine fresh-frozen shoulders and found that medial row augmentation with medial horizontal mattress stitch reinforcement improved both maximum loads to failure and force resistance to 3 and 5 mm gap formations (338 ± 90.0 N and 77.8 ± 18.6 N, respectively) compared with single and double tendon perforation knotless medial row double row constructs (122.2 ± 33.8 N, 62.2 ± 6.7 N and 228.3 ± 99.9 N, 60.0 ± 0 N, respectively). It demonstrated a nearly tripled load to failure when compared with the single tendon perforation knotless medial row repair.29 Of note, the medial row knotted technique in this study used separate tendon perforations for each suture-tape limb and incorporated the #2 Fiberwire strands from the medial knots into the lateral rows. This study demonstrates that of the knotless medial row constructs, double tendon perforation improves biomechanical stability compared to single tendon perforation and that the medial row knotted construct is biomechanically superior to both single and double tendon perforation knotless medial row repairs.
Park et al. recently performed a biomechanical cadaveric study comparing medial row knotted versus knotless double row constructs using suture-tape and compared each fixation method in regard to self-reinforcement. The self-reinforcement parameters measured included contact area, contact force, and contact pressure at different shoulder abduction angles with progression loading up to 60 N and concluded that the medial row knotless suture-tape double row constructs had significantly higher self-reinforcement than the knotted repair, without diminishing footprint contact. The knotted medial row was thought to inhibit self-reinforcement resulting in stress-shielding of the lateral tendon.27
Although there are conflicting results with biomechanical studies comparing knotless and knotted medial row constructs, clinically, these results may not be as significant. Millet et al. evaluated their outcomes in 137 shoulders comparing a knotted No.2 fiberwire suture bridging construct with a knotless suture-tape bridging construct. They concluded that the use of either construct led to excellent outcomes at a minimum of 2 years follow up. They also obtained post-operative MRIs on 52 of 121 eligible shoulders (those that did not undergo revision shoulder surgery) at a mean of 4.4 years postoperatively and demonstrated that knotted medial row fixation were significantly more likely to have an full-thickness rotator cuff re-tear diagnosed by MRI (p < 0.041), however, the MRI follow up in the knotted medial row shoulders were performed further out from surgery (5.9, SD 1.3 years) compared to the knotless suture tape repair (3.9, SD 1.0 years).31
Our current study also evaluated the mode of failure of each testing construct. Our data, shown in Table 1, demonstrate similar results to Barber et al.’s study3 with the majority of failures in the medial knotted group being due to sutures tearing through the tendon. (67% versus 78%, respectively).
Table 1.
Cadaver demographics and mode of failure.
| Cadaver No | Age | Sex | Mode of Failure for Knotless | Mode of failure for Knotted |
|---|---|---|---|---|
| 1 | 55 | F | Tendon tore | Sutures tore through tendon |
| 2 | 55 | F | Screw Failure | Sutures tore through tendon |
| 3 | 32 | F | Tissue failure + screw came out (after) | Tissue failure |
| 4 | 58 | M | Sutures tore through tendon | Sutures tore through tendon |
| 5 | 51 | M | Sutures tore through tendon | Sutures tore through tendon |
| 6 | 57 | M | Tendon tore (10% posterior tear pre-test) | Screw came out (50% posterior tearpre-test) |
The mean age was 51 ± 8.9 years.
6. Limitations
This study is not without its limitations. Biomechanical cadaveric studies cannot replicate in vivo human tissue, so care must be taken when interpreting results. The use of matched pairs, however, may minimize the variability in tissue quality between test and control groups. In addition, though cyclic loading was performed, the effects of tissue healing cannot be inferred, therefore the results can only be interpreted for time-zero.
7. Conclusion
No significant difference was observed in medial row fixation point displacement, construct stiffness, and ultimate load to failure between tying and not tying medial anchor fiberwire sutures in a transosseous-equivalent double-row rotator cuff repair using FiberTape.
Acknowledgements
The authors thank the University of Miami Center for Orthopaedic Research and Education (CORE) for funding and Arthrex (Naples, FL) for providing the implants.
