Abstract
Open patellar stabilization surgeries carry a risk of knee stiffness, patello femoral pain, longer time for recovery and poor cosmesis. We describe an arthroscopic assisted minimally invasive technique for patella maltracking which can help eliminate these complications.
Keywords: Patella stabilization, Medial reefing, Arthroscopy, Lateral release, Minimally invasive, Medial patellofemoral ligament
Patellar maltracking and instability are debilitating disorders of the knee. The medial patellofemoral ligament and lateral retinaculum are the primary cause of instability.1, 2 We describe an arthroscopic technique of patellar stabilization by medial retinaculum imbrication and lateral release.
Lateral retinacular release is performed arthroscopically with Sabre 30 (Arthrocare) through a lateral portal followed by medial patellofemoral reefing. Patella is marked and a stab incision is carried out medial to the superior and inferior medial border of the patella (Fig. 1A). A Mayo needle with non absorbable suture (Ethibond 1–0, D 9464, Ethicon US) is passed from just medial to patellar medial border through the medial retinaculum to around 5 cm medial to patellar medial border under direct arthroscopic vision (Fig. 1B and C). Care should be taken to avoid trapping the saphenous nerve and long saphenous vein which are pre marked (Fig. 1A). The both sides of free end of the suture is passed subcutaneously into the midpoint incision (Fig. 1D) and ends tied into a knot (Fig. 1E). This step is repeated again with another incision below the first one (Fig. 2). This results in reefing of the medial retinaculum as it folds on itself medializing the patella. This surgical technique relies on nonabsorbable ethibond to maintain the imbricated fold of retinaculum, as it doesn’t depend on the scarring of the retinaculum.
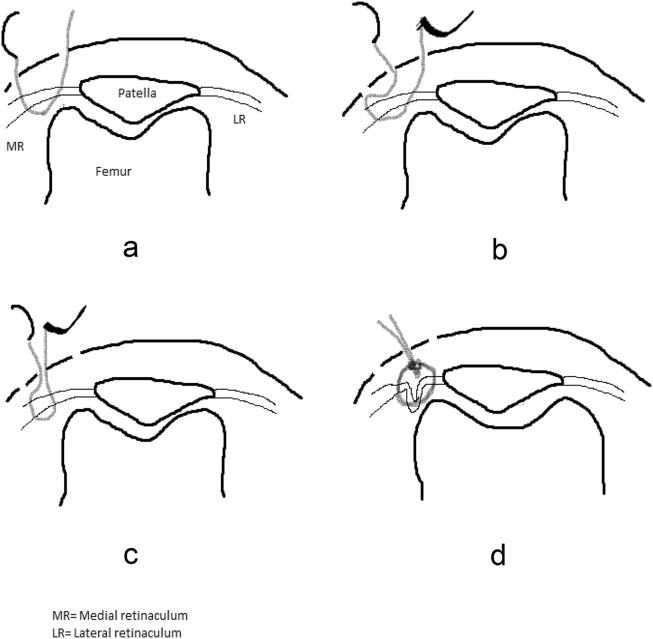
Fig. 1.
(a) The three incisions (A,B and C) are made lateral to the course of the saphenous nerve and long saphenous vein. (b) Ethibond is passed from A to B extrasynovially (confirmed through the scope). (c) The Ethibond needle is extracted from B and then passed from B to C subcutaneously. (d) Free end of suture is passed subcutaneously from A to C using Mayo needle and tied. (e) Skin is closed.
Fig. 2.
(a) Ethibond is passed extra-synovially superomedial to the patella and exited 5 cm medial to its entry. (b) Ethibond is then passed subcutaneously and exited through an incision midline between the two incisions. (c) The free end of the suture is inserted into a Mayo needle and passed subcutaneously through an incision between the first two incisions. (d) Both ends of the suture are tied and cut.
1. Discussion
In recent years, many arthroscopic techniques have been developed for lateral release and medial imbrication. It has gained popularity due to cosmetic advantages. A study conducted by Haspl et al. concluded good results with fully arthroscopic lateral release and medial plication.2 Clinically we noticed Kujala score improved to 94, compared to 64 preoperatively (p < 0.05) and also the mean Lysholm score improved to 78, compared to 51 preoperatively (p < 0.05). Radiologically congruence angle, lateral patellar displacement and lateral patellofemoral angle showed significant improvement post-operatively. This procedure is effective, does not require any special instruments and is technically simple.
Disclaimer
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Specific national laws have been observed.
Declaration of competing interest
The authors of this paper certify that they have no affiliations with or involvement in any organization or entity with any financial interest such as honoraria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership or any other non-financial interest in the subject matter or materials discussed in this manuscript.
References
- 1.Shah Kalpit N. Lateral patellofemoral ligament: an anatomic study. Orthop J Sports Med. 4 Dec. 2017;5:12. doi: 10.1177/2325967117741439. 2325967117741439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haspl M., Cicak N., Klobucar H., Pecina M. Fully Arthroscopic stabilization of the patella. Arthroscopy. 2002;18:1–3. doi: 10.1053/jars.2002.30023. [DOI] [PubMed] [Google Scholar]