References
- 1.Burkhart S.S., Denard P.J., Konicek J., Hanypsiak B.T. Biomechanical validation of load-sharing rip-stop fixation for the repair of tissue-deficient rotator cuff tears. Am J Sports Med. 2014;42(2):457–462. doi: 10.1177/0363546513516602. [DOI] [PubMed] [Google Scholar]
- 2.Vaishnav S., Millett P.J. Arthroscopic rotator cuff repair: scientific rationale, surgical technique, and early clinical and functional results of a knotless self-reinforcing double-row rotator cuff repair system. J Shoulder Elbow Surg. 2010;19(2):83–90. doi: 10.1016/j.jse.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 3.Barber F.A., Drew O.R. A biomechanical comparison of tendon-bone interface motion and cyclic loading between single-row, triple-loaded cuff repairs and double-row, suture-tape cuff repairs using biocomposite anchors. Arthrosc J Arthrosc Relat Surg. 2012;28(9):1197–1205. doi: 10.1016/j.arthro.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Denard P.J., Jiwani A.Z., Lädermann A., Burkhart S.S. Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthrosc J Arthrosc Relat Surg. 2012;28(7):909–915. doi: 10.1016/j.arthro.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Frank J.B., ElAttrache N.S., Dines J.S., Blackburn A., Crues J., Tibone J.E. Repair site integrity after arthroscopic transosseous-equivalent suture-bridge rotator cuff repair. Am J Sports Med. 2008;36(8):1496–1503. doi: 10.1177/0363546507313574. [DOI] [PubMed] [Google Scholar]
- 6.Ma C.B., Comerford L., Wilson J., Puttlitz C.M. Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg Am. 2006;88(2):403–410. doi: 10.2106/JBJS.D.02887. [DOI] [PubMed] [Google Scholar]
- 7.Mazzocca A.D., Millett P.J., Guanche C.A., Santangelo S.A., Arciero R.A. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33(12):1861–1868. doi: 10.1177/0363546505279575. [DOI] [PubMed] [Google Scholar]
- 8.Millett P.J., Warth R.J., Dornan G.J., Lee J.T., Spiegl U.J. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23(4):586–597. doi: 10.1016/j.jse.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Sugaya H., Maeda K., Matsuki K., Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89(5):953–960. doi: 10.2106/JBJS.F.00512. [DOI] [PubMed] [Google Scholar]
- 10.Trantalis J.N., Boorman R.S., Pletsch K., Lo I.K. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthrosc J Arthrosc Relat Surg. 2008;24(6):727–731. doi: 10.1016/j.arthro.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 11.Burkhart S.S., Adams C.R., Burkhart S.S., Schoolfield J.D. A biomechanical comparison of 2 techniques of footprint reconstruction for rotator cuff repair: the SwiveLock-FiberChain construct versus standard double-row repair. Arthrosc J Arthrosc Relat Surg. 2009;25(3):274–281. doi: 10.1016/j.arthro.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Millett P.J., Mazzocca A., Guanche C.A. Mattress double anchor footprint repair: a novel, arthroscopic rotator cuff repair technique. Arthrosc J Arthrosc Relat Surg. 2004;20(8):875–879. doi: 10.1016/j.arthro.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Park M.C., ElAttrache N.S., Tibone J.E., Ahmad C.S., Jun B., Lee T.Q. Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16(4):461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Park M.C., Tibone J.E., ElAttrache N.S., Ahmad C.S., Jun B., Lee T.Q. Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16(4):469–476. doi: 10.1016/j.jse.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Warth R.J., Greenspoon J.A., Bhatia S., Millett P.J. Arthroscopic double-row rotator cuff repair using a knotless, interconnected technique. Operat Tech Orthop. 2015;25(1):43–48. [Google Scholar]
- 16.Cho N.S., Lee B.G., Rhee Y.G. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Sports Med. 2011;39(10):2108–2116. doi: 10.1177/0363546510397171. [DOI] [PubMed] [Google Scholar]
- 17.Cho N.S., Yi J.W., Lee B.G., Rhee Y.G. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010;38(4):664–671. doi: 10.1177/0363546509350081. [DOI] [PubMed] [Google Scholar]
- 18.Rhee Y.G., Cho N.S., Parke C.S. Arthroscopic rotator cuff repair using modified mason-allen medial row stitch: knotless versus knot-tying suture bridge technique. Am J Sports Med. 2012;40(11):2440–2447. doi: 10.1177/0363546512459170. [DOI] [PubMed] [Google Scholar]
- 19.Voigt C., Bosse C., Vosshenrich R., Schulz A.P., Lill H. Arthroscopic supraspinatus tendon repair with suture-bridging technique: functional outcome and magnetic resonance imaging. Am J Sports Med. 2010;38(5):983–991. doi: 10.1177/0363546509359063. [DOI] [PubMed] [Google Scholar]
- 20.Yamakado K., Katsuo S., Mizuno K., Arakawa H., Hayashi S. Medial-row failure after arthroscopic double-row rotator cuff repair. Arthrosc J Arthrosc Relat Surg. 2010;26(3):430–435. doi: 10.1016/j.arthro.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 21.Liu R.W., Lam P.H., Shepherd H.M., Murrell G.A.C. Tape versus suture in arthroscopic rotator cuff repair: biomechanical analysis and assessment of failure rates at 6 months. Orthop J Sports Med. 2017;5(4):1–7. doi: 10.1177/2325967117701212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mook W.R., Greenspoon J.A., Millett P.J. Arthroscopic double-row transosseous equivalent rotator cuff repair with a knotless self-reinforcing technique. Open Orthop J. 2016;10:286–295. doi: 10.2174/1874325001610010286. Suppl 1: M4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Busfield B.T., Glousman R.E., McGarry M.H., Tibone J.E., Lee T.Q. A biomechanical comparison of 2 technical variations of double-row rotator cuff fixation: the importance of medial row knots. Am J Sports Med. 2008;36(5):901–906. doi: 10.1177/0363546507312640. [DOI] [PubMed] [Google Scholar]
- 24.Mall N.A., Lee A.S., Chahal J. Transosseous-equivalent rotator cuff repair: a systematic review on the biomechanical importance of tying the medial row. Arthrosc J Arthrosc Relat Surg. 2013;29(2):377–386. doi: 10.1016/j.arthro.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 25.Park M.C., Peterson A., Patton J., McGarry M.H., Park C.J., Lee T.Q. Biomechanical effects of a 2 suture-pass medial inter-implant mattress on transosseous-equivalent rotator cuff repair and considerations for a “technical efficiency ratio”. J Shoulder Elbow Surg. 2014;23(3):361–368. doi: 10.1016/j.jse.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 26.Werner A., Heuberer P.R., Laky B., Kriegleder B., Reihsner R., Eberhardsteiner J. Superiority of bridging techniques with medial fixation on initial strength. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2559–2566. doi: 10.1007/s00167-012-1922-9. [DOI] [PubMed] [Google Scholar]
- 27.Park M.C., Peterson A.B., McGarry M.H., Park C.J., Lee T.Q. Knotless transosseous-equivalent rotator cuff repair improves biomechanical self-reinforcement without diminishing footprint contact compared with medial knotted repair. Arthrosc J Arthrosc Relat Surg. 2017;33(8):1473–1481. doi: 10.1016/j.arthro.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 28.Leek B.T., Robertson C., Mahar A., Pedowitz R.A. Comparison of mechanical stability in double-row rotator cuff repairs between a knotless transtendon construct versus the addition of medial knots. Arthroscopy. 2010;26:S127–S133. doi: 10.1016/j.arthro.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 29.Pauly S., Fiebig D., Kieser B., Albrecht B., Schill A., Scheibel M. Biomechanical comparison of four double-row speed-bridging rotator cuff repair techniques with or without medial or lateral row enhancement. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2090–2097. doi: 10.1007/s00167-011-1517-x. [DOI] [PubMed] [Google Scholar]
- 30.Smith G.C.S., Bouwmeester T.M., Lam P.H. Knotless double-row SutureBridge rotator cuff repairs have improved self-reinforcement compared with double-row SutureBridge repairs with tied medial knots: a biomechanical study using an ovine model. J Shoulder Elbow Surg. 2017;26(12):2206–2212. doi: 10.1016/j.jse.2017.06.045. [DOI] [PubMed] [Google Scholar]
- 31.Millett P.J., Espinoza C., Horan M.P. Predictors of outcomes after arthroscopic transosseous equivalent rotator cuff repair in 155 cases: a propensity score weighted analysis of knotted and knotless self-reinforcing repair techniques at a minimum of 2 years. Arch Orthop Trauma Surg. 2017;137(10):1399–1408. doi: 10.1007/s00402-017-2750-7. [DOI] [PubMed] [Google Scholar